Parkinson`s Disease
advertisement

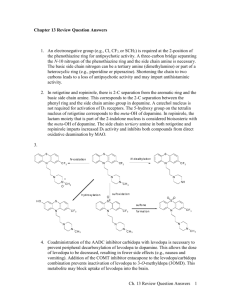
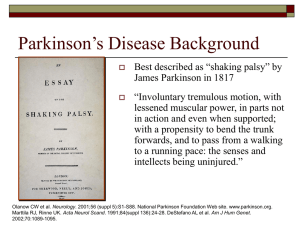
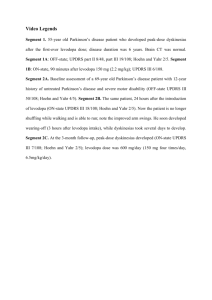
Parkinson’s Disease History 1. How long has Parkinson’s been around? Ans. Probably more than 182 years. 2. Who was the disease named after? Ans. James Parkinson in 1817. What Is It? 1. What is Parkinson’s disease? Ans. Parkinson’s disease is a neurodegenerative disease. Parkinson’s Disease is defined by its cardinal features. 2. What are the cardinal features of Parkinson’s disease? Ans. They are: i. Bardykinesia- which is slowness of movement, which includes difficulty initiating movements, incompleteness of ongoing movements, and arrest of on going movements. ii. Muscle rigidity- which is an increased resistance to stretch at major joints. It can be felt at one, several, or all major joints. iii. Resting Tremor- occurs when muscles are relaxed iv. Postural Instability- is the inability to respond to or compensate for hidden changes such as an abrupt turn 3. Who does Parkinson’s diseases effect? Ans. 1% of all adults over 65. There seems to be a correlation; the older you are the more likely you are to get Parkinson’s disease. 4. At what level of dopamine depletion in Parkinson’s considered a clinical disease? Ans. When 80% of dopamine neurons are lost and your body has been depleted of dopamine to about 20%. 5. What is the cause of Parkinson’s disease? Ans. The cause is unknown. There is no test that reveals a cause or confirms the diagnosis of the disease. 6. Is there a cure for Parkinson’s disease? Ans. NO Biological Aspects 1. What occurs in the brain of someone who has Parkinson’s? Ans. What happens is the part of the brain that produces dopamine, the substantia nigra, begins to decrease in number, which causes decrease amount of available dopamine. Your brain is also breaking down dopamine in the synapse naturally by MAO-B. This leaves you with little dopamine, and the loss of dopamine throws off the neural balance of dopamine/ acetlycholine. Carbidopa/Levodopa TRADE NAME: Sinemet USEFUL DAILY DOSE: 200-1200 mg DRUG CLASS AND MECHANISM: Levodopa-carbidopa is a combination of two drugs, levodopa and carbidopa. When levodopa is taken orally, it crosses through the "blood- brain barrier." Once it crosses, it is converted to dopamine. The resulting increase in brain dopamine concentrations is believed to improve nerve conduction and assist the movement disorders in Parkinson disease. Carbidopa does not cross the blood-brain barrier. Carbidopa is added to the levodopa to prevent the breakdown of levodopa before it crosses into the brain. The addition of carbidopa allows lower doses of levodopa to be used. This reduces the risk of side effects from levodopa such as nausea and vomiting. This combination medicine was approved by the FDA in 1988. PHARMACOKINETICS: SinemetTM is administered orally. Following oral administration, amino acid transport mechanisms carry levodopa across the membrane of the GI tract, with approximately 30-50% of the drug entering the circulation. As a result, high concentrations of amino acids in the GI tract (i.e., a high- protein diet) can interfere with absorption of levodopa. Bioavailability of controlled-release preparations of levodopacarbidopa is approximately 71% compared with 99% for regular- release preparations. Levodopa-carbidopa distributes throughout the body, but due to peripheral metabolism, less than 1% of levodopa reaches the CNS; carbidopa does not penetrate the CNS. Approximately 95% of a dose of levodopa is metabolized to dopamine by L-aromatic amino acid decarboxylase in the stomach, intestines, and liver. Carbidopa is not appreciably metabolized. The onset of action of levodopa-carbidopa can be observed 2-3 weeks after therapy is initiated, but some patients require up to 6 months of therapy before beneficial effects are seen. The plasma half-life of both levodopa and carbidopa is roughly 1-2 hours, and the duration of action of a dose is 5 hours. Levodopa-carbidopa is eliminated renally as dopamine metabolites and small amounts as unchanged drug. DRUG INTERACTIONS: The use of amantadine (Symmetrel), benztropine (Cogentin), procyclidine (Kemadrin), or trihexyphenidyl (Artane) with levodopa-carbidopa can enhance the antiParkinson's effects of levodopa. Droperidol, haloperidol (Haldol), loxapine (Loxetine), metoclopramide (Reglan), phenothiazines such as prochlorperazine (Thorazine); thioxanthenes as thiothixene (Navane) inhibit dopamine in the brain. These drugs, therefore, can worsen Parkinson's disease and reverse the beneficial effects of levodopa. Methyldopa (Aldomet) and reserpine also can interfere with the beneficial actions of levodopa- carbidopa and can increase the risk of side effects. Phenytoin (Dilantin) can increases the break-down of levodopa- carbidopa, reducing its effectiveness. Use of levodopa-carbidopa with monoamine oxidase inhibitors (MAOI's) antidepressants, for example, isocarboxazid (Marplan), phenelzine (Nardil), tranylcypromine (Parnate), and procarbazine (Matulane), can result in severe and dangerous elevations in blood pressure. MAOI's should be stopped 2-4 weeks before starting levodopa-carbidopa therapy. The side effects associated with levodopa, including dizziness upon rising, confusion, movement disorders, nausea, and hallucinations, all can be increased by selegiline (Eldepryl). PREGNANCY: Although there are no human studies that have examined the effects of levodopa-carbidopa on the fetus, animal studies have shown adverse effects. Therefore, in prescribing levodopa- carbidopa for a pregnant woman, the physician must weigh the potential risks to the fetus against the potential benefits to the mother. Levodopa is also distributed into breast milk. It also may inhibit production of milk. It is generally recommended that levodopa-carbidopa should not be given to women who are breast- feeding. SIDE EFFECTS: Serious side effects with levodopa-carbidopa include difficulty passing urine, dizziness, lightheadedness or fainting spells, fast or irregular heartbeat (palpitations), mental depression, mood changes such as aggressive behavior or hallucinations, stomach pain, uncontrolled movements of the mouth, head, hands, feet, shoulders, eyelids or other unusual muscle movements, unusual bleeding or bruising, and unusual tiredness. Minor side effects include memory loss, anxiety, mental depression or euphoria, confusion, or nervousness, constipation, diarrhea, dry mouth, flushing of the skin, headache, loss of appetite, muscle twitches, nausea/vomiting, nightmares, trouble sleeping, and unusual tiredness or weakness. Infrequently, patients may develop a drop in white blood cell count during levodopa-carbidopa therapy. This is a cause to temporarily, if not permanently, stop treatment. Pergolide TRADE NAME: Permax USEFUL DAILY DOSE: 0.75-5.0 mg DRUG CLASS AND MECHANISM: Pergolide (PermaxTM ) can help correct an imbalance of chemicals in the brain thought to be responsible for Parkinson's disease. Pergolide helps to improve muscle control and movement difficulties. Pergolide will not cure Parkinson's disease, but will help to control the symptoms and slow down the progression of the disease. Pergolide tablets are taken together with other tablets that control parkinsonian symptoms. As a potent dopaminergic agonist, pergolide, taken orally, directly stimulates postsynaptic dopamine receptors in the nigrostriatal system. The dopamine-agonist properties of pergolide are not associated with presynaptic dopamine synthesis or stores; pergolide is an agonist at postsynaptic receptors. Pergolide is one of the most potent dopaminergic agonists. Unlike bromocriptine, pergolide stimulates both DA and DA receptors. Pergolide also causes less nausea and orthostatic hypotension than does bromocriptine and may be effective in patients who have become tolerant to bromocriptine. Pergolide is administered orally and is well absorbed. It is approximately 90% bound to plasma proteins. The drug undergoes metabolism to 10 metabolites, some of which are pharmacologically active. Elimination of the drug is primarily renal. The elimination half-life has been reported as 27 hours. DRUG INTERACTIONS: Pergolide is a potent dopamine-receptor agonist. Dopaminereceptor antagonists, including the neuroleptics (phenothiazines, haloperidol, and thiothixene), or metoclopramide should not be administered concurrently because they can antagonize the effects of pergolide. Other medicines that can interact with pergolide include medicines for mental problems and psychotic disturbances. Concomitant administration of amantadine, benztropine, procyclidine, or trihexyphenidyl with levodopa-carbidopa can enhance the therapeutic effects of levodopa but should not be used in patients with a history of psychosis. Droperidol; haloperidol; loxapine; phenothiazines; thioxanthenes (thiothixene and chlorprothixene); and possibly papaverine inhibit dopamine receptors in the brain, exacerbating parkinsonism and antagonizing the therapeutic effects of levodopa. Molindone can block dopamine receptors in the brain, interfering with the antiparkinsonian effects of levodopa and levodopa can antagonize the antipsychotic effects of molindone. Phenytoin can interfere with the effects of levodopa-carbidopa by enhancing the metabolism of the drug. The concomitant administration of bromocriptine with levodopa-carbidopa can result in additive effects that can be used to therapeutic advantage and allow for reduced dosages of levodopa-carbidopa. High-protein diets can interfere with the absorption of levodopa from the GI tract, thereby delaying its effects. Amino acids can compete with levodopa for transport into the brain, producing an erratic response to the drug. Concomitant use of monoamine oxidase inhibitors (MAOIs) with levodopa-carbidopa can result in hypertensive crisis. Simultaneous use of these agents is contraindicated. MAOIs should be discontinued 2-4 weeks before initiation of levodopa- carbidopa therapy. PREGNANCY: Pergolide is classified as pregnancy category B. No adequate studies have examined the effects of pergolide on the human fetus. Animal reproduction studies have shown no adverse fetal effects. SIDE EFFECTS: Serious side effects with pergolide include anxiety, restlessness, confusion, double vision, or other vision problems, fainting spells, hallucinations, headache, mental changes, palpitations, and uncontrollable movements of the arms, face, hands, head, mouth, shoulders, or upper body. Minor side effects with pergolide include constipation or diarrhea, difficulty sleeping, dizziness or drowsiness, flu-like symptoms (fever/chills/muscle aches), loss of appetite, lower back pain, chest or neck pain, nausea/vomiting, runny or stuffy nose, stomach pain, unusual weakness, and weight change. Bromocriptine TRADE NAME: Parlodel USEFUL DAILY DOSE: 3.75-40 mg DRUG CLASS AND MECHANISM: Bromocriptine (ParlodelTM ) comes from a group of medicines known as ergot alkaloids. It blocks the release of a hormone, called prolactin, that affects the menstrual cycle and breast milk production. Bromocriptine is useful in treating menstrual and fertility problems, and abnormal milk production. Bromocriptine can be used to treat Parkinson's disease. It is also helpful in treating acromegaly (excessive growth hormone). Related agents include pergolide and lisuride, which have 10 to 1000 times the potency of bromocriptine on a milligram basis. Bromocriptine stimulates dopamine type-2 receptors and antagonizes type-1 receptors in the hypothalamus and the neostriatum of the CNS. Pergolide, another ergot derivative, stimulates both type-1 and type-2 receptors. Prolactin secretion from the anterior pituitary gland is suppressed. Following bromocriptine-induced reductions in serum prolactin levels, ovulation and ovarian function will resume in amenorrheic patients, and lactation will be suppressed in women with normal ovarian activity. Bromocriptine also induces menses in amenorrheic women with normal levels of serum prolactin (possibly via the release of luteinizing hormone), and may have a direct stimulatory effect on ovarian dopaminergic receptors. Resumption of menses usually occurs within 6-8 weeks following administration of the drug. Patients with Parkinson's disease usually do not develop tolerance to the neurological effects of bromocriptine as they do to levodopa therapy. Bromocriptine also slightly increases sodium excretion and can reduce blood pressure. High doses of the drug can induce vasoconstriction. PHARMACOKINETICS: Although 28% of an orally administered dose of bromocriptine is absorbed across the GI tract, only 6% reaches the circulation due to significant hepatic metabolism. Oral administration of a single 1.25-5.0 mg dose results in serum prolactin reductions within 2 hours. Bromocriptine therapy produces maximal reductions in the serum prolactin levels of hyperprolactinemic patients within 4 weeks and significantly reduces growth hormone levels in acromegaly patients within 1-2 hours. The drug binds extensively (9096%) to serum albumin and does not appear to distribute into erythrocytes. More than 90% of an absorbed dose undergoes first-pass metabolism, with the remainder of the dose hydrolyzed in the liver to inactive metabolites. Bromocriptine has a half-life of 3 hours. Metabolites are eliminated in the bile, with only a small amount excreted by the kidneys. PREGNANCY: Bromocriptine is pregnancy risk category C. Although no adequate human studies have been performed on the effects of this drug on the fetus, animal reproduction studies have shown adverse fetal effects. Therefore, in making the decision to administer this drug during pregnancy, the potential risks to the fetus must be weighed against the potential benefits to the mother. Bromocriptine should not be given to patients planning to breast-feed. Bromocriptine interferes with lactation and therefore should not be used during breast-feeding. Bromocriptine can cause hypotension and should not be administered during the postpartum period unless vital signs are normal and at least 4 hours have passed. DRUG INTERACTIONS: Drugs that increase the concentration of prolactin, such as butyrophenones including haloperidol; loxapine; molindone; monoamine oxidase inhibitors (MAOIs); imipramine; amitriptyline; methyldopa; phenothiazines; thioxanthines; and reserpine, can antagonize the effects of bromocriptine. Estrogens or progestins can produce amenorrhea or galactorrhea when administered, and use during bromocriptine administration is not recommended. High doses of bromocriptine can decrease the tolerance to ethanol, so patients should be warned of this effect and advised to lessen ethanol consumption while receiving bromocriptine. A disulfiram-like reaction can occur during concomitant use of bromocriptine and ethanol, which is manifested as chest pain, tachycardia, throbbing headache, flushing of the face, severe weakness, sweating, nausea, vomiting, and blurred vision. Bromocriptine and levodopa are both dopamine agonists. Concomitant use of these agents can cause additive neurologic effects. Although this drug combination may be necessary in some patients, dosages of levodopa may require reduction if bromocriptine is added. Case reports have documented hypertension and seizures occurring as a result of concomitant use of bromocriptine and phenylpropanolamine. Until more data are available, this drug combination should be avoided whenever possible. SIDE EFFECTS: Large doses of bromocriptine can cause mental status changes including confusion, so the drug should be used with extreme caution in parkinsonian patients who exhibit signs of dementia. Hallucinations can develop in patients receiving bromocriptine alone or in combination with levodopa. Dosage reduction usually eliminates these hallucinations, but discontinuation of the drug may be required. Prolonged therapy with bromocriptine has resulted in the development of pulmonary infiltrates, thickening of the pleura, and pleural effusion. Serious side effects with bromocriptine include blurred vision, confusion or hallucinations, difficulty breathing, fainting spells, dizziness or lightheadedness, irregular heartbeat, chest pain or palpitations, persistent and watery nasal discharge, seizures (convulsions), and weakness or tiredness. Minor side effects include diarrhea or constipation, drowsiness, dry mouth, headache, loss of appetite, nausea, vomiting, runny nose, or stuffy nose, and stomach pain. Selegiline TRADE NAME: 1-Deprenyl-Eldepryl USEFUL DAILY DOSE: 2.5-10 mg DRUG CLASS AND MECHANISM: Selegiline (EldeprylTM ), also commonly known as deprenyl or deprenil, helps to increase or extend the effects of levodopa or carbidopa, and slow the progression of Parkinson's disease. Selegiline belongs to a class of drugs, called monoamine oxidase inhibitors (MAOIs), that block certain enzymes in the brain and change the balance of certain chemicals in the brain. Selegiline is an oral agent used in the treatment of idiopathic Parkinson's disease, in combination with levodopa or levodopa and carbidopa. Due to its selectivity for MAO type B, selegiline is purported to possess fewer drug interactions and a lower risk of hypertension than phenelzine (Nardil TM ). In controlled clinical trials, selegiline caused slight improvement in motor performance at the start of therapy and worsening at its discontinuance; it also delayed the development of disability that requires the addition of levodopa. Selegiline is a noncompetitive antagonist of monoamine oxidase type B (MAO-B), the main form of this enzyme in the human brain. Monoamine oxidase type B is responsible for the oxidative deamination of dopamine in the brain. Blockade of this enzyme reduces the metabolism of dopamine, decreases free radical production, and potentiates the effects of administered levodopa. It is unknown whether the benefits seen in Parkinson's disease occur from increased dopaminergic transmission or from a decreased rate of neuronal death due to free radicals. Selegiline doses of 10 mg/day block essentially all the MAO-B in the adult brain. Selegiline's duration of action depends on the time required to regenerate MAO type B At higher selegiline doses (e.g., 20-40 mg/day), brain MAO is blocked nonselectively, predisposing patients to the risks of traditional MAOIs that block MOA type A (e.g., hypertension). Like phenelzine, the effects of selegiline are cumulative, with beneficial effects seen in a few days to several months. PHARMACOKINETICS: Selegiline is administered orally and is readily absorbed from the GI tract and crosses the blood/brain barrier. Peak serum concentrations are found in 0.5-2 hours. The drug is rapidly and completely metabolized to three active derivatives with the following half-lives: N-desmethyldeprenyl, 2 hours; 1-amphetamine, 17.7 hours; and 1methamphetamine, 20.5 hours. Selegiline is eliminated slowly by the kidneys; about 45% of a single 10 mg dose is eliminated in the urine as the three active metabolites in 48 hours. PREGNANCY: Selegiline should be used cautiously in pregnant women. The effects on the fetus during pregnancy are not known. DRUG INTERACTIONS: Selegiline is a monoamine oxidase inhibitor. In general, tricyclic antidepressants should be used cautiously, if at all, in patients receiving drugs with monoamine oxidase inhibitor (MAOI) activity. Although at low doses selegiline is selective for MAO type B, in doses above 30-40 mg/day, this selectivity is lost. Selegiline, despite its selectivity, can provoke serious CNS reactions in patients receiving either tricyclic antidepressants (clomipramine, desipramine, etc.) or fluoxetine. Concomitant administration of selegiline and fluoxetine can cause mania and the development of a serotonin syndrome (characterized by hyperthermia, diaphoresis, shivering, tremor, myoclonus, seizures, ataxia, delirium, restlessness). Concurrent use of selegiline with fluoxetine is not recommended because of this rare, but serious reaction. At least 2 weeks should pass between the last dose of a MAO inhibitor and the first dose of fluoxetine. However, at least a 5-week interval is needed between the last dose of fluoxetine and initiation of MAO-inhibitor therapy because of the prolonged elimination of fluoxetine. It is unclear if selegiline interacts similarly with other member of the selective serotonin reuptake inhibitors (SSRIs). Administration of levodopa to patients receiving drugs that inhibit monoamine oxidase (MAO) can produce a hypertensive response. While traditional MAOIs such as phenelzine inhibit MAO type A and selegiline is selective for MAO type B, at doses above 30-40 mg/day, this selectivity is lost. Selegiline can increase levodopa-induced dyskinesias, nausea, orthostatic hypotension, confusion, and hallucinations. Reductions in levodopa dosage may be necessary within a few days after the start of selegiline treatment. Even though Parkinson's disease is an indication for both selegiline and levodopa, and these 2 drugs may be administered together safely in some cases, patients should be monitored closely for hypertensive responses, especially if selegiline doses higher than 10 mg/day are used. At doses of 20 mg/day, selegiline can interact with foods and beverages containing high concentrations of pressor amines such as tyramine. Sudden and severe hypertensive reactions are possible. This reaction is believed to be a result of selegiline's effects on MAO type A, which occurs at higher doses. Dietary restrictions should be observed for at least 2 weeks after the last dose of any MAO inhibitor. Other catecholamine-releasing or sympathomimetic agents (e.g., ephedrine, phenylpropanolamine) may induce drug interactions with selegiline at higher doses. SIDE EFFECTS: Serious side effects with selegiline include black, tarry stools, changes in behavior (mood swings, irritability, confusion, agitation), chest pain, difficulty breathing, difficulty speaking, enlarged pupils, fever, clammy skin, increased sweating, hallucinations, headaches, lightheadedness or fainting spells, loss of balance, muscle or neck stiffness or spasms, slow/fast or irregular heartbeat (palpitations), uncontrollable muscle movements or spasms of the head, face, arms, or legs. Minor side effects include anxiety or nervousness, blurred vision, increased sensitivity of the eyes to light, changes in taste, constipation or diarrhea, difficulty sleeping, drowsiness or dizziness, dry mouth, loss of appetite, weight loss, muscle aches or pains, nausea/vomiting, ringing in the ears, stomach discomfort or pain, and unusual tiredness or weakness. Do not treat yourself for coughs, colds, or allergies without asking your doctor or pharmacist for advice. Some ingredients may increase possible side effects to selegiline. Selegiline may cause the feet and legs to swell because of peripheral edema. Amantadine TRADE NAME: SymmetrelTM\ USEFUL DAILY DOSE: DRUG CLASS AND MECHANISM: AMANTADINE (SymmetrelTM ) is an antiviral agent. Amantadine prevents or treats certain influenza (flu) infections. It is not an effective treatment for colds or other viruses. Amantadine can improve muscle control and reduce muscle stiffness in patients with Parkinson's disease (shaking palsy) or similar movement disorders. It was introduced as an agent for prophylaxis of influenza A and was later found to cause symptomatic improvement in parkinsonism. Amantadine's mechanism of action is not fully understood. Antiparkinsonian actions are unrelated to the antiviral effects. Amantadine appears to potentiate CNS dopaminergic responses. It may release dopamine and norepinephrine from storage sites and inhibit the reuptake of dopamine and norepinephrine. Amantadine is clearly less effective than levodopa but can offer additional benefit in patients experiencing maximal or waning effects from levodopa. As an antiviral, amantadine can inhibit viral replication within the viral cell. Amantadine appears to block the uncoating of the virus particle and subsequent release of viral nucleic acid into the host cell. It also may interfere with penetration of the cell wall by adsorbed virus. To prevent a viral infection, the drug should be present before exposure to the virus, but, if given within 24-48 hours of onset of symptoms, the influenza may be less severe. PHARMACOKINETICS: Amantadine is administered orally. Absorption from the GI tract appears to be rapid and complete. Bioavailability is 86% in the elderly and greater than 90% in young adults.• Peak plasma concentrations are achieved in about 2-4 hours following oral administration. Steady-state concentrations following daily dosage are obtained in 2-4 days. Amantadine crosses the blood-brain barrier and the placenta; distributes into tears, saliva, and nasal secretions; and is excreted into breast milk. Ninety percent of amantadine is excreted in the urine via glomerular filtration and tubular secretion. Renal impairment reduces protein binding. The elimination half-life in patients with normal renal function is about 11-15 hours but can be as long as 7-10 days for those with severe renal impairment. Half- life in elderly patients is 24-29 hours. Acidifying the urine increases the rate of excretion. Only a small amount of amantadine is removed by dialysis. Because amantadine is primarily excreted unchanged in the urine, patients with renal impairment should receive lower doses. PREGNANCY: Amantadine is classified as a pregnancy category C drug. No complete or well-controlled studies have been done. Use during pregnancy should be avoided unless the potential benefits outweigh the possible risks to the fetus. DRUG INTERACTIONS: Ethanol should not be used with amantadine because of the possible increase of CNS effects such as dizziness, confusion, lightheadedness, fainting, or orthostatic hypotension. Amantadine should be used with caution with anticholinergics, tricyclic antidepressants, antihistamines, or phenothiazines because of the possible increase of anticholinergic effects, especially hallucinations, nightmares, or confusion. Reductions in the dosage of both drugs may be necessary before using them together. Amantadine can increase the efficiency of levodopa by its action on central nerve terminals. Patients who exhibit psychoses should avoid this combination because of the possibility of an increased psychotic effect. Amantadine used concomitantly with CNS stimulants can result in increased stimulant effects, such as nervousness, irritability, or insomnia, and can lead to seizures or cardiac arrhythmias. Close monitoring of the patient is recommended. SIDE EFFECTS: Serious side effects with amantadine include changes in vision, depression or thoughts of suicide, difficulty passing urine, fainting spells or lightheadedness, hallucinations, movement difficulties, purplish spots or network on the skin, seizures, swelling of the feet or legs. Minor side effects with amantadine include anxiety, irritability, nervousness, diarrhea or constipation, difficulty sleeping, or nightmares, drowsiness, dry mouth, headache, loss of appetite, unusual tiredness. If you are taking amantadine for a movement disorder, do not suddenly stop taking it. You may get muscle stiffness, paralysis, confusion, or find it difficult to pass urine. If you are taking amantadine for Parkinson's disease, be careful not to overdo physical activity as your condition improves. Gradually increase activity so that your body has time to adjust. Abrupt withdrawal of amantadine should be avoided in patients with Parkinson's disease since this may precipitate symptoms of increased rigidity, confusion, urinary retention, or bulbar palsy.