Supplementary Materials and Methods (doc 52K)
advertisement

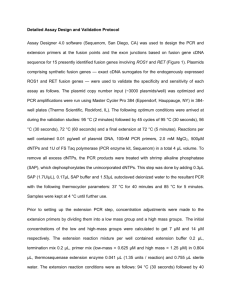
SUPPLEMENT Materials and Methods Case selection From the Tokyo Children’s Cancer Study Group (TCCSG) bioresources, we selected RNA samples obtained from 401 pediatric acute lymphoblastic leukemia (ALL) patients consisted of three subcohorts. The first subcohort is an uncontinuous series of randomly selected 42 BCP-ALL patients without conventional cytogenetic abnormalities. Most of the patients were newly diagnosed with ALL while some relapsed patients were also included. The second one is a continuous series of newly diagnosed 333 pediatric ALL patients enrolled in the TCCSG L0416/0616 study from December 2004 to July 2007. This group include 41 T-ALL, 1 unclassified ALL, and 291 BCP-ALL patients consisted of 15 BCR-ABL1+, 17 E2A-PBX1+, 53 ETV6-RUNX1+, 3 MLL-AF4+, 2 MLL-AF9+, 65 hyperdiploid, 3 hypodiploid, and 133 BCP-ALL patients without conventional cytogenetic abnormalities (unpublished data). The third subcohort include 26 BCP-ALL without conventional cytogenetic abnormalities selected from outside the L0416/0616 cohort by means of the dull or negative expression of CD10. To investigate unknown fusion genes, whole transcriptome sequencing was performed on RNA samples obtained from 55 pediatric BCP-ALL patients without conventional cytogenetic abnormalities including entire patients of the first subcohort and 13 patients randomly selected from the second subcohort. To estimate the frequency of fusion gene being newly identified, RNA samples obtained from remaining patients of the second subcohort were used for screening with RT-PCR. Since all four EP300-ZNF384+ cases identified in the first and second subcohorts revealed dull or negative expression of CD10 based on immunophenotypic examination, we screened a further 26 of CD10-dull or -negative BCP-ALL cases without conventional cytogenetic abnormalities (the third subcohort) by RT-PCR to find out another cases with fusion gene being newly identified. Diagnoses were made on the basis of the morphology and routine examinations, including immunophenotyping, cytogenetic analysis, DNA contents analysis, and the real-time PCR detection of 8 fusion transcripts: MLL-AF4, MLL-AF9, MLL-ENL, major BCR-ABL1, minor BCR-ABL1, ETV6-RUNX1, E2A-PBX, and SIL-TAL1, as described previously.1 The investigations were approved by the institutional review boards of all participating institutions. Informed consent was obtained from parents or guardians, and informed assent was obtained from the patients when appropriate based on their age and level of understanding.1 Whole transcriptome sequencing and detection of fusion genes Total RNAs were extracted from bone marrow-derived leukemic cells of the patient using the miRNeasy Mini Kit (Qiagen, Valencia, CA, USA) and whole transcriptome sequencing was performed, as described previously.2,3 Briefly, after qualification using Agilent RNA 6000 Nano Kit (Agilent Technologies, Santa Clara, CA, USA), cDNA libraries were prepared from 1 g of total RNA by using the TruSeq RNA sample preparation kit v2 (Illumina, Inc., San Diego, CA, USA, catalog # RS-122-2001). The resultant libraries were quantified using KAPA Library Quantification Kit (KAPA Biosystems, Inc., Woburn, MA, USA, catalog # KK4835) and checked for quality and size using Agilent High Sensitivity DNA Kit (Agilent, catalog # 5067-4626). The samples were loaded on to the cBot (Illumina) for clustering on a flow cell, the flow cell was then sequenced using a HiSeq1500 (Illumina) according to manufacturer’s instructions. A paired-end (2 x 101) run was performed using the SBS Kit v3-HS (Illumina, catalog # FC-401-3001). At least 30,000,000 reads were obtained for each sample. To avoid multiple counting of each fusion transcript, RNA sequencing data were used after removal of paired-end reads with the identical nucleotide sequence, which had probably been derived from PCR duplicates during library preparation. For prediction of fusion genes, the deFuse program5 was used as described previously.6 After applying default filtering of this program, potential alternative splicing and read-through products that the program predicted were eliminated, and candidates that had exon boundary junctions were selected. EP300-ZNF384 fusion was supported by 39 spanning reads and 146 split reads in case-1 and by 52 spanning reads and 68 split reads in case-2. RT-PCR For detection of the EP300-ZNF384 fusion transcript, PCR was carried out as described previously4 and a 372-bp fragment was amplified using the following primers: EP300-forward-S3, 5’-tctaggggtgggtcaacagt-3’ 5’-ctgtcagcaaggtggggtag-3’. and ZNF384-reverse-AS3 Sanger sequencing of the PCR products was performed as described previously.3 Fluorescence in situ hybridization (FISH) analysis Dual color FISH analysis was performed on bone marrow specimens obtained from Case 1 using the bacterial artificial chromosome (BAC) clones RP11-958C6 (labeled with Green-dUTP, Abbott Laboratories, Abbott Park, IL, USA) and RP11-1137P19 (labeled with Orange-dUTP, Abbott), including EP300 and ZNF384 genes, respectively (http://genome.ucsc.edu/cgi-bin/hgGateway). By employing standard techniques, 1,000 cells were examined. Japan). Actual examinations were performed by LSI Medience Corporation (Tokyo, References for Materials and Methods 1 Kiyokawa N, Iijima K, Tomita O, Miharu M, Hasegawa D, Kobayashi K, et al. Significance of CD66c expression in childhood acute lymphoblastic leukemia. Leuk Res 2014; 38: 42-48. 2 Kobayashi K, Mitsui K, Ichikawa H, Nakabayashi K, Matsuoka M, Kojima Y, et al. ATF7IP as a novel PDGFRB fusion partner in acute lymphoblastic leukaemia in children. Br J Haematol 2014; 165: 836-841. 3 Masuzawa A, Kiyotani C, Osumi T, Shioda Y, Iijima K, Tomita O, et al. Poor responses to tyrosine kinase inhibitors in a child with precursor B-cell acute lymphoblastic leukemia with SNX2-ABL1 chimeric transcript. Eur J Haematol 2014; 92: 263-267. 4 Tomita O, Iijima K, Ishibashi T, Osumi T, Kobayashi K, Okita H, et al. Sensitivity of SNX2-ABL1 toward tyrosine kinase inhibitors distinct from that of BCR-ABL1. Leuk Res 2014; 38: 361-370. 5 McPherson A, Hormozdiari F, Zayed A, Giuliany R, Ha G, Sun MG, et al. deFuse: an algorithm for gene fusion discovery in tumor RNA-Seq data. PLoS Comput Biol 2011; 7: e1001138. 6 Gotoh M, Ichikawa H, Arai E, Chiku S, Sakamoto H, Fujimoto H, et al. Comprehensive exploration of novel chimeric transcripts in clear cell renal cell carcinomas using whole transcriptome analysis. Genes Chromosomes Cancer 2014; 53: 1018-1032. Legends to supplementary Figures and Table Supplementary Figure 1. (A) The EP300-ZNF384 fusion transcripts were amplified by RT-PCR. In Case 1, the presence of EP300-ZNF384 fusion gene was only confirmed in the samples obtained at 2nd and 3rd relapse, because of unavailability of the samples at initial diagnosis and 1st relapse. As an internal control, the human GAPDH gene was also detected. Lane 1, molecular weight marker; Lanes 2-8, patient RT–PCR products as indicated. (B) The result of Sanger sequencing of the PCR product obtained from Case 1 (at 2nd relapse) is indicated. The PCR products obtained from the other patients showed identical sequences. Supplementary Figure 2. Histograms of CD19, CD10, and aberrant myeloid antigens (CD13 and CD33) of EP300-ZNF384 fusion gene-positive cases (Cases 1-6) are indicated with a positive rate (%). As a control, histograms of a typical CD10-positive B-cell precursor acute lymphoblastic leukemia case (CD10+Cnt) are also shown. X-axis, fluorescence intensity; Y-axis, relative cell number. Supplementary Table. Immunophenotypes of patients. Immunophenotypic features of patients with the EP300-ZNF384 fusion gene are summarized.