Which of the following antibiotics is NOT used for

Junior Pain Control
Final Examination
Summer 2004
Name:
Box #:
Read all questions very carefully! The answer sheet is the last page of this booklet.
1.
Which of the following antibiotics is NOT used for
SBE antibiotic prophylaxis?
A. Azithromycin
6.
Which are significant risk factors for perioperative
MI?
1. History of angina pectoris
B. Clarithromycin
C. Clidamicin
D. Erythromycin
2.
Which of the following statements about aspirin is
NOT true?
A. The typical dose is 325-650 mg q4h.
2. Ischemic changes on the EKG (ECG)
3. Previous MI
4. Age over 70
3.
B. An early sign of toxicity tinnitus.
C. The maximum daily dose is 3,200 mg.
D. A massive overdose can lead to uncoupling of oxidative phosphorylation.
Which of the following statement(s) about ibuprofen is/are NOT true?
1. Preliminary stidies have indiated that ibuprofen
A. 1, 2, 3
B. 1 and 3
C. 2 and 4
D. 4 only
E. All of the above
7.
What percent of all patients are successfully sedated by nitrous oxide at levels of 50% and below? (Hint:
How often would you expect to be successful by increasing the percentage to between 50-70% if the may block the beneficial effects of aspirin.
2. The amount of ibuprofen in a Vicoprofen tablet is
400 mg.
3. Ibuprofen is one of the most effective NSAID analgesics.
4. Ibuprofen irreversibly blocks platelet aggregation. patient is not satisfactorily sedated at 50%?).
A. 85%
B. 90%
C. 95% WILL NOT BE ON TEST
D. 99%
8.
Which cardiac valve is most commonly affected by rheumatic heart disease?
A. Aortic
B. Pulmonary
C. Tricuspid
D. Mitral
A. 1, 2, 3
B. 1 and 3
C. 2 and 4
D. 4 only
E. All of the above
4.
Which of the following statement(s) about opioids is/are not true?
1. Most opioids cause pupillary dilation.
2. There are no opioids combination drugs with aspirin.
3. Most of the analgesia is due to activity at the kappa receptor.
4. A side effect of opioids is nausea and vomiting.
9.
Unconsciousness in syncope results from:
A. Electrolyte imbalance
B. Neurogenic shock
C. Cerebral hyperemia
D. Cerebral hypoxia
10.
In the treatment of an acute anaphylactic reaction, the first drug that should be administered is:
A. Hydroxyzine
B. Epinephrine
C. Hydrocortisone
D. Diphenhydramine A. 1, 2, 3
B. 1 and 3
C. 2 and 4
D. 4 only
E. All of the above
5.
Which of the following is not indicated for the acute pain of multiple tooth extractions?
1. Rofecoxib (Vioxx)
2. Dexamethasone (Decadron)
3. Tramadol (Ultram)
4. Celecoxib (Celebrex)
11.
The selection of a vasoconstrictor for a local anesthetic depends upon
A. the duration of the procedure.
B. the need for hemostasis.
C. the medical status of the patient.
D. all the above.
12.
A patient that is allergic to pencillin and needs antibiotic prophylaxis is BEST treated with:
1. Amoxicillin
2. Cephalexin
A. 1, 2, 3
B. 1 and 3
C. 2 and 4
D. 4 only
E. All of the above
3. Doxycycline
4. Clindamycin
A. 1 and 3
B. 1, 2, 3
C. 2 and 4
D. 4 only
E. All the above
13.
Meperidine has a possible fatal interaction with which of the following medication classes?
A. Selective serotonin reuptake inhibitors
B. Monoamine oxidase inhibitors
C. Beta blockers
D. Macrolide antibiotics
14.
Which pair of anesthetics is most likely to show crossallergy?
A. Lidocaine-mepivacaine
B. Prilocaine-tetracaine
C. Procaine-mepivacaine
D. Procaine-lidocaine
E. Lidocaine-benzocaine
15.
The usual adult dosage of codeine administered orally is
A. 500-1000mg.
B. 250-500mg.
C. 30-60mg.
D. 2-5mg.
E. None of the above.
16.
In general, what is the amount of the SBE prophylaxis dose that is taken six hours after the first dose?
A. Double the initial dose.
B. The same as the initial dose.
C. ½ of the initial dose
D. ¼ of the initial dose
E. None of the above
17.
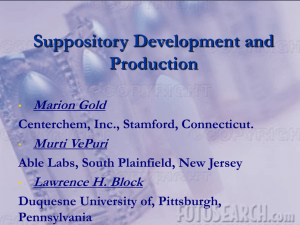
The patient reports to you uncontrollable nausea and vomiting the next day. Every time he drinks anything
(including water) he is stricken with severe retching and vomiting immediately. He has been up most of the night with this recurrent problem, and now is in severe pain because of inability to take his pain medications. What is your plan?
A. Suppository Valium
B. Suppository Phenergan
C. Suppository Versed
D. Suppository acetaminophen
E. Suppository fentanyl (Sublimaze
)
18.
Which of the following local anesthetics are examples of ESTER-type linkages? (Hint: These are generic names)
1. Procaine
2. 3-chlorprocaine
3. Benzocaine
4. Pontocaine
A. 1 and 3
B. 1, 2, 3
C. 2 and 4
D. 4 only
E. All the above
19.
A 6-year-old child undergoes several pulpotomies and
SSC crowns. How much Tylenol with codeine elixir
(120 mg acetaminophen and 12 mg codeine per teaspoon) would you give every 6 hours? The child weighs 50 pounds and you would like to give the equivalent of two Tylenol #3 tablets every 6 hours.
You will have to choose the amount that is CLOSEST to the calculated amount.
A. ½ teaspoon
B. 1 teaspoon
C. 1 ½ teaspoons
D. 2 teaspoons
E. 2 ½ teaspoons
20.
How many mg/cc is in 50% Dextrose?
A. 0.5 mg/cc
B. 5 mg/cc
C. 50 mg/cc
D. 500 mg/cc
21.
Which of the following drugs does NOT contain
Acetaminophen?
A. Fioricet
B. Percocet
C. Darvocet N-100
D. Fiorinal
22.
After receiving an inferior alveolar block using a long
25 gauge needle the patient develops paralysis of some of the facial muscles. This is most probably related to diffusion of the anesthetic solution into the:
A. Otic ganglion
B. Medial and/or lateral pterygoid muscles
C. Motor branches of the mandibular nerve supplying the masticatory muscles
D. Parotid gland
E. Submandibular parasympathetic ganglion
23.
What is the injectable local anesthetic that can cause methemoglobinemia?
A. Lidocaine
B. Mepivacaine
C. Articaine
D. Prilocaine
24.
Caution should be used in giving chronic alcoholics which analgesic?
A. Darvon
B. Darvon compound
C. Darvocet N-100
D. All of the above
E. None of the above
25.
See answer sheet for question and answer area.