Emerging Infectious Disease and Infection Control
advertisement
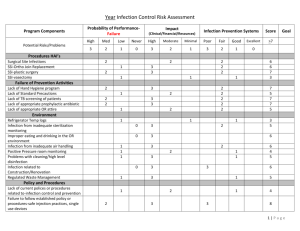
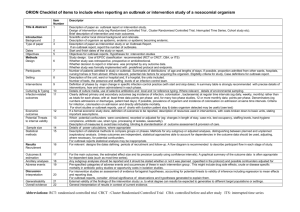
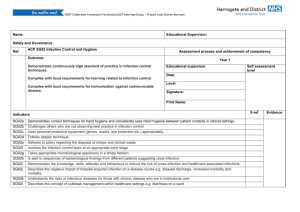
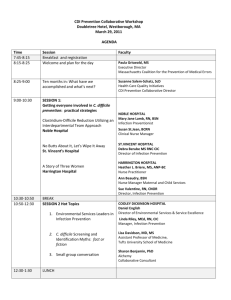
RI Committee on Occupational Safety &Health ____________________________________________________________ What you going do if it comes for you? Emerging Infectious Disease and Infection Control Avian flu has ratcheted up attention to the potential threat for a major pandemic outbreak. The emergence of any new infectious pathogen creates unique problems especially for workers directly engaged in dealing with an outbreak. The safety and health of emergency responders, health care, and public safety workers will need to be a critical part of evolving infection control policies and practices since their ability to function will be crucial in halting and controlling the spread of an outbreak. No one is sure when, or even whether, an outbreak will occur. From the perspective of occupational health the principal step as of now is to become familiar with current infection control policies and procedures, especially for a pandemic event and to get involved with the discussion about these policies. Coordinated Planning There are two broad currents to the policies and procedures under development. The first is extra-institutional. This involves planning within the context of large-scale interventions. During the SARS outbreak several steps were taken which serve to inform current planning: at this level expect to see infection control policies that address a set of connected themes: Pharmaceutical therapies that can immunize, or minimize impact of the infectious the agent – locating and isolating patients, monitoring and quarantining contacts, travel restrictions, screening travelers, maintaining strict infection control procedures within high risk settings, limiting public gatherings. One key to this level of the planning is to discuss the tensions between staffing and public health interventions. (During the SARS outbreak 60% of quarantined healthcare workers in Toronto could not explain why they were under quarantine.) National programs and projections are available through the Centers for Disease Control and the WHO. (If the SARS outbreak can be said to have had a positive impact, it is, that it helped to prime many in the health community for similar situations. It has galvanized the international medical community (WHO) which will be critical for surveillance, operational guidance and response throughout the world. ) The local Health Department has been working with hospitals on various phases of coordinated planning under bioterrorism preparedness. These plans can and should be reconfigured to address natural threats. Facility /Institutional Roles Within statewide planning certain key public safety agencies, hospitals, fire departments will have designated roles to play in an outbreak. They are occupationally at higher risk. Workers in each should become familiar with these roles and make sure that protections for worker safety and health are addressed and understood. Take two examples: A hospital or units in a hospital may be designated as special quarantine units. Workers within these units will need to specialized training as regards controlling transmission and protecting themselves. E.g. what critical infection controls should they follow, what respirator protections etc. Or, emergency responders may be first on the scene to deal with infected patients or asked be asked to transport patients. They should understand the appropriate quarantine and infection control policies and procedures appropriate to their risk and situation, including what to expect as far vaccine and or antiviral medications they might be issued. What is an Infection Control Policy An infection control plan will shift target and focus depending on the characteristics of an infectious agent – virulence, transmission mode (air, bodyfluids, surfaces), attack rates (in different age groups), vaccine protection (if any), susceptibility to antivirals, and response to other treatments. However, there are certain generic features an infection control program will address: criteria for detecting a “case.” standard precautions; isolation practices; planning relating to specific wards and isolations; respiratory protection policy (airborne and droplet precautions; patient cough etiquette; masking issues. strict enforcement of hand and surface hygiene; role of vaccines and anti-viral meds and related therapies (e.g. drugs that interrupt mediators of sepsis). In a like vein other agencies and institutions may play a secondary active role (e.g. the media, public transit, and school personnel) or be involved (e.g. colleges and universities) by virtue of the fact that they have sizable groups of people on site.) What is vital for these collateral institutions and agencies is to make their needs and situation(s) known to those who are designing infection control and response. This dialogue will be critical in helping to shape a workable and practical response. RI Committee on Occupational Safety & Health 741 Westminster St. Prov RI 02903 (401) 751-2015/jobhealth@juno.com