suppositories
advertisement

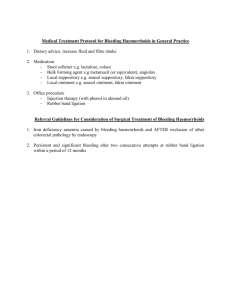
SUPPOSITORIES 1 Dose character: For rectal administration, one half to two or more times than the oral dose is given. - The correct dose of any drug depends on the rate of release from the suppository - Since the vehicle can change the rate of drug absorption , the amount of drug to be given in suppository dose depend on the vehicle, the chemical and physical from the drug. http://commons.wikimedia.org/wik i/Image:Suppositories_three_differ ent_sizes_2.jpg 2 Types: 1- Rectal suppository: 32 mm in length, cylindrical, have one or both end tapered. a) Adult rectal supp. Weight 2gm b) infant rectal supp.1gm 2- Vaginal suppository: pessaries, 5gm, usually oviform or cone shaped, weight from 3-5 gm 3- Urethral suppository: bougies 4gm and 10-15 cm long for male and 6-7.5cm long for female. , pencil shaped. 3 Therapeutic uses Suppository can be used for local or systemic effect. The action depends on nature of drug , concentration and rate of absorption Rectal suppository are intended for treatment of constipation and hemorrhoids. Suppositories are also administered for systemic action (analgesics, antispasmodics, sedatives & tranquilizers). 4 Factor affecting drug absorption form rectal suppository: 1) Physiologic Factor: The human rectum is approximately 15-20 cm in the length, when empty of fecal material; it contains 2-3 ml of inert mucous fluid. In resting state, the rectum is non motile. There is no villa or microvillus on rectal mucosa. Physiological factors include: 5 A) Colonic Content: When systemic effect are desired from suppository greater absorption may be expected from a rectum that is void than that with fecal matter. An evacuation enema maybe administered before insertion of a suppository. Diarrhea, colonic obstruction and tissue dehydration influence the rate & degree of drug absorption from rectum. 6 B) Circulation: Drugs absorbed rectally partially by pass portal circulation, thereby enabling drug destroyed in liver to exert systemic effect. Depending on the height at which absorption occurs at rectum, the drug passes into inferior, middle or superior hemorrhoid veins. The inferior is nearest to the anus, the upper hemorrhoid vein —> portal circulation .thus it is advisable to keep supp in the lower part of rectum. 50% -70% of drug administered rectally, reported to go directly into general circulation. 7 C) pH and lack of buffering capacity of the rectal fluid : Rectal fluids are neutral (pH 7-8), have no effective buffer capacity. The barrier separating colon lumen from the blood is preferentially permeable to the unionized forms of drugs, thus absorption of drug would be enhanced by change in pH of the rectal mucosa to one that increase the proportion of unionized drugs. 8 2) Physiochemical characteristics of the drug: A) Lipid water solubility of a drug (partition coefficient): - The lipid water partition coefficient of a drug is important in selecting the suppository base and in anticipating drug release from that base - lipophilic drug, in other word, distributed in a fatty suppository base has fewer tendencies to escape to the surrounding queues fluids - . 9 - Thus water-soluble salt are preferred in fatty base suppository. water-soluble base e.g: PEG, which dissolve in the rectal fluids, release both water-soluble and oil-soluble drugs. 10 B) Degree of ionization: The barrier separating colon lumen from the blood is preferentially permeable to the unionized forms of drugs, thus absorption of drug would be enhanced by increase the proportion of unionized drugs 11 C) Concentration of a drug in a base: - The more drugs in a base, the more drug will be available for absorption. - If the concentration of the drug in the intestinal lumen is above a particular amount, the rate of absorption is not change by further increase in concentration of drug. - In general, the rate limiting step in drug absorption from suppository is the partitioning of the dissolved drug from the melted base and not the rate of solution of drug in the body fluid. - 12 - Scientists showed that: the rate, at which the drug diffuses to the surface of the suppository, Particle size, and presence of surface-active agents are factors that affect drug release from suppositories. 13 3) Physiochemical Characteristics of the Base and Adjuvant: 1)- Nature of the Base: - Suppository base capable of melting, softening or dissolving to release the drug for absorption. - If the base irritating the colon, it will promote colonic response, lead to increase bowl movement and decrease absorption. 14 2) Presence of Adjuvant in Base : Adjuvant in a formula may affect drug absorption, change the rheological properties of the base at body temperature, or affected the dissolution of the drug. 15 Specifications for Suppository Bases : 1- Origin & Chemical Composition: A brief description of the composition of the base reveals the sours of the origin (natural or synthetic or modified natural products). Physical or chemical incompatibilities with other constituents may be predicted if the exact formula composition is known including preservatives, antioxidants and emulsifiers 16 2- Melting Range : Suppository bases don't have a sharp melting point, their melting characteristics are expressed as ranges, indicating the temperature at which the fats start to melt and the temperature at which completely melted. Melting range is usually determination by " Wiley melting point", "Capillary melting point", " Incipient melting (or thaw)point". 17 3- Solid-Fat Index (SFI): One can determine the solidification and melting ranges of fatty bases as well as the molding character, surface feel and hardness of the bases. A base with sharp drop in solids over a short temperature span proves brittle if molded too quickly. 18 The solid content at room temperature could determine suppository hardness. Since skin temperature is about 32° C, one can predict that would be dry to touch from a solid content over 30% at that temperature. 19 20 4- Solidification Point: This test allow to determine the time required for solidifying the base, when it is chilled in the mold if the interval between the melting point and solidifying point is 10° C or more, time required for solidification may have to be shortened for amore efficient manufacturing procedure by refrigeration, if melting point 33° C and solidifying point 20° C then it will be liquid for 13° C, then the drug will sediment and the apex of the suppository will contain all the drug. 21 5- Hydroxyl Value: "It is the number of milligrams.of KOH (Potassium hydroxide) that would neutralize the acetic acid used to acetylate 1g of fat. It reflects the monoand di-glyceride content of a fatty base. 6- Saponification Value: The number of milligrams of KOH (Potassium hydroxide) required to neutralize the free fatty acids and saponify the ester contained in 1 g of a fat. From saponification value we can know the type of glyceride present (mono-, di- or tri-) and also amount present. 22 7- Iodine Value: It is the number of grams of Iodine that reacts with l00 g of fat or other unsaturated material. The possibility of decomposition by moisture, acids, oxygen (which leads to rancidity of fats) increases with higher iodine value. 8- Water Number: It is the amount of water in grams that can be incorporated in l00g of fat. The "water number" can be increased by the addition of surfaceactive agents. 9- Acid Value: It is the number of milligrams of KOH (Potassium hydroxide) required neutralizing the free fatty acids in I g substance (fat). Low acid value or absence of acid value is important for good suppository bases. 23 Properties of an Ideal Suppository Base: The ideal suppository base may be described as follows : 1- Melts at rectal temperature 36° C, or dissolve in rectal fluid 2- Completely non toxic, and non irritating to sensitive and inflamed tissues. 3- Compatible with a broad variety of drugs. 4-No metastable forms. 5- Shrinks sufficiently on cooling to be released form the mold without the need for mold lubricants. 6- Non- sensitizing 24 7- Has a melting and emulsifying property. 8- Water number is high (a high percentage of water can incorporated in it) 9- It is stable on storage, dose not change odor, color, release pattern. 10- Can be manufactured by molding either by hand, compression, machine . 11- Acid value is below 0.2, saponification value ranges from 200 to 245, and Iodine value is less than 7. 12- SFI curve is sharp, in other word, the interval between melting point and solidification point is small 25 Type of Suppository Bases: A- Fatty Bases. B- Hydrophilic Suppository Bases C-water dispersible Bases 26 A- Fatty Bases: Cacao Butter (theobroma oil) It is the most widely used suppository base. It satisfy many requirement for ideal suppository base : 1) Bland. 2) Non reactive. 3) Melt at body temperature. - Cacao Butter is a triglyceride, yellowish white, solid, brittle fat, smells and taste like chocolate. Its melting point between 30-35° C, it iodine value is “between” 34-38 and its acid value is no higher than 4, because cacao butter can melt and rancid. So it must be stored in cool dry place protected from light. 27 Cacao butter exhibited polymorphism (exist in different crystalline forms). Cacao butter is thought to exist in 4 crystalline states: 1) α - crystal ــmelt at 22oC ــunstable 2) γ - crystal ــmelt at 18oC ــunstable 3) β’ - crystal ــmelt at 27oC ــunstable 4) β – stable crystal ــmelt at 34-36oC ــ stable 28 Various forms of cacao butter depend on: 1- Degree of heating. 2- Cooling process. 3- Conditions during this process. The re-conversion to the stable B- form takes form one to four days depending on the storage temperature, the higher the temperature the faster the change. 29 Disadvantages of Cacao Butter 1- Rancidity and slow deterioration during storage. 2- Melt in warm weather. 3- Liquefy when incorporated with certain drug such as: volatile oils, creosote, phenol and chloral hydrate. 4- Over heating lead to isomerizes to metastable form. So this will decrease melting point. 5- Low contractility during solidification, suppository will adhere to the mold and will be necessitates uses of lubricant. 6- Quality of cacao butter varies with origin and treatment. 7- Water number is low (20-30), this could be improved by addition of 5-10%tween61. 8- Leakage from the body. 30 Advantages of Cacao Butter: 1- Non reactive. 2- Melt at body temp. 3- Solidification point lies 12-13° C below melting point, during formulation the mass can be stirring and maintain cacao butter liquid below its solidification point. 4- Emulsion can be added in Conc 5-10 % to keep insoluble drug suspended. 31 5-Increase conc. of water soluble drugs, lead to decrease melting point until eutectic point is obtained 6- Melted cocoa butter is viscous (semisolid) which help in corporation of drug. The difference in melting point &solidification point is large to give chance for incorporation with drugs. 32 B- Hydrophilic Suppository Bases: 1-Glycerine Suppositories: Glycerine 91 g Sod. Stearate 4g Purified water 5g To make approximately l00g 2- Glycerated gelatin suppositories: Drug & purified water 10g Gelatin 20g Glycerin 70g - Because glycerin is hygroscopic, there suppositories are packed in materials that protect them from environmental moisture. - This base do not melt at body temp., but dissolve in the secretions of the body cavity in which they are inserted. 33 3-Polyethylen glycol (PEG): Marketed as carbowax or polyethylenglycol, exist as liquid or wax like solid depending on molecular weight. Their water soluble, hygroscopic and vapor pressure decrease with increasing average molecular weights. The wide range of melting point and solubility makes possible the formulation of suppository with various degrees of heat stability and with different dissolution rates. They do not hydrolyze or deteriorate, are physiologically inert and do not support mold growth. Base usually dipped in water before insertion, so that possible irritation maybe eliminated 34 3-WATER - DISPERSIBLE BASE Several non-ionic surface active materials, closely related chemically to PEG as suppository bases. The bases can be used for formulation both water-soluble and oil-soluble drugs (e.g.; Tween & Span). These surface active agents may be used alone, blended or used in combination with other suppository vehicle. Another type of water dispersible suppository vehicle is based on the use of water soluble cellulose derivatives (e.g. methylcellulose & sodium carboxymethylcellulose ). Advantages of Water Dispersible Bases: 1. Stable on storage at elevated temperature. 2. Compatible with many drugs. 3. Non support of microbial growth, non toxic and non sensitive. 35 Method Of Manufacture Of Suppositories: 1- Hand Molding: It is the oldest and simplest method, by rolling the suppository into the desired shape. The mass is then rolled into a cylindrical rod of desire length and diameter. 2- Compression Molding: Elegant suppository can be made b compression the coldgrated mass into the desired shape . It is simple and more elegant appearance than hand molding. It avoids the possibility of sedimentation of the insoluble solids in the suppository base. 36 3- Pour Molding: Most commonly used method for production of suppository on both small & large scale. First, the base is melted on water bath, and then the drugs are either emulsified or suspended in it. Then, the mass is pour into cooled metal molds, which are usually chrome or nickel plated. 4- Automatic Molding Machine: The molding operation (pouring, cooling & removal) can be performed by machine . The output of a typical rotary machine, range from 3500 to 6000 suppositories per hour. 37 38 SPECIFIC PROBLEMS IN FORMULATING SUPPOSITORIES : 1- Water in suppositories: Use of water as a solvent for drug should be avoided for the following Reasons: a- Water accelerates oxidation of fats. b- If water evaporates, the dissolved substance crystallizes out. c- Unless H2O is present at level than that requires for dissolving the drug, the water has little value in facilitating drug absorption. Absorption from water containing suppository enhance only if an oil in water emulsion exist with more than 50% of the water in the external phase . d- Reaction between ingredients (in suppository) are more likely to occur in the presence of water. e- The incorporation of water or other substances that might be contaminate with bacteria or fungi necessitates the addition of bacteriostatic agents (as parabens) 39 2- Hygroscopicity: a- Glycerinated gelatin suppositories lost moisture by evaporation in dry climates and absorbed moisture under conditions of high humidity b- PEG bases are also hygroscopic. 40 3- Incompatibilities: a- PEG bases are incompatible with silver salt, tannic acid, aminopyrine , quinine , icthammol, asprine , benzoc.aine & sulphonamides . b- Many chemicals have a tendency to crystallize out of PEG, e.g.: sodium sarbital, salicylic acid & camphor. c- Higher concentration of salicylic acid softens PEG to an ointment-like consistency, d- Aspirin complexes with PEG. e- Penicillin G , although stable in cocoa butter and other fatty bases , was found to decompose in PEG bases . f- Fatty bases with significant hydroxyl values may react with acidic ingredients. 41 4- Viscosity: The viscosity of the melted suppository base is important in the manufacture of the suppository and to its behavior in the rectum after melting. Melted cocoa butter have low viscosity than glycerinated gelatin and PEG type base in low viscosity bases, extra Care must be exercised to avoid sedimentation of suspended particles. To overcome the problems caused by use of low viscosity bases: a- Use base with a more narrow melting rang that is closer to body temperature. b- The inclusion of approximately 2% aluminum monostearate not only increase the viscosity of the fat base but to maintain homogenous suspension of insoluble material. c- Cetyl , stearyl or myristyl alcohols or stearic acid are added to improve the consistency of suppositories . 42 5- Brittleness : Suppositories made from cocoa butter are elastic and don't fracture readily. Synthetic fat base with high degree of hydrogenation and high stearate content and a higher solids content at room temperature are usually more brittle. To overcome, 1) the temperature difference between the melted base & the mold should be minimal. 2) Addition of small amount of Tween 80, castor oil, glycerin imparts plasticity to a fat 43 6- Volume contraction: Occurs in many melted suppository base after cooling the mold, result in: a- Good mold release (contraction facilitate the removal of the suppository from the mold , eliminating the need for mold release agents). b- Contraction hole formation at the open end of the mold, this will lowered suppository . The contraction can be eliminated by pouring a mass slightly above its congealing temperature into a mold warmed at about the same temperature or the mold is overfilled so that the excess mass containing the contraction hole can be scraped off. 44 Lubricant or mold releasing agent: Cocoa butter adhere to suppository molds because of its low volume contraction. A various mold lubricants or release agents must be used to overcome this difficulty (mineral oil , aqueous solution of sodium lauryl sulfate , alcohol , silicones , soap). The release of suppository from damaged mold was improved by coating the cavities with polytetrofluoroethylene (Teflone). 45 7- Rancidity and Antioxidant: Rancidity results from the autoxidation and subsequent decomposition of unsaturated fats into low & medium molecular weight saturated & unsaturated aldehydes , ketones and acids , which have strong unpleasant odor. Example of effective antioxidant are phenols such as " hydroquinone or B-naphtholquinone. 46 DOSAGE REPLACEMENT FACTOR The amount of base that is replaced by active ingredient in suppository formulation can be calculated. The replacement factor (f) is derived from the following equation: F=100(E-G)+1 Where: E= weight of pure suppository base. G= weigh of suppositories with x% active ingredient. 47 WEIGHT AND VOLUME CONTROLE: The amount of active ingredient in each suppository depends on: 1 . Its concentration in the mass. 2. The volume of the mold cavity. 3. The specific gravity of the base. 4. The volume variation between molds (within 2% of the desired value). 5. Weight variations between suppositories due to inconsistencies in the manufacturing process. e.g. incomplete closing of molds, uneven scrapings (variations in weight should be within ± 5%) 48 Quality Control of Suppository 1) Surface appearance and shape: to evaluate: absence of fissuring – absence of migration of active ingredient, absence of pitting, absence of fat blooming (dullness of surface) 49 2) MELTING RANGE TEST: Macromelting range: measures the time it takes for the entire suppository to melt when immersed in a constant temperature (370C) water bath. Micromelting range: is the melting range measured in capillary tubes for the fat base only. The apparatus used for measuring the melting range of the entire suppository is a USP tablet disintegration apparatus. The suppository is completely immersed in the constant temperature water bath, and the time for the entire suppository to melt or dispense in the surrounding water is measured. The in-vitro drug release pattern is measured by using the same melting range apparatus. 50 3) LIQUIFACTION OR SOFTENING TIME TESTS OF RECTAL SUPPOSITORIES: The "softening test" measures the liquefaction time of rectal suppositories are an apparatus that simulate in-vitro conditions (at 37oC). 51 52 4) BREAKING TEST: It is designed as a method for measuring the fragility or brittleness of suppositories. The apparatus consists of double-wall chamber in which the test suppository is placed. Water at 37C is pumped through the double walls of the chamber, and the suppository, contained in the drug inner chamber, supports a disk to which a rod is attached. The outer end of the rod consists of another disc to which weights are applied. 53 54 5) Mechanical strength: It is a force necessary to break a supp. And indicate whether supp is brittle or elastic. ( not less than 1.8-2 Kg) by Erweka method 6) Melting & solidification Solidification can be determine by using evacuated flask into which the melt is placed, the temp of cooling is noted to determine the solidification point. 55 7) DISSOLUTION TESTING: The patterned is measured by using the same melting range apparatus. If the volume of water surrounding the suppository is known, then by measuring aliquots of the water for drug content at various intervals within the melting period. A (time versus drug release) curve could be established and can be plotted. 56 PACKAGING OF SUPPOSITORY Suppository must be placed in a container in such a manner that they do not touch each other. • Staining, breakage or deformation by melting caused by adhesion can result from poorly wrapped packaged suppository. Suppository is foiled in tin or Al paper and plastic. • Over wrapping is done by hand or machine. Many suppositories are not individually, wrapped. In such cases, they are placed into cardboard boxes or plastic containers that have been molded to provide compartment for 6 or 12 suppositories. 57 IN- PACKAGE MOLDING: A significant advance in suppository manufacturing was the development of automated method for molding suppository, directly in their wrapping materials. This is currently accomplished with either plastic or Al-foil. *ADVANTAGE OF INPACKAGE MOLDING: 1. high production rate. 2. no generation of scraping. 3. no bulk handling. 4. maintenance of strict temperature control 58 STORAGE Suppository should be protected from heat, preferably stored in the refrigerator. Glycerinated gelatin suppositories should be protected from heat, moisture, and dry air by packaging in well-sealed containers and storing in a cool place. 59