subjective perception of hypersensitivity to chosen additives
advertisement

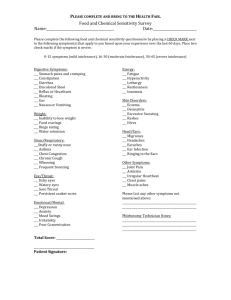
1 SUBJECTIVE PERCEPTION OF HYPERSENSITIVITY TO CHOSEN ADDITIVE-CONTAINING FOODS IN THE POPULATION OF CHILDREN AND YOUTH Ewa Zagórecka 1, Maciej Kaczmarski 2, Janina Piotrowska-Jastrzębska 1 Department of Propedeutics of Paediatrics, Medical Academy of Białystok Head: Janina Piotrowska – Jastrzębska, M.D., Ph.D. 2 III Department of Paediatrics, Medical Academy of Białystok Head: prof. Maciej Kaczmarski, M.D., Ph.D. 1 Adverse reactions to food constitute a significant problem, particularly in the population of developmental age. According to Chandra, at least 30% of people experience symptoms that indicate food intolerance once or more during their lifetime. Of all adverse reactions genuine food allergies constitute approximately 20 to 30-40%. The term is used to describe a syndrome of clinical symptoms (organic, systemic) appearing in the human organism after the ingestion of foods or food additives and due to abnormal immune response. More frequently, however, mechanisms other than immune are involved. The reactions are defined as non-immune hypersensitivity (food intolerance) and can result from harmful action of certain substances contained in food, such as toxins (poisoning) or active pharmacological compounds (tyramine, caffeine), or may be due to enzymatic, metabolic and other disorders. Determination of genuine incidence of adverse reactions to foods in the population, including food allergy, poses numerous problems. First of all, great discrepancy exists between subjective perception of adverse symptoms by adults or parents with respect to their children and clinical evidence of adverse reactions to foods. In British surveys, up to 20% of adult responders believed to have symptoms of food allergy, while blind challenge tests confirmed adverse reactions in 1.4%. Up to 28% of parents involved in a study conducted by Bock declared that their children had at least one event of adverse symptoms following food ingestion. However, the latest epidemiological data indicate that the frequency of reliably evidenced allergy to e.g. cow milk protein – being the most common in childhood – ranges between 1.8 and 4.4%. The incidence of adverse reactions to substances purposely added to food is even more difficult to determine. The so called food additives constitute a numerous group of chemical compounds varying in structure, physico-chemical features, biological and toxicological properties, origin and functions. Their use in food production, in pharmaceutical and cosmetic industries is determined by a number of factors. The major aim is to improve the quality of products and their sensory attractiveness or to ensure proper productive, technological and storing processes. Food additives admitted to use are safe for general population when used according to legal regulations. However, adverse reactions to food additives have been described in hypersensitive patients. The incidence of intolerance to substances purposely added to food is difficult to determine for a number of reasons, although according to Würthrich and other researchers it is considerably less common than is believed. The difficulties are due to the use of different diagnostic criteria (e.g. case history data, challenge tests), different selection and number of 2 patients, problems to identify individually harmful additives (type and dose of substances used in challenge tests) and many others. Pathogenetic mechanisms of adverse food reactions induced by additives have not been fully elucidated. IgE-dependent allergies, which can be confirmed in diagnostic tests (skin tests, allergen-specific IgE) – e.g. allergy to carmine dye, annato, aspartam or sulphites, constitute only a small part. Cases of intolerance (non-immune mechanisms) which can be diagnosed by means of the golden diagnostic standard i.e. double blind placebo-controlled test (DBPCFC) hold the majority. In future, the assessment of the secretion of sulfidoleukotriens by peripheral leukocytes isolated from patients and stimulated by food additives may be of certain help. This type of study has been recently conducted by Worm et al. (2001). According to the European Communites Scientific Committee for Food, adverse reactions to additives refer to 0.03-0.15% of the adult population. In a research conducted among adults in Denmark and England, the incidence of intolerance to food additives was found to be 0.010.23%. In the study of Young carried out on children and adults (c. 30,000 people) a total of 7.4% of responders associated different types of adverse symptoms with food additives. Eventually, verified by DBPCFC tests, the incidence was estimated at 0.026%. Adverse reactions to food additives are more likely to occur in the population of children than adults. This is indicated by Danish studies performed by Fuglsang et al. on 4,952 school children (5 - 16-year-olds) and in the group of 472 children with allergic diseases. Open challenge tests using mixtures of various additives were positive in 9.8% and 7%, while DBPCFC method revealed intolerance in 1% and 2% respectively. The authors emphasised the fact that adverse reactions to additional substances were much more common in allergic children. In Mexican studies carried out by Madrigala et al. hypersensitivity to substances added to food referred to 0.6% of children. In Poland, there are no epidemiological data concerning the incidence of intolerance to food additives among children. Therefore, the present study has been undertaken in the Białystok centre and will be conducted in stages. The aim of the first stage – already accomplished – was to determine the incidence of subjective perception of adverse symptoms following ingestion of particular foods rich in additives. The subsequent stages will involve verification of preliminary results, by e.g. open challenge and double blind placebo controlled tests. Questionnaire investigations conducted in autumn 2001 among parents of children and adolescents aged 6-16 years, attending randomly selected schools in Białystok and randomly chosen classes in these schools. The analysis included 5,044 properly and completely filled in questionnaires (74% returnability); Chi² independence test was used for statistical calculations, with significance levels defined as p<0.05. The group involved in the study consisted of 2,538 girls (50.3%) and 2,506 boys (49.7%); 23% were aged 6-8 years, 35.4% - 9-11 years and 41.6% - 12-16 years. According to parents, 14.6% (734) of children experienced different types of adverse symptoms following food ingestion, due to food allergy or intolerance. In this subgroup, 47.4% (348) were boys and 52.6% (386) girls. The incidence of adverse reactions to foods was statistically significantly correlated with age - symptoms of intolerance were more common in younger age groups compared to older children – p<0.05 (approximately 17-18% in 6-7-year-olds, 7% in 13-14-year-olds). 13% of the responding parents (664) stated that food allergy or intolerance was diagnosed by a physician (at present or in the past), the problem referring to 49% (320) of boys and 51% (328) of girls. Likewise, in the same group, the incidence of reported food allergy/intolerance was correlated with age (p<0.05), but not with sex. As reported by parents, of 5,044 inquired children 9.3% (467) were or still are on a diet with certain limitations or elimination of various products. 3 The analysis of the questionnaire data showed that 9,8% children (497) demonstrated subjective adverse symptoms after ingestion of certain products containing additives. This referred to 47.9% (238) of boys and 52.1% of girls (259) and was most frequently reported by parents of 6-9-year-olds (13-14%) and most rarely (5%) by parents of 14-15-year-olds. Statistical analysis showed a significant correlation with age (p<0.05), but not with sex. According to parents, adverse symptoms associated with intolerance of food additives were most common in children after the consumption of sparkling drinks like Coca-Cola or orangeade – 9% (458), sweets (chewing gum, sweets, crisps, cakes) – 6.64% (335), fast food and fruit – 4% (204}. The most common adverse symptoms due to the consumption of foods reported by parents as intolerated included: abdominal pain – 9.9% (503), cutaneous rash – 8.8% (446), cough and rhinitis – 5.5% (280) and 5.6% (282), and headaches – 4.9% (248). The incidence of symptoms from the skin (cutaneous rash, exacerbation of atopic dermatitis, urticaria), gastric disorders (abdominal pain, loose stools), cough, rhinitis, concentration disorders and hyperactivity was statistically significantly correlated with age – younger children reacted more frequently (p<0.05). No correlation with age was found in the case of such symptoms as itching of the skin, dyspnoea, headaches and systemic reactions. No statistically significant differences were also observed in the incidence of the above symptoms in relation to sex. In the subgroup of 497 (9.8%) patients with suspected hypersensitivity to foods rich in additives 63.4% (315) reacted with adverse symptoms following ingestion of various types of sparkling drinks, 48.9% (243) – sweets and 31.4% (156) - fast food. The incidence of adverse symptoms after ingestion of various types of spices was statistically significantly correlated with age (p<0.03) – being more common in older children. In the case of the other types of food no correlation with age or sex was revealed. The most common manifestations of food intolerance in this subgroup (497) included abdominal pain 61.8% (307), cutaneous rash 55.3% (275), rhinitis 38.8% (193), cough 38.2% (190), headaches 33.4% (166) and hyperactivity 29.2% (145). A statistically significant correlation with age was observed in the case of such symptoms as exacerbation of atopic dermatitis (p<0.03), cough (p<0.02), nausea/vomiting (p<0.01) – these symptoms were more frequent in younger age groups, and headaches (p<0.01) being more common in older children. No correlation with sex was found. Taking into consideration adverse symptoms after consumption of food additives in atopic or hypersensitive children, the cases well known from literature, the incidence of declared intolerance to additive-containing foods was compared between children with and without diagnosed food hypersensitivity (664 and 4,380, respectively). Statistically significant differences (p<0.001) were found for each information (type of food, clinical symptoms), with higher intolerance incidence in hypersensitive children. At the present stage of the study – elaboration of the questionnaires – we are not able to determine the genuine incidence of intolerance to food additives. The incidence of subjectively perceived intolerance to foods rich in additives was estimated at 9.8% - which, however, has to be verified. The knowledge of the real extent of the problem of adverse reactions to food additives and their diagnosis seems essential. It can clear the patients from suspicions and may prevent relating different ailments to imaginary intolerance. On the other hand, confirmed diagnosis will allow elimination of these substances, being the only suitable therapeutic management.