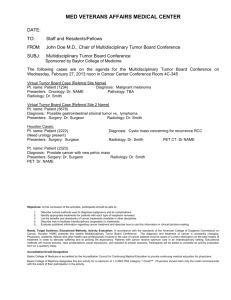
Case 1
advertisement

Clinical history: 43 y.o. white female patient with a 4 years history of infiltaring poorly differented ductal carcinoma of the breast presenting with a pelvic mass. The sections were taken from the pelvic tumor. An immunostain for GCDFP is negative. Choose a correct diagnosis: a. Metastatic ductal carcinoma of the breast b. High grade serous carcinoma c. Granulosa cell tumor d. Metastatic melanoma Correct diagnosis: High grade serous carcinoma Discussion: The mass consists of sheets of poorly differentiated tumor cells with scattered gland formation that is histologically different from the patient's ductal carcinoma of the breast (see image). The tumor is diffusely and strongly positive for CK7, ER, PAX-8 and WT-1, variably positive for PR and is negative for GCDFP, CK20, CEA, MelanA, SMA, Desmin, CD34 and S100. This immunoprofile supports an ovarian origin and is consistent with a high grade serous carcinoma. The origin of metastatic poorly differentiated carcinomas of the breast and ovary can be difficult to recognize. This is particularly true if the metastasis occurs in an anatomic location where both tumors commonly metastasize. Rarely, ovarian tumor s can metastasize to the breast or axillary lymph nodes where they may be misdiagnosed as mammary carcinoma. Similarly, a subset of breast cancer (typically lobular carcinoma) can involve the ovaries and thus present as pelvic masses. Immunohistochemistry is helpful in most instances, since breast cancers are PAX-8 and WT-1(with rare exceptions for WT-1) negative, whereas ovarian serous carcinomas are positive. The opposite is true our most used breast markers GCDFP and mammoglobin. While the majority of ovarian tumors are negative for both markers, there are tumors that are positive for either or both markers. Clinical history: 66 y.o. white male patient with a 14.5 cm mediastinal mass that was attached to the pulmonary ligament. Choose a correct diagnosis: a. Solitary fibrous tumor b. Leiomyoma c. Leiomysarcoma, low grade d. Desmoplastic mesothelioma Correct diagnosis: Leiomysarcoma, low grade Discussion: NOTE: The tumor infiltrates and distends the pleura and focally involves the serosal surface, however, the attached portions of lung do not show invasion into the lung parenchyma. The tumor is variably cellular ranging from highly cellular areas with storiform pattern to hyalinized areas with low cellularity. Pleomorphic tumor cells are present but no necrosis is noted and mitosis are not readily identified. Immunostains demonstrate that the tumor cells are desmin, smooth muscle actin and bcl-2 positive, and cytokeratin (AE1/AE3), S-100 and CD34 negative. This staining pattern supports the diagnosis of a smooth muscle neoplasm. Focal dystrophic ossification is also seen. The tumor focally infiltrates fibroadipose tissue consistent with parietal pleura where tumor is seen abutting but not involving the inked surface of fibroadipose tissue. These areas may represent the site of attachment to the parietal pleura observed during surgery. On H&E stain the tumor is a low grade spindle cell neoplasm with features of a low grade smooth muscle cell tumor. The characteristic vessels of a solitary fibrous tumor are not present. Immunohistochemically, the tumor cells express muscle markers, and are negative for cytokeratin, CD34 and S-100 a pattern that supports. Bcl-2 positivity is usually not seen in smooth muscle cell tumors and is interpreted as aberrant expression. Since this a pleural/mediastinum based smooth muscle neoplasm it should be graded as a deep seated smooth muscle tumor. Because of the presence of pleomorphic tumor cells even in the absence of necrosis and increased mitotic activity the tumor should be considered a low grade leiomyosarcoma. Clinical history: 67 y.o. white female patient with 14 cm left kidney mass. Choose a correct diagnosis: a. Mixed epithelial and stromal tumor of kidney b. Cystic nephroma c. Cystic renal cell carcinoma d. Polycystic kidney disease Correct diagnosis: Mixed epithelial and stromal tumor of kidney Discussion: The tumor exhibits morphologic features of both cystic nehproma and mixed epithelial and stromal tumor (MEST) of the kidney. It contains a dominant (12.5 cm) cyst that has no lining and is filled with hemorrhagic acellular material. The surrounding smaller cysts are lined by a single layer of flat epithelial or hobnail cells. The intervening stroma is fibrotic with focal areas showing hypercellular, ovarian-type stroma. Scattered aggregates of smaller tubular structures with surrounding cellular stroma are also present. Areas with multiple, small to medium sized cysts and scant fibrotic intervening stroma represent features typically seen in cystic nephroma, whereas areas with more abundant stroma with focal small tubular structures are more often seen in MEST. The morphologic features of these two rare benign neoplasms show significant overlap and thus in selected cases the distinction between these two entities can be difficult. Reference: Am J Surg Pathol, vol 31;No4:489-500; Apr. 2007. Clinical history: 28 y.o. white male patient with 3.2 cm subcutaneous soft tissue mass on the back Choose a correct diagnosis: a. High grade sarcoma consistent with malignant fibrous histiocytoma b. Malignant melanoma c. Malignant peripheral nerve sheath tumor d. Pleomorphic rhabdomyosarcoma Correct diagnosis: Pleomorphic rhabdomyosarcoma Discussion: The tumor is composed of variably pleomoprpic spindle and focally polygonal shaped cells with variable amount of dense eosinophilic cytoplasm. The mitotic activity is high and no necrosis is noted in the single section available for review. Immunostains demonstrate that the tumor cells are positive for desmin and smooth muscle actin, focally positive for myogenin and cytokeratin (AE1/AE3 and Cam5.2), and are negative for CK903, S-100 and Melan-A. This staining pattern supports the diagnosis. Pleomorphic rhabdomyosarcoma (PRMS) is a high grade sarcoma composed of polygonal, round and spindle shaped cells with dense eosinophilic cytoplasm marked pleomorphism that lack morphologic evidence of myogenic differentiation. No embryonal or alveolar component should be noted. PRMS occurs in adults (more commonly in males) and most are in deep soft tissues of the extremities. Cross striations are extremely rare. Clinically, they are rapidly growing painful lesions. Like other muscle tumors PRMS express common muscle markers like desmin, skeletal muscle myosin, variably express smooth muscle actin and myogenin and MyoD1. The MyoD1 and myogenin expression is usually more limited than those seen other types of RMS. Epithelial markers and S-100 are usually negative. The prognosis is poor. Clinical history: 28 y.o. woman with an anal fistula Choose a correct diagnosis: a. Pilonidal sinus b. Pulse granuloma c. Granuloma annulare d. Crohn’s disease Correct diagnosis: Pulse granuloma Discussion: Sections show anal skin with dermal fibrosis, fistula tract and small hyalinized fibrotic perivascular nodules with associated mild chronic inflammation skin with fistula tract and associated (so called hyaline angiopathy or pulse granuloma). Hyaline angiopathy or pluse granuloma are hyalinized ring-like or nodular structures that are seen in areas of chronic inflammation. In the oral cavity they typically occur in areas of periostitis often with associates food particles. The finding has no clinical significance and is thought to be secondary to a reaction to seeds and other food vegetable matter. An alternative hypothesis is that they represent old vasculitis. Clinical history: 42 y.o. African American female patient with a right lower lobe lung nodule. Choose a correct diagnosis: a. Organizing pneumocystis pneumonia b. Organizing Cryptococcus pneumonia c. Sarcoidosis d. Histoplasmosis Correct diagnosis: Organizing Cryptococcus pneumonia Discussion: Sections show a lung nodule with organizing frothy exudate with associated chronic inflammation with small poorly formed granulomata and scattered giant cells. The nodule is well demarcated but not encapsulated and does not have a fibrous wall. No necrosis or hyalinization is present. On H&E stains there are small refractive appearing round structures within the frothy exudates and in the cytoplasm of some giant cells that are positive for variably sized round to oval spore forms on a fungal (GMS) stain. No dot-like staining is noted within the organisms. A mucin stain is negative, whereas a FontanaMasson stain shows strong staining in the wall of these microorganisms consistent with capsule deficient cryptococci. Rarely, organizing, vaguely granulomatous inflammation may be seen in association with both pneumocystis and cryptococcus infections and thus can be difficult to diagnose. In the majority of cases Cryptococcus can be diagnosed by performing a mucin stain which can highlight the mucopolysaccharide capsule of the organisms. In a minority of cases, like the current one, however, the capsule is lost and therefore a mucin stain is negative. Based on the staining pattern on a fungal stain the differentiation between Cryptococcus and other fungal organisms can be difficult. A Fontana-Masson stain is very useful in this setting since it will only stain capsule deficient cryptococci.