Appendix 1
advertisement

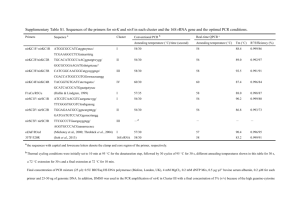
Online Data Supplement Use of culture and molecular analysis to determine the effect of antibiotic treatment on microbial community diversity and abundance during exacerbation in cystic fibrosis patients M M Tunney, E R Klem, A A Fodor, D F Gilpin, T F Moriarty, S J McGrath, M S Muhlebach, R C Boucher, C Cardwell, G Doering, J. S Elborn, M C Wolfgang MOLECULAR DETECTION METHODS DNA Isolation Total DNA was extracted from approximately 200 mg aliquots of frozen (-80°C) sputum samples using a FastPrep Instrument in combination with the FastDNA Spin Kit (MP Biomedicals) according to the manufacturer’s protocol. Isolated DNA was passed over a Zymo-Spin IV-HRC column to remove PCR inhibitors (Zymo Research) and quantified with Quant-iT PicoGreen dsDNA reagent (Invitrogen). T-RFLP Analysis Terminal-Restriction Fragment Length Polymorphism (T-RFLP) analysis was performed as previously described. [1 ,2] Briefly, 100 ng of isolated DNA was used as template for PCR amplification using modified versions of the universal bacterial 16S rRNA gene specific primers Bac8f (5’-NAGRGTTTGATCCTGGCTCAG) and Bac926r (5’- NCCGTCAATTCCTTTRAGTTT) and AmpliTaq Gold 2x PCR Master Mix (ABI). The Bac8f and Bac926r primers were fluorescently labelled at the 5’ end with 6FAM and HEX, respectively (Eurofins MWG Operon). For each DNA sample, three 50 µl PCR reactions were pooled and digested with ExoSAP-IT (USB) to 1 remove excess primers and incomplete single stranded PCR fragments according to the manufacture’s specifications. Double stranded DNA products were purified using a Montage PCR Device (Millipore) and DNA concentration determined with QuantiT PicoGreen dsDNA reagent. For each DNA sample, 250 ng of the resulting duallabelled PCR product was digested in two separate reactions with the restriction endonucleases HaeIII and HhaI (New England Biolabs), respectively. Digested DNA fragments were purified and desalted with mini Quick Spin Oligo Columns (Roche) using the manufacturer’s supplemental desalting protocol. Digested DNA (2 µl) was added to 10 µl of a cocktail of Hi-Di Formamide (Applied Biosystems) and CSTROX-25-1000 custom sizing ladder (BioVentures). The resulting mixture was loaded onto an ABI 3130 Genetic Analyzer, utilizing a 36 cm 4-capilary array, containing POP-7 polymer and 1x running buffer. Foundation Data Collection 3.0 software was used to run the Genetic Analyzer and data was viewed with GeneMapper 4.0 (Applied Biosystems). All software was run with default factory settings although a custom run module was created for separation of fragments up to 1000 nucleotides in length. Traces with off-scale peaks were rerun with a shorter injection time until all peaks were on-scale. Traces with low peak amplitude were repeated with more DNA and/or a longer injection time. Using the above method, a total of four T-RFLP spectra (representing both 5’ and 3’ terminal restriction fragments generated by two different restriction endonucleases) were produced for each patient sample. In order to identify bacterial genera within the patient T-RFLP spectra, we created clone libraries from PCR products targeting the 16S rRNA gene in DNA isolated from a previously collected set of CF sputum. For 33 unique clones (online supplementary Table 2), representing the predominant aerobic and anaerobic bacterial genera identified in previous culture and molecular-based detection studies of CF 2 sputa,[3-7] we generated both DNA sequences and T-RFLP spectra (as above). The clone sequences were identified to genus using the Ribosome Database Project Classifier algorithm.[8] As our classifications involve many taxa, some of which have not been well studied and for which database characterizations are therefore incomplete, we restricted all RDP classifications to the genus level. To assign taxa to each patient sample, we systematically compared T-RFLP spectra for the 33 reference clones (representing 22 different genera) samples to the spectra generated for the 64 CF patient samples. After running all reference and patient samples through our custom peak calling algorithm (available upon request), we normalized our data by dividing the intensity of each peak in each spectra by the total intensity of all peaks in that spectra. We then calculated for each reference spectra the degree of overlap between the peaks in the reference spectra and the peaks in each sample spectra. In the case of perfect overlap between a reference and sample spectra, this comparison would yield a score of 1. If there were no peaks in common between a reference and sample spectra, this comparison would yield a score of 0. We performed this calculation independently for 3 spectra (5’ and 3’ termini for HaeIII and the 5’ termini for HhaI; the 3’ termini for Hha contains overlapping predicted peaks for several abundant taxa including Granulicatella, Streptococcus and Burkholderia and was therefore not used). We summed the results for all 3 spectra to produce a single score reflecting the degree of overlap between reference and sample spectra. For our T-RFLP predictions, we chose as a threshold 0.2, which corresponds to a 6.67% overlap between the peaks of the reference and sample spectra. 251 of the scores met this threshold and hence in each of these 251 cases the genus was marked “present” in the sample (Table 2, manuscript). There are a number of assumptions 3 that we make in our estimates that may lead to some inaccuracy. We have made no attempt to correct for multiple taxa sharing similar peaks. In addition, our permutations assume that a restriction cut of any length is equally probable; this is not necessarily true as the 16S rRNA gene has conserved and variable regions and therefore some peaks may occur more frequently than others across all reference spectra. Estimation of Total Bacterial Load Quantitative, real-time PCR (QRT-PCR) was used to determined total bacterial load in each sputum sample. Purified DNA (described above) was analyzed in duplicate reactions at three different template amounts (40 ng, 20 ng, and 10 ng) using a previously published [9] set of universal primers and TaqMan probe that amplify a conserved fragment of the bacterial 16S rRNA gene. PCR reactions were performed using an ABI 7500 Fast Real-Time PCR System with TaqMan Gene Expression Master Mix (Applied Biosystems). 16S rRNA gene copies per gram of sputum were calculated using the highest average 16S rRNA gene copy number for each template. A plasmid containing the cloned 16S rRNA gene from E.coli was used as the standard for determining copy number in the human derived DNA samples. Statistical analysis Normally distributed patient characteristics were presented as mean (SD) whilst nonnormal characteristics were presented as median (inter-quartile range). Age, weight and FEV1 were compared within participants before and after antibiotic treatment and until stable using paired samples t-test. CRP and WCC were compared before and after antibiotic treatment and until stable using Wilcoxon signed-rank tests. 4 Spearman’s rank correlation coefficients were calculated to measure the strength of the linear association between T-RLFP and total viable counts. Aerobe and anaerobe viable counts were compared at each sampling timepoint (initiation and completion of antibiotic treatment, stable) using Wilcoxon signed-rank tests. The effect of antibiotic treatment on bacterial abundance was determined by comparing both aerobic and anaerobic counts before and after antibiotic treatment using Wilcoxon signed rank tests. For the subset of patients, in which 3 samples were collected (initiation and completion of antibiotic treatment, stable), aerobe and anaerobe total viable counts were compared between the three groups using Friedman’s test. For those matched sample pairs in which P. aeruginosa had been detected on admission for treatment, total viable counts were compared before and after antibiotic treatment using Wilcoxon signed rank test. The log10 qPCR was compared before and after antibiotic treatment using a paired samples t-test. A Spearman’s rank correlation coefficient was used to measure the strength of the linear association between the sum of the total aerobe and anaerobe counts and the qPCR values. Statistical analysis was performed with the SPSS (SPSS Version 14, Chicago, Illinois, USA) software package. REFERENCES 1. Dicksved J, Lindberg M, Rosenquist M, et al. Molecular characterization of the stomach microbiota in patients with gastric cancer and in controls. J Med Microbiol 2009;58(Pt 4):509-16. 2. Sibley CD, Parkins MD, Rabin HR, et al. A polymicrobial perspective of pulmonary infections exposes an enigmatic pathogen in cystic fibrosis patients. Proc Natl Acad Sci U S A 2008;105(39):15070-5. 3. Rogers GB, Carroll MP, Serisier DJ, et al. Characterization of bacterial community diversity in cystic fibrosis lung infections by use of 16s ribosomal DNA terminal 5 restriction fragment length polymorphism profiling. J Clin Microbiol 2004;42(11):5176-83. 4. Rogers GB, Carroll MP, Serisier DJ, et al. Use of 16S rRNA gene profiling by terminal restriction fragment length polymorphism analysis to compare bacterial communities in sputum and mouthwash samples from patients with cystic fibrosis. J Clin Microbiol 2006;44(7):2601-4. 5. Rogers GB, Carroll MP, Serisier DJ, et al. Bacterial activity in cystic fibrosis lung infections. Respir Res 2005;6:49. 6. Harris JK, De Groote MA, Sagel SD, et al. Molecular identification of bacteria in bronchoalveolar lavage fluid from children with cystic fibrosis. Proc Natl Acad Sci U S A 2007;104(51):20529-33. 7. Tunney MM, Field TR, Moriarty TF, et al. Detection of anaerobic bacteria in high numbers in sputum from patients with cystic fibrosis. Am J Respir Crit Care Med 2008;177(9):995-1001. 8. Cole JR, Wang Q, Cardenas E, et al. The Ribosomal Database Project: improved alignments and new tools for rRNA analysis. Nucleic Acids Res 2009;37(Database issue):D141-5. 9. Nadkarni MA, Martin FE, Jacques NA, et al. Determination of bacterial load by real-time PCR using a broad-range (universal) probe and primers set. Microbiology 2002;148(Pt 1):257-66. 6 Table 1 Antibiotic regimens used to treat infective pulmonary exacerbations Antibiotic regimen Number of exacerbations treated Tobramycin, ceftazidime 9 Tobramycin, piperacillin/tazobactam 8 Tobramycin, meropenem 1 Tobramycin, temocillin, ciprofloxacin 1 Tobramycin, ciprofloxacin, colomycin 1 Temocillin, colomycin 2 Temocillin, meropenem 1 Piperacillin/tazobactam, colomycin, ciprofloxacin 1 Amikacin, meropenem 1 Amikacin, clindamycin, moxifloxacin, clarithromycin 1 7 Table 2 Reference clones generated from sequenced 16S rRNA genes used to identify bacterial genera present in T-RFLP spectra from CF sputa samples Clone ID UNCCF0001 UNCCF0002 UNCCF0003 UNCCF0004 UNCCF0005 UNCCF0006 UNCCF0007 UNCCF0008 UNCCF0009 UNCCF0010 UNCCF0011 UNCCF0012 UNCCF0013 UNCCF0014 UNCCF0015 UNCCF0016 UNCCF0017 UNCCF0018 UNCCF0019 UNCCF0020 UNCCF0021 UNCCF0023 UNCCF0024 UNCCF0025 UNCCF0026 UNCCF0027 UNCCF0028 UNCCF0029 UNCCF0030 UNCCF0031 UNCCF0032 UNCCF0033 UNCCF0034 Accession GU361868 GU361872 GU361876 GU361860 GU361873 GU361864 GU361880 GU361884 GU361888 GU361874 GU361882 GU361861 GU361887 GU361871 GU361879 GU361859 GU361862 GU361869 GU361870 GU361890 GU361883 GU361886 GU361889 GU361863 GU361878 GU361866 GU361881 GU361877 GU361875 GU361865 GU361891 GU361867 GU361885 RDP Classification Haemophilus; 100% Fusobacterium; 100% Neisseria; 100% Porphyromonas; 100% Granulicatella; 100% Rothia; 100% Actinomyces; 100% Streptococcus; 100% Streptococcus; 100% Streptococcus; 100% Gemella; 100% Propionibacterium; 100% Burkholderia; 100% Prevotella; 100% Prevotella; 100% Pseudomonas; 100% Corynebacterium; 100% Veillonella; 100% Atopobium; 100% Streptococcus; 100% Actinomyces; 100% Actinomyces; 100% Devosia; 100% Pasteuriaceae Incertae Sedis; 100% Planomicrobium; 97% Prevotella; 100% Ralstonia; 100% Actinomyces; 100% Achromobacter; 100% Prevotella; 100% Prevotella; 100% Prevotella; 100% Staphylococcus; 100% 8 Table 3: Summary of bacterial genera detected by culture and T-RFLP in CF sputum at initiation and completion of IV antibiotic treatment for an exacerbation and when stable Key genera detected by culture genera detected by T-RFLP Ex: initiation of antibiotic treatment for an exacerbation (for the 3 patients treated twice for an exacerbation, samples denoted as 1 and 2) EOT: completion of antibiotic treatment for an exacerbation ST: stable *No quantitative culture results available # No T-RFLP results available 9 Figure 1 10 Figure 1 Summary of bacterial genera detected by culture and T-RFLP in sputum samples collected from 23 adult CF patients on initiation of antibiotic treatment (Ex) and completion of antibiotic treatment (EOT) for an exacerbation and when stable (ST). Three of the patients (patients 1, 11 and 19) were treated twice for exacerbation during the course of the study resulting in a total of 26 matched initiation/completion of treatment sample pairs. The legend shows the different bacterial genera detected by either method and is sorted by known or observed culture conditions for the respective organisms. Genera marked with an asterisk (*) could not be identified by T-RFLP analysis due to the lack of corresponding reference spectra (online supplementary Table 2). A) Total viable counts (TVC) of bacteria detected by both aerobic and anaerobic culture. The y-axis shows the cumulative sum of log10 (TVC) for all cultured microbes. B) Culture-independent T-RFLP analysis of microbial community composition. The y-axis indicates the cumulative T-RFLP prediction score for each of the bacterial genera identified in a patient sample. In order to reduce false positive identification of bacterial genera, a prediction score cutoff of 0.2 was applied, which requires at least 5% of the peak area in a patient sample to match the corresponding peaks in a given reference spectra. 11 Figure 2. Representative T-RFLP spectra from patient 11 generated at each of the indicated timepoints. At each time point, 4 T-RFLP spectra were generated using two different enzymes (Hae and Hha) with both the 5’ and 3’ end carrying the fluorophore label. Both exacerbations in this patient were treated with a combination of tobramycin and ceftazidime. 12 P*=0.01 1012 Total bacterial concentration concentration (16S rRNA gene copies/G) 1011 1010 109 108 107 P†=0.05 End of treatment Exacerbation Stable * Comparing two groups using paired samples t-test. † Comparing 3 groups using multivariate analysis of variance. Figure 3 Quantitative PCR (qPCR) measurements of the 16S rRNA gene copy number from CF sputum samples collected from adult patients with CF at initiation (Exacerbation) and completion of IV antibiotic treatment (End of Treatment) for an exacerbation and when stable (Stable). 13