FIXED PROSTHETICS
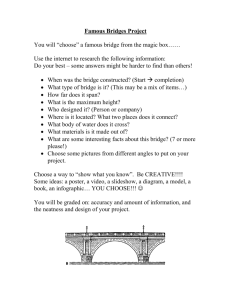
advertisement

FIXED PROSTHETICS 1. In the appointment for bridge preparation, what else do you do in the same appointment? Take an impression of the unprepared teeth or of the wax up in a silicone putty or alginate and save it for later. Before making the preparation, replace or adjust any damaged restoration. LA, Make the preparation, check parallelism, place retraction cords impregnated with epinephrine or aluminium chloride solution, and take impressions using an elastomeric material, make an occlusal registration (blue-mousse or jet bite). Make the temporary bridge using the impression taken before of the wax up or unprepared teeth, use a bis – acryl resin (luxatemp) and seat it over the preparation. After initial set, remove it, let it finish curing, trim it, polish it and cement it with temporary cement (temp bond). Take the shade, make the lab sheet and send it off and give another appointment to the patient. 2. How do you prepare a temporary bridge? Using a good alginate impression material or PVS putty of the unprepared teeth, place Bis acryl composite resin material such as luxatemp or protemp. Place it on the prepared teeth, when the initial set has been reached the impression is removed and the provisional left to finish curing, remove it, trim it, check occlusion and polish it. It can also be done with an over-impression taken of the diagnostic cast (diagnostic waxing). Placing resin in the over-impression and then seating the cast into the over-impression. After it has cured it is removed and trimmed, the occlusion adjusted and polished (useful for multiple crowns). Prefabricated provisional restorations can be use as well (prefabricated polycarbonate crowns, preformed anatomic metal crown). These can be trimmed to fit, lined with resin and joined together. 3. How is it prepared in the lab? Advisable if preparing multiple crowns or if temporary crown needs to last for several months, preferred for its accuracy, protection to the pulp. By taking an over-impression on the diagnostic cast (diagnostic waxing). An acrylic template can also be used, shaped on a diagnostic cast, using a vacuum forming machine. Then, filled with resin and after it has finish curing, the provisional is removed, trimmed and polished. Any defects on the tooth should be filled and smooth over with red utility wax, before the over-impression is taken. The provisional is relined and adjusted at the chairside. 4. Why would not let the acrylic completely cure in the mouth? (at least 2 reasons) It may bind in the undercuts and be impossible to remove. It may cause a thermal injury from the exothermic setting reaction (poly-n-butyl methacrylate), a chemical injury from the presence of free monomer, and mechanical injury caused by volume changes or pressure arising from polimeratization shrinkage. Neither poly methyl methacrylate PMMA, nor poly ethyl methacrylate PEMA, are considered strong enough these days for provisional bridge construction. They Have been replaced by the use of Bis GMA composite resin material such as Protemp or Luxatemp. 5. What characteristics would you be looking for when choosing an impression material? Accuracy, long term dimensional stability, use characteristics (handling properties), taste or smell, elastic recovery, tear resistance, hydrophilicity (wettability), bond to tray, cost. 6. What would you do in the next appointment? Try in stage: If porcelain fused to metal bridge is being constructed it is advisable to try in the metal work before the porcelain is added to it. The fit of the metal framework is evaluated and the occlusion adjusted. Check contacts, proximal, centric and excursive-lateral and protrusive. If ceramic crowns, use try in paste to hydrate the porcelain, protecting it from breaking, check marginal fit, contact points, and occlusion, if any adjustments are required polish with porcelain polishing wheels. Make sure patient is happy before you cement the crown. 7. Would you try the metal framework with the biscuit bake or only the metal framework and why? Only for big cases to try aesthetics, speech, length, seating on the lip. If you only try the biscuit bake you wont be able to see the metal framework. You try both with the metal framework you check the margins and with the biscuit bake occlusion. 8. What do you do when first trying the metal framework and it does not seat? The bridge can be sectioned, and hopefully both retainers will then seat. The two parts are then secured in the new position with acrylic resin (duralay) and sent back to the lab to be soldered. Or take a new impression and secure good provisional to make sure teeth stay stable. Make sure of good contacts. 9. What are the possible reasons for that? This can occur if there has been some minor movement of the abutments since the impression was taken. 10. What could have gone wrong if the metal framework is perfect on the dies but only seats in one abutment in the mouth? (give at least 2 reasons) Temporary cement left in the preparation, too tight proximal contacts, distorted impression, die over trimmed leading to over extension of margin, movement of the abutments. 11. What cement do you use to porcelain fused to metal bridge and why? Any is good, Zinc phosphate (standard and has been extremely successful, disadvantages is solubility in oral fluids and lack of adhesion), Polycarboxylate (week chemical bond to dentin, undergo plastic deformation after loading, less retentive than Zinc phosphate and GI cements), GI (weak chemical bond to dentin, release fluoride), resin modified glass ionomer cements (release fluoride, are insoluble and provide better retention, imbibes water and expands with time), resin cements (greater retention, care with eugenol contamination of dentin, difficulty in manipulating). I will choose GI cement. They are easy to handle, may be polished after light curing, good aesthetic, fluoride release, improve mechanical strength. 12. What is your favourite brand name? Fuji (plus), encapsulated system ensure optimal mixing and allow placement via syringe tip 13. What would it be your second option and why? Zinc phosphate because has been the traditional cement to lute dental restorations and has been extremely successful, has good strength properties. 14. What causes postoperative sensitivity and what is the management? Over reduction, overheating while preparing, chemical reaction of provisional cement, bacterial contamination of the pulp, exposure, high contact. Postpone cementation of the crown, make sure the provisional restoration is not in hyperocclusion and it covers all prepared tooth surfaces, recement for several days. If pulpitis persists, endodontic therapy will be necessary before the permanent restoration can be cemented. Never cement a crown permanently over a symptomatic tooth. 15. Bridge 13-11: All the procedure from case selection to cementation, follow up? Take a history. Clinical exam (extra oral-sings TMJ dysfunction and intraoral-oral hygiene, periodontal condition, general condition, length edentulous span, condition and position abutments, occlusion).Radiographs, diagnostic mounting in ICP. Diagnostic waxing. Treatment planning. Before tooth preparation, remove caries, place core and post. Preparations. Soft tissue management. Impressions. Occlusal registration. Temporary bridge. Metal work try in. Trial cementation(if any further adjustments need to be done). Instructions of how to clean the bridge. Permanent cementation. Adjust contacts and polish. Follow up (to check if bridge still functioning satisfactory, check fit, contacts, comfort and sensitivity, gingival response). Maintenance. 16. In which case a wax up is not needed When the destruction of the teeth is minimal, when the occlusion is not a problem, in anterior when a denture tooth can be use for the same purpose (simulation of final restoration and occlusion). When it is straight forward, easy case. When the shape is not going to change or when aesthetic is not an issue for a posterior tooth. 17. Gingival tissue management? Horizontal and vertical displacement? Why is horizontal displacement required? How would you retract the gingiva prior to taking the impression for the fabrication of a bridge? Gingival retraction is performed to decrease gingival exudates’ and expose sub gingival preparation prior to polishing the margins and impression taking. Impregnating the retraction cord in substances such as adrenaline-8% epinephrine (could induce cardiac reactions), ferric sulphate (kinder to the gingival tissue) or aluminium chloride to decrease bleeding. The cord should be gently placed into the gingival crevice with a flat plastic or cord packer prior to impression taking and temporization. Placement of retraction cord prior to tooth reduction around the cervical area, results in minimal damage to the gingival complex. The cord shields the soft tissues from the bur. A retraction material such as Expasyl can be used as well to access the cervical margins. It is the only sulcus opening method that guarantees the integrity of the epithelial attachment, unlike the double cord technique. No anaesthesia required. Electrosurgery may be indicated where a margin extends subgingivally and gingival overgrowth is hampering restoration placement or impression taking. 18. Case of patient with severe pain in third quadrant, wear facets, no dental problems, stressful job. Differential diagnosis, other tests needed for diagnosis, definitive diagnosis and treatment plan? More x rays (PA, OPG), vitality test, check for fractures, check occlusion, Palpate muscles. It could be crack tooth syndrome, referred pain, cyst or tumour. It can also be grinding or clenching teeth (Bruxism), TMJ problems, muscular spasm. Stress management, local heat on face (heat packs), occlusal splint to protect teeth. 19. What is bilateral balanced occlusion? Balancing contacts in all excursions of the mandible to increase stability of full dentures. Not applicable to natural dentition. 20. Preparation of 21 and 23 for full coverage PFM bridge. Impression material that I would choose and reason? What records are to be sent to the lab? What type of occlusion would be ideal for this case, would be better canine guidance or group functions, why? Elastomers, addition cured silicone preferred because are very stable. Lab sheet wit explanation, date to be return, impression in silicone of upper arch, impression in alginate or cast of lower arch, occlusal registration, shade. Group function occlusion because multiple tooth contact and the load wont be only in the canine. I think, as it is already supporting the bridge. 21. Prepare 12, 11 CR veneer, tetracycline staining, CR bonding to enamel and dentine, dentin exposed during prep, thickness, finishing line, traumatic occlusion, porcelain veneer? Tetracycline staining (mild discoloration) is an indication for porcelain veneer. Avoid in edge to edge occlusion. There should ideally be enamel around the entire periphery, which is necessary for adhesion and seal the veneer to the surface. There should be enough available enamel for bonding, because bonding in dentin is not as reliable as enamel bonding. Veneers are usually 0.5-0.7 mm thick, 0.3 for small teeth. The finish line should be a chamfer. If the tooth is discoloured the margin should be subgingival (but still in enamel), otherwise keep it slightly supragingival (right at the gingival margin). Porcelain veneers have better performance aesthetics than resin composite. Porcelain is less plaque retentive. 22. Types of impressions techniques? Monophase (polyeter) The same mix of regular viscosity material is used for both a stock tray and syringe. Double mix technique (polysulfite, addition cured silicone) a single stage technique necessitating the mixing of heavy and light body materials at the same time, and use of a special or stock tray. Apply adhesive to the tray, mix heavy and light body for 45-60 seconds, remove retraction cord or leave it in place and dry preparation. Apply light body mix around preparation and gently stream air to direct material into crevice. Position tray containing heavy bodied material, support the tray with light pressure until 2 min after apparent set. Putty and wash technique (silicone). The putty and light body can be used with a stock tray, either single stage (as described above) or two stage. 23. Implants. 65 years patient advice for implant? Explain about osteoporosis. Implants are based on the concept of osseointegration. Made of titanium or hydroxyapatite coated titanium. Indicated in edentulous mouth unable to retain dentures, partially dentate for bridges abutments, single anterior tooth replacement, and maxillofacial prostheses post cancer surgery or trauma. Good oral hygiene is mandatory. Joint planning between oral surgeon and restorative dentist is essential for success. It is performed by raising a mucosal flap and preparing a channel in bone, using matched spiral drills. The entrance is counter sunk and then it is either pressed into place or screwed in. In two stage procedure the implant is covered by the flap at the end of the procedure and left to heal for 4 to 6 months. After healing; excision of the mucosa overlying the implants is performed and insertion of the abutments. Prosthetic procedures can start after two weeks. I one stage procedure, insertion of the abutment at the end of implant placement. Age is not a major impactor. Osteoporosis can be a risk factor for implant not to work, as well as diabetes, smokers and patients taking Bio- phosphates (fosamas); calcium related medicament-danger osteonecrosis. This medicament is given to people with osteoporosis to stop the metabolism of the bone. 24. What is benefit of condylar guidance ????Reproducing (simulates) the real mandibular movements on the articulator, which minimize the amount of time spent adjusting the restoration at the try in stage and allows changes to the patient’ occlusion to be planned. This question should be about anterior guidance, in that case it protects the posterior tooth in protrusive movements. If adjustable articulator, you could program it to help you achieve the anterior guidance. 25. What would happen if there is uneven thickness of metal coping? The metal will show through the crown or there will be over contouring in some areas restoration (either opaque or over contoured). It could have deficient strength, deficient margins, and induce casting errors. 26. Is the upper lateral incisor an adequate abutment for a missing upper canine? The upper lateral incisor has the poorest amount of support and retention. If a canine is to be replaced with a bridge the occlusal scheme should be designed to provide group function in lateral excursions. The two premolars and lateral can be use as abutments. 27. What do you understand by the concept of biological width? It extends approximately 2 mm from the bottom of the gingival sulcus to the alveolar crest. 1 mm is junctional epithelium and 1 mm is connective tissue. A 3 mm distance is recommended between the finish line of the preparation or final margin of a restoration and the alveolar bone. 28. If the patient presents with a lost upper anterior as an emergency. What are the treatment options that you have to offer? Direct bonded resin bridge, temporary denture. Depending on the patient urgency, the time. 29. How would you manage gingival bleeding prior to taking impressions? Astringent, retraction cord, electrosurgery, TCA. 30. What is the best material to make impressions for crown and bridge? Why? Polyvinyl siloxane (PVS) or addition reaction silicone. It has good physical properties: Accuracy unsurpassed, can record fine detail, best elastic recovery, dimensional stable and can be poured the convenience of the operator, permits second pour, handling properties very favourable, supplied in number of viscosities, clean, odourless and tasteless, minimal material specially in custom tray. Polyether as PVS are the most acceptable impression materials, have excellent accuracy, long term stability, less accurate after 2 weeks, poor taste, elastic recover good but not as good as PVS, good tear resistant, hydrophilic, less expensive. 31. What do you do if the patient is complaining of pain on the night after you cement the temporary bridge? Reassure the patient, explain the possible causes, and tell it could be an initial symptom. Make sure the temporary bridge is well cemented covering the margins, check occlusion; it could be a high contact. Keep in observation until symptoms disappear. 32. What do you do if you discover that during the preparation there was a pulp exposure? If traumatic exposure, small, and uncontaminated, perform direct pulp cap with hard setting calcium hydroxide and restore. If carious exposure, and continued pulp vitality is doubtful, RCT will be required. If time is short, can dress tooth with ledermix and a traditional GI cement, and extirpate pulp at next visit. 33. How can you improve the retention if you have a short crown? Crown lengthening, forced eruption, addition of grooves or boxes in the preparation. A minimum of 4.0 mm oclusocervical is necessary for molar preparations and 3.0 mm for premolar preparations. 34. Bennet movement, angle, how much? Bennet movement is the lateral shift of the mandible. Bennet angle is formed by the balancing condyle when moves down forward and inward with the median plane when projected perpendicularly on the horizontal plane.