Improving Responsiveness to Maori with Chronic Conditions
advertisement

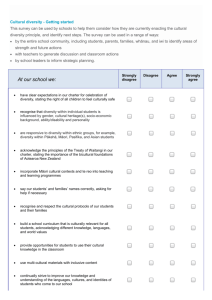
DISCUSSION PAPER IMPROVING RESPONSIVENESS TO MĀORI WITH CHRONIC CONDITIONS EXPERT WORKING GROUP MEETING 4 MAY 2010 CONTENTS CONTENTS 2 SECTION ONE: RESEARCH 3 PURPOSE OF THIS SECTION CHRONIC CONDITIONS MĀORI AND CHRONIC CONDITIONS BARRIER TO SERVICE FOR MĀORI SOCIOECONOMIC STATUS Examples of socioeconomic statistics PROVIDER COMMUNICATION PATIENT KNOWLEDGE EXPERIENCES OF MĀORI PATIENTS WHĀNAU ASSITING WITH CARE 3 3 4 5 6 6 6 7 8 8 SECTION TWO: EXAMPLES OF CURRENT MODELS 10 PURPOSE OF THIS SECTION COUNTIES MANUKAU CHRONIC CARE MANAGEMENT PROGRAMME THE NGATI AND HEALTHY PREVENT DIABETES COMMUNITY PROGRAMME (NGATI POROU HAUORA, TAIRAWHITI) THE MĀORI CASE MANAGEMENT CLINIC PROJECT 2001-2003 (RAUKURA HAUORA O TAINUI, CLENDON, AUCKLAND) KIA RITE, KIA ORA MODEL (WHAIORA WHANUI TRUST, MASTERTON) GET CHECKED GREEN PRESCRIPTIONS (GRX)/TE RONGOAA KAKARIKI ONE HEART MANY LIVES, PHARMAC SECTION THREE: DISCUSSIONS 16 PURPOSE OF THIS SECTION SUMMARY STRENGTHENING WHĀNAU KNOWLEDGE OF HEALTH AND PREVENTION IMPROVING SERVICE RESPONSIVENESS THROUGH COORDINATED CARE SUPPORTING THE ROLE OF THE WHĀNAU IN SELF MANAGEMENT IMPROVING COMPLEX CARE (CASE MANAGEMENT) STRENGTHENING AND SHARING SUCCESSFUL MĀORI MODELS OF HEALTH 16 16 18 18 19 20 20 APPENDIX ONE: MINISTRY DIRECTION 21 PURPOSE OF THIS SECTION MINISTRY OF HEALTH STRATEGIC DIRECTION FOR MĀORI HEALTH Figure 1:Overarching framework of He Korowai Oranga: The Māori Health Strategy THE GOVERNMENT’S HEALTH TARGETS Table 1: Health Targets and how they are measured THE DIABETES AND CARDIOVASCULAR DISEASE QUALITY IMPROVEMENT PLAN (QIP) 21 21 22 23 24 24 25 APPENDIX 2: IDENTIFIED KEY GROUPS 26 TE HOTU MANAWA MĀORI MĀORI PHO COALITION TE ROOPU MATE HUKA TE OHU RATA O AOTEAROA (TE ORA): MĀORI MEDICAL PRACTITIONERS ASSOCIATION OF AOTEAROA/NEW ZEALAND HAUORA.COM (NATIONAL MĀORI HEALTH WORKFORCE DEVELOPMENT ORGANISATION) TUMU WHAKARE (NATIONAL REFERENCE GROUP OF MĀORI HEALTH STRATEGY MANAGERS WITHIN DHBS) BEST PRACTICE ADVOCACY CENTRE (BPAC) Maori Innovation Fund 10 10 11 11 12 13 14 15 Date: 27 Aug 09 Version: 2 Page 2 of 29 26 26 26 27 27 27 27 SECTION ONE: RESEARCH Purpose of this section This section provides you a summary of relevant research on Māori and Chronic Conditions. Chronic Conditions Chronic conditions or long-term conditions are those that can only be controlled but not, at present, cured. Some common long-term conditions are: alcohol and other addictions alzheimer and other dementias asthma arthritis cancer cardiovascular disease chronic obstructive pulmonary disease (COPD) chronic pain congestive heart failure depression and anxiety disorders diabetes stroke. There are many other long-term conditions, including rare conditions with a genetic origin and oral health conditions. Unlike acute illness, most long-term conditions develop over longer periods of time, sometimes having their origins antenatally. They do not always have a clear point of onset, and may have multiple causes, including genetic inheritance that can be modified through early life experience. Accidents and injuries can also result in long-term conditions requiring ongoing health care and support and management, such as chronic pain, depression and the effects of head injury. Often people have more than one long-term condition (referred to as co-morbidities or multiple morbidities). Some long-term conditions cause other long-term conditions, while others can be the result of acute illnesses. Long-term conditions that arise in childhood and adolescence may be more advanced or severe in adulthood, unless they are well managed in the early stages. In New Zealand: An estimated 70% of health care funds are spent on chronic conditions. 80% of all deaths in NZ result from chronic conditions. Chronic conditions contribute the major share of the disparity in life expectancy between Māori and non-Māori. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 3 of 29 All New Zealanders are affected by chronic conditions – whether as carers for family and whānau, taxpayers, health professionals or managing their own chronic condition. Where New Zealand specific research is available, most cost of illness studies on longterm conditions report annual societal costs greater than $100 million. In New Zealand intangible costs tend to be estimated in the billions, for example, intangible costs were estimated at over $2.5 billion for arthritis in 2005 and over $9 billion for dementia in 2008. Where they exist, cost of risk factor studies, including for tobacco use, physical inactivity and obesity, report annual societal costs of over $800 million. There are no studies on the overall economic cost of all long-term conditions in New Zealand. Although the costs of these conditions and risk factors can not be entirely eliminated, they do, however, highlight the vast investment in the management of long-term conditions. Understanding these costs can help to inform how best to invest resources. Mismanagement of chronic conditions is the leading cause of hospitalisations, accounts for 80 percent of all preventable deaths and is estimated to consume a major proportion of our health care funds. Chronic conditions are also a barrier to independence, participation in the workforce and in society – social and economic costs we are yet to calculate as a nation. Māori and Chronic Conditions Chronic conditions account for a higher proportion of illness and deaths among Māori, people on low incomes and Pacific peoples than among the general population. The need to reduce health inequalities remains urgent. Although there has been a consistent increase in life expectancy among Māori and nonMāori since the 1950s, an 8.5 year gap in life expectancy remains. In 2002, a newborn Māori boy could expect to live 69 years, compared with 77.2 years for a non-Māori boy. At birth, a Māori girl could expect to live 73.2 years compared with 81.9 years for a nonMāori girl (Statistics New Zealand 2004). A range of data suggests that differences in health outcomes for Māori arise, in part, from differences in health care received. When compared with people of European descent within the same income range, Māori were significantly less likely to have seen a doctor when sick, received recommended tests, or filled a prescription. Cost was a significant contributor (Schoen et al 2004a). Māori hospital patients have a higher risk of preventable, adverse effects than non-Māori, non-Pacific patients (Davis et al 2006). There is increasing evidence that Māori do not receive comparable health management across a range of chronic conditions. For example, Māori have significant difficulties in receiving expert help for asthma when needed, have more severe and more poorly managed asthma, and higher hospitalisation rates than non-Māori (Ministry of Health 1999). Māori are less likely to be referred for surgical and specialist services, and are more likely to receive lower than expected levels of quality hospital care than Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 4 of 29 non-Māori (Ellison-Loschmann and Pearce 2006). For example, in both diabetes (Baxter 2002) and cardiac interventions (Westbrook et al 2001), Māori receive less intervention and treatment. The higher mortality rate for Māori (Robson et al 2006) with diagnosed cancer suggests that either diagnosis has been delayed or referral and treatment processes are inequitable. Barrier to Service for Māori Considerable local and international evidence about inequalities in health has become available in the last decade (MOH 2002; Smedley et al 2002; Robson & Harris 2007). Health inequalities occur between population groups according to numerous factors, including cultural and historical, socio-economic status, geographical place of residence, ethnic identity, and gender. Internationally, researchers have identified both barriers to, and facilitators of, access to health care for minority patients in their search for explanations for health disparities. New Zealand studies have similarly identified organisational, human resource, and patient-community issues in access to health care. At the organisational level barriers include: the timing and availability of services, the universal, Western approach to health care, the under-representation of Māori in the health professions, appointment systems, and the lack of appropriate educational and promotional material. At the human resource level barriers include: the characteristics of non-Māori health staff, including their perceptions of and attitudes about Māori patients; and appropriate provider-patient communication, or lack thereof. At the individual or community level barriers include: the socio-economic position of many Māori which makes healthcare unaffordable; and patient attitudes, beliefs and preferences which may make healthcare inappropriate, feared and/or not a priority. Patient feedback about their satisfaction with health care providers can provide valuable information about barriers to, and facilitators of, healthcare which, in turn, can aid clinicians in their ability to provide accessible healthcare to Māori. Patient knowledge, attitudes, beliefs, values, and preferences are also associated with access to care. Attitudes to health care are often informed by people’s past experiences and/or the experiences of their whānau and others close to them (Cram et al 2003). Previous negative experiences with the healthcare system and/or perceptions of bias, such as non-Māori health services not being seen as acceptable or clients hearing negative comments from others, can prevent people from accessing health care (Bryant & Campbell 1996; Health Waikato 2001). Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 5 of 29 Socioeconomic status Evidence on socioeconomic mortality trends in New Zealand (Ministry of Health and University of Otago 2006) shows that, compared with the general population, those with low incomes experience higher mortality rates from major chronic illnesses. Lifestyle behaviours, psychosocial stress and health system performance all have an effect on health. These factors are influenced by socioeconomic status, which in turn has some relationship with ethnicity. The interaction among this interplay of factors is not straightforward. For example, smoking, the most influential modifiable risk behaviour, is more prevalent among those on a lower income. But recent research on contributors to health inequalities found that the contribution smoking makes to ethnic disparities in mortality is probably less than 10 percent. Socioeconomic factors contribute an additional 32 to 39 percent (Blakely et al 2006). People on low incomes are more likely to develop chronic conditions. Furthermore, since chronic conditions have significant financial impacts that extend beyond direct medical costs, households on low incomes are likely to enter cycles of poverty and ill health. For example, living standards are lower among families with high numbers of doctor visits for child illness; families are restricted in their social and economic participation because of a child’s serious health conditions (Ministry of Social Development 2004). There are also cumulative effects on health from psychosocial stressors (Seeman et al 2004). Examples of socioeconomic statistics Between 1981 and 1999, Māori were disproportionately represented in lower socioeconomic strata and consequently disproportionately affected by the health consequences of lower socioeconomic status. Māori to non-Māori inequalities in mortality persist within socio-economic strata and socioeconomic gradients in mortality exist within both Māori and non-Māori ethnic groups. The different socioeconomic resources or position of Māori and non-Māori/nonPacific groups account for at least half of the ethnic disparities in mortality for working age adults and one-third for older adults. Widening inequalities in socioeconomic resources between these groups during the 1980s and 1990s explained about one third to a half of the widening in the mortality disparity (for people of working age) (Ministry of Health and University of Otago 2006). From 1992-2002, the number of sickness beneficiaries in New Zealand rose from around 30,000 to 40,000, while the number of people on the invalids benefit doubled (Ministry of Social Development 2005). Increases not attributable to population growth, population ageing and rise in age of superannuation, are associated with mental illness and musculoskeletal incapacities for the majority of New Zealand. Provider communication There is growing evidence that the quality of communication between Māori and health professionals affects health outcomes for Māori (Penney 2005). This evidence offers an insight into barriers to accessing health services for Māori. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 6 of 29 Māori feel respected in mainstream health care services when they are able to relate to and make sense of the advice from their doctor (Cram et al 2003; Jansen 2006). Poor communication may contribute to Māori, especially women, being less likely to visit a GP than non-Māori, which in turn increases the likelihood they will go to the doctor only when in need of urgent attention (Crengle et al 2005). Non-Māori doctors have reported ‘lower levels of rapport’ with Māori patients (Jansen 2006). This may be a reason for doctors’ shorter mean consultation times for Māori (Crengle et al 2005). Māori receive significantly less treatment for depression and even lower payments from ACC than non-Māori (Jansen 2006). Differential access through the health system is cumulative and contributes to earlier and higher mortality rates overall for Māori. Patient Knowledge In 2006, New Zealand and other countries participated in the Adult Literacy and Lifeskills Survey (ALL). The ALL measured the prose literacy, document literacy, numeracy and problem solving skills of respondents aged 16 to 65 years. From this data, information relating to respondents’ health literacy was derived using specific questions related to health issues. The Ministry has completed an analysis of the ALL health literacy data and produced a report titled ‘Kōrero Mārama: Health Literacy and Māori’. The report describes the health literacy skills of Māori compared to non-Māori. The report presents findings by gender, rural and urban location, age, level of education, labour force status and household income. The report shows that on average New Zealanders have poor health literacy skills. Some groups have even poorer health literacy, including Māori, the elderly, and those on low income. Māori were found to have poorer health literacy skills compared to non-Māori across all of the measured variables. Eighty percent of Māori males and 75 percent of Māori females were found to have poor health literacy skills. Māori who lived in a rural location had on average the poorest health literacy skills by geographic location. Māori in the 5065, 16-18 and 19-24 year age groups had the poorest health literacy compared to the rest of the population. People with poor health literacy skills are at greater risk of experiencing poor health outcomes. People with poor health literacy are less likely to: recognise the first signs of medical problems, access health care services, communicate well with health professionals, understand health information and instructions, and sufficiently manage their long-term/chronic condition. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 7 of 29 People with poor health literacy skills also incur higher health care costs both for themselves and the system as they are: less likely to use prevention services and therefore enter the health system for treatment, less likely to have the skills to manage their medication which can have serious health implications and cause wastage, are more likely to use emergency services, and are more likely to visit and be admitted to hospital with preventable cases. Experiences of Māori patients In the 2007 National Advisory Committee on Health and Disability report on Meeting the Needs of People with Chronic Conditions, and series of case studies were conducted on service performance. The Māori case study articulated the value of family/whānau involvement. This was not only reflected in whakapapa whānau but also with ‘whānau’ acquired through social services. An essential element of care according to the Māori case study is including the whole whānau. In this way all issues affecting the whānau are covered, not just the immediate needs of the person with the chronic conditions. Nor is whānau restricted to family. One example was given where a ropu rangatahi included koroua and kuia in their waka outing. The strength of this is that the koroua and kuia are able to provide wisdom that may benefit the rangatahi. This takes account of the wairua aspect of health. Not having families/whānau present at significant health assessments led to miscommunication within families/whānau about the needs of people with chronic conditions. Additionally, not involving the family/whānau in care planning meant that someone with a chronic condition might not be able to keep an appointment if they were dependent on family/whānau for transport. The Māori felt that health care professionals take little account of whānau as an integral part of their health and treatment process. Whānau assiting with care There are strong arguments for health professionals to have greater involvement with family/whānau in providing care to people with chronic conditions. Greater involvement is a key way in which relationships with providers can be built to increase access for Māori and Pacific peoples. It results in significant impacts on health and wellbeing for the person with a chronic condition. Greater involvement is culturally appropriate. However, regardless of which culture a person comes from, the support of family/whānau and friends is needed by people with chronic conditions for practical assistance and wellbeing. Involving whānau in support for self-management increases the likelihood that healthy behaviour will be adopted. Since family and whānau members are likely to have similar risk factors to the person with the chronic condition, involving family/whānau is a sound preventative approach. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 8 of 29 Research has made it clear that people with chronic conditions needed and valued the practical assistance given by family and friends with transport, history-taking at appointments, daily-living tasks and complex medication or monitoring routines. There is a growing awareness of the burden placed on whānau emphasising the needs of a person’s whānau had to be considered and supported. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 9 of 29 SECTION TWO: EXAMPLES OF CURRENT MODELS Purpose of this section This section provides examples of current programme to improve the responsiveness to Chronic Conditions. Counties Manukau Chronic Care Management Programme Counties Manukau DHB use a chronic care model to provide the framework for a number of chronic conditions programmes or initiatives spanning a person’s life course from prevention to palliative care. The model and associated programmes were developed to seamless care to targeted patients with specific chronic diseases need (ranging from low to very high). Underlying the model are principles of all chronic care models including: population health centred care, involvement of family/whanau, multidisciplinary communication and information-sharing. consistently deliver and varying levels of key approaches and approaches, personteamwork, effective Initiatives within the chronic care model are determined by regional strategic priorities and plans as well as objectives from the national health and disability strategies. Individual disease projects are aligned to the model. A significant initiative set within the framework is the Chronic Care Management programme (CCM). The CCM is the first structured chronic care management programme to be developed and evaluated in New Zealand. Key components of the CCM reflect a chronic care model, addressing system design, decision support, information systems and system organisation. The programme focuses on people with chronic conditions who have very high and complex needs. In addition to the CCM, the DHB has worked collaboratively with the community to develop ‘Let’s Beat Diabetes’, a whole-district initiative with considerable community participation. The CCM includes cultural competence as a core component. It is designed to meet the needs of Māori and Pacific peoples and to ensure equity in access and health outcomes for these populations district-wide. The theme of cultural competence is based on the model developed by the National Centre for Cultural Competence in the US. The CCM model requires providers to demonstrate a willingness and ability to understand the diverse cultures of their patients and work with key people from these cultures to develop targeted interventions, communications and support (Counties Manukau 2001; Wellingham et al 2003). Achieving culturally competent systems is recognised as a developmental process for organisations, involving ongoing education and training. Maori Innovation Fund Date: 27 Aug 09 Version: 2 Page 10 of 29 The CCM outlines plans for both Māori and Pacific peoples that acknowledge their culturally specific views of health and wellbeing. Each plan focuses on systematically incorporating cultural competency into every level of the organisation: organisational values, policy, recruitment and training, community involvement, development of language and resource materials, data collection, relationships with Māori and Pacific providers and ongoing quality improvement processes The Ngati and Healthy Prevent Diabetes Community Programme (Ngati Porou Hauora, Tairawhiti) The Ngati and Healthy Prevent Diabetes Community Programme in the East Coast is a joint health and education initiative between Ngati Porou Hauora (PHO) and the University of Otago. The programme aims to reduce the prevalence of insulin resistance (diabetes type 2) through the promotion of healthy lifestyles and increased awareness of diabetes in six Ngati Porou communities. A strong feature of the programme is a focus on the community as well as the individual. Activities such as hunting, playing touch rugby, fishing and gardening along with exercise programmes are promoted in the programme. Local runanga participate by hosting cooking demonstrations and community discussions on health and wellbeing. A mobile health service regularly travels to each community to monitor the health of those identified at high risk of diabetes. (Ministry of Health 2005b) An evaluation of this programme is currently being undertaken. A randomised survey of selected individuals preceding the programme found that type 2 diabetes mellitus is common among the population and that insulin resistance is even more prevalent, especially among younger age groups. Insulin resistance is believed to be an underlying cause of type 2 diabetes mellitus. (Tipene-Leach et al 2004) The Māori Case Management Clinic Project 2001-2003 (Raukura Hauora O Tainui, Clendon, Auckland) The aim of the project was to improve Māori health outcomes by establishing new primary care facilities that deliver a ‘by Māori for Māori’ model of community health care. New clinics were established in the high deprivation areas (NZDep deciles 8-10) of Manurewa/Clendon, Papakura and Mangere in order to provide accessible health care services. Operated by Māori health providers, the facilities aim to provide a low cost, high quality and culturally appropriate service for Māori living in these communities. Each of the clinics had to demonstrate that their model of health care incorporated tikanga (customary practice) consistent with the following Māori health paradigm: Tikanga Mo Nga Iwi Me Nga Hapu – appropriate engagement of Māori Tino Rangatiratanga – Māori control over health care Taha Whanau – involving the whanau in health care Taha Wairua – maintaining spiritual wellbeing Taha Hinengaro – maintaining emotional and mental wellbeing. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 11 of 29 Staff with appropriate background and experience were employed to meet the needs of the population. Since opening, the clinics have increased the number of staff in order to meet demand for services. A key focus of each of the clinics is providing case management under Care Plus for people with chronic diseases. Each of the clinics employs a chronic disease management nurse who works with patients in developing a care plan and provides support for self-management of their disease. The Clendon clinic opened on 1 February 2001, with a clinic opening in Papakura on 30 July 2001 and in Mangere on 8 October 2001. Results from the evaluation of the Clendon clinic showed that there was very rapid growth in registration in the initial stages, with around 50 percent of the total local Māori population registered. By November 2001 70 percent of patients registered were Māori, 12 percent were of Pacific descent. Seven percent of the enrolled population were identified with a chronic illness, with asthma and diabetes accounting for 64 percent of those with chronic conditions. The main factors given by people for accessing the Raukura O Tainui Clendon clinic were affordability, cultural acceptability and close proximity to patients. Meeting the needs of people in the community, institutional support from Tainui and the location of the clinic in a busy shopping mall were other factors attributed to the high enrolment. Low fees, seeing the whanau as a whole, generous consultation time, the full subsidisation of medication and the approach of staff all contributed to patients’ perceptions that the clinic was making an extra effort to meet their needs. Patients felt their information was secure and confidential and were assisted with accessing other support services. Patient satisfaction was reported as being very high. Kia Rite, Kia Ora Model (Whaiora Whanui Trust, Masterton) "Kia Rite, Kia Ora" has been designed to support Māori to realise their potential, build on whānau strengths and take control of their lives by building healthy relationships within primary care and community-based services. The programme focuses on improving the provision of care through: education, development of whānau wellness action plans, supporting and educating for selfmanagement of chronic conditions (like diabetes), improvements in co-ordinated care through primary and secondary health service. As part of the programme, a Social / Community Health Worker, Registered Nurse (Kaikōkiri) and a Doctor form the kāhui, to focus on the comprehensive wellness needs of the whānau tangata-whaiora. A pre-visit which takes place either in the home or at Whaiora – depending on the preference of the whānau tangata-whaiora. Medication review takes place and routine tests are organised according to standing orders and protocols. An agenda is created in preparation for the doctor visit with the whānau tangata-whaiora and to ensure that the doctor visit is fully informed. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 12 of 29 The pre-visit facilitates a comprehensive assessment and a successful doctor’s visit which allows sufficient time to build relationships between the tangata-whaiora and doctor and address all the agenda items in detail. Plans are developed with the whānau tangata-whaiora to improve self-management capability coupled with appropriate treatment regimes which are understood and agreed to by the tangata-whaiora. The Kaikōkiri is available to attend the doctor visit and maintains the relationship during the gap between doctor visits Post-visits are conducted by Kaikōkiri and ensure that the whānau tangata-whaiora understood what took place at the doctor visit. The main goal of the post-visit is to ensure that whānau tangata-whaiora are well informed and confident enough to manage actively the agreed plan. Between visits are conducted by Kaikōkiri to sustain and build on the progress made. These visits aim to find solutions to any difficulties being faced by the whānau tangatawhaiora in traversing their wellness journey. The model anticipates the need for advocacy to ensure they are well supported, for example in their interactions with other agencies (like Ministry of Social Development). The objective is to sustain self-management to a point where the whānau tangatawhaiora „graduates‟ from Kia Rite, Kia Ora into the Whaiora General Practice supported by current Whaiora services where they will be supported by appropriate SIA and Care Plus funding. Graduation is a formal assessment which evaluates the capability to selfmanagement the on-going wellness goals. The development of a low-cost access general practice at Whaiora later in 2010 will assist in supporting whānau tangata-whaiora who „graduate‟ from Kia Rite, Kia Ora and whose requirements of primary care will then require less intensive treatment. Kia Rite, Kia Ora is complementary to the Wairarapa DHB Clinical Services Action Plan 2009 and the Wairarapa Guided Care Model and it specifically recognises and addresses the social and environmental issues that impact our predominantly Māori client base. The programme is currently in development and will be evaluated in 2013. Get Checked The Get Checked (Annual Review) programme gives individuals with diagnosed diabetes an opportunity to consult with their GP and/or nurse each year and to plan their care for the year ahead. District Health Boards Get Checked services, are provided through contracts with Primary Care Organisations and General Practice. The programme was implemented in 2000 and entitles people with diagnosed diabetes to have a free annual health check from their GP or appropriately trained registered primary health nurse. The programme’s objectives are to: systematically screen for the risk factors and complications of diabetes to Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 13 of 29 promote early detection and intervention (in accordance with an evidence-based guideline) agree on an updated treatment plan for each person with diabetes prescribe treatment and refer people for specialist or other care if appropriate update the information in the diabetes register, which is used as a basis of clinical audit and for planning diabetes services in the area improve the planning and co-ordination of services delivered by all healthcare providers decrease the barriers to accessing high quality care for Māori and Pacific Island peoples. The Get Checked programme is part of one of the three National Health Targets to improve diabetes services. a. Increased percent of people with diabetes will attend free annual checks. b. Increased percent of people with diabetes will have satisfactory or better diabetes management. c. Increased percent of the eligible adult population will have had their CVD risk assessed in the last five years. Diabetes is important as a major and increasing cause of disability and premature death, and it is also a good indicator of the responsiveness of a health service for people in most need. The two indicators monitor the access quality improvement programs in primary care, and the quality of care and risk of diabetes complications. Cardiovascular disease (CVD) includes heart attacks and strokes - which are both substantially preventable with lifestyle advice and treatment for those at moderate or higher risk. The indicator monitors the proportion of the eligible population who have had the blood tests for CVD risk assessment (including the blood tests to screen for diabetes) in the preceding five year period. Green Prescriptions (GRx)/Te Rongoaa Kakariki The Hamilton Diabetes uptake of Physical Activity project (unpublished), led by a Margaret Williams, will provide a better understanding of ways to improve delivery of health services for Māori that will help reduce the disparities in health outcomes. The project involves patients managing their chronic disease through a Green Prescription (GRx)/Te Rongoaa Kakariki. The GRx initiative starts as written advice from a health professional to a patient to be physically active. Detailed advice and support are then provided by a physical activity advisor, often by telephone. The GRx is more effective in increasing physical activity in New Zealand European than Māori. Other modes of delivery of GRx to Māori need to be explored. One modified version using kanohi-ki-te-kanohi/face-to-face contact with the GRx advisor was trialed within the Te Wai o Rona: Diabetes Prevention Strategy. Interview analysis showed Māori participation increased because trust and rapport with the advisor were established. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 14 of 29 For this study of New Zealand European and Māori who are given GRx for six months it is hypothesized that those undertaking kanohi-ki-te-kanohi will have increased their physical activity more than those receiving telephone support at six months and one year follow-up. Both qualitative and quantitative measurements will be used to test the hypotheses and to explore differences by ethnicity and gender. One Heart Many Lives, PHARMAC One Heart Many Lives is a cardiovascular disease primary prevention programme, which targets Maori and Pacific Island men aged 35+. It aims to raise both awareness of heart disease and what causes it and decrease the level of cardiovascular risk among men aged over 35. The campaign aims to: increase awareness of cardiovascular risk and how that risk can be reduced encourage people at high risk of cardiovascular disease to see a medical professional (“get to your Doctor for a check up”) promote healthy lifestyle as part of managing overall care (“get more active”, “eat better” and “stop smoking”) The campaign involves social marketing focused on the way heart disease affects the person, their family and friends, their roles within their families/whānau, and their relationships and responsibilities. This part of the campaign tries to get men to personalise the risks of heart disease, thereby encouraging them to take action. The workshops are facilitated and include a broad cross-section of people. Highly inspirational people are brought in to speak to the groups. The workshops also include information on the optimal use of medicines (such as statins). A 2006 evaluation of One Heart Many Lives was favourable, describing it as “well developed” and “a useful contribution”. The Ministry also favours the campaign. We consider it to be one of the best opportunities to get nationally consistent messages out to communities. Moreover, the campaign uses the best available tools to provide those messages. Regional campaigns have been run in Porirua, the Hawke’s Bay, Gisborne, Northland and the Western Bay of Plenty. The initiatives were provided through local organisations, following a common One Heart Many Lives theme. The community-level approach has led to significant buy-in from communities and is responsible for much of the campaign’s success. Results from the regional campaigns indicate increased awareness about cardiovascular disease, an increase in the uptake of statins, and an increase in the number of people making changes to their lifestyle. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 15 of 29 SECTION THREE: DISCUSSIONS Purpose of this section This section provides points for discussion around improving the responsiveness to Māori. Summary The way the health care system is designed affects its ability to respond to the needs of those with chronic diseases and long-term conditions. Healthcare systems worldwide have evolved to support the management of acute and episodic care, but are less able to deal with people with chronic diseases and long-term conditions. In response to this mismatch, new models have been developed to describe the changes required in health care systems to improve the quality of care and outcomes for people and their families and whānau. Historically, medical care for people with chronic diseases or long-term conditions was provided by hospital based specialists. This is no longer possible or desirable and increasingly health systems around the world are recognising the pivotal role of primary health care for optimal management of chronic diseases and long-term conditions. Services, however, need to be supported by improved community/hospital integration and configured with new relationships across the health and social sectors. As well as shifts in the health system, the management of chronic diseases and longterm conditions requires an emphasis on the person and their family playing a central role in their own health care. The concept of supporting self-management focuses on people being partners in the process, contributing to decisions about their health care. This shift in focus is not just because people deserve to be partners in their own health care but also because the health care can then be delivered more effectively and efficiently. This emphasis on people and their families being partners in their care is framed within an understanding that the decisions and choices people make are influenced by a range of biological, psychological and social factors. Supportive environments are needed to encourage people in their health and wellbeing behaviours. This acknowledges the need to work across all of the sectors that impact on health, including social services, education, housing, and justice simultaneously. Māori with chronic conditions and their family/whānau have a vital role in managing the condition(s). Family/whānau meet a wide range of practical and emotional needs for people with chronic conditions. When involved in care planning, family/whānau may also support behaviour and lifestyle changes. It is easier for a person to achieve a comprehensive and clear management plan when the services they deal with have established relations with one another. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 16 of 29 For people and whānau to manage more effectively and safely at home, they need to develop knowledge and understanding of their condition. They need support to understand what they can do to keep themselves well, slow their condition’s progression, manage symptoms and when to seek help. This approach involves reorientating the health system to provide better and earlier support for people to live well with chronic diseases and long-term conditions. People with chronic conditions want continuity in their health care, regardless of how many professionals are required to assist them, or how many places they have to go to receive treatment and support. Having accessible services and knowing what each health professional contributes to their care plan helps a person to manage their condition better. This requires integrated systems and at times coordinated care. People can move backwards and forwards through different stages in their condition depending on the risk, severity and impacts of their condition at anyone time. This means that health care and other support needs will also vary in nature and intensity over time. The health care required across the chronic diseases and long-term conditions continuum ranges from prevention initiatives, self-management, early detection and intervention, management and treatment in community and hospital settings, rehabilitation to palliative care. Some of the key issues highlighted in section one are: Patient knowledge, attitudes, beliefs, values, and preferences are also associated with access to care Improving responsiveness and communication with Māori consumers and their Whānau Previous negative experiences with the healthcare system and/or perceptions of bias create barriers for Māori consumers to ultilize health services Recognition of socio-economic barriers, costs, patient attitudes, beliefs and preferences Recognition of the role of the essential role of Whānau Whānau, hapū, iwi and Māori community aspirations to have more control over their own health and wellbeing Some of the options explored to improve responsiveness to Māori include: Strengthening Whānau Knowledge of Health and Prevention Improving service responsiveness through coordinated care Supporting the role of the Whānau in Self Management Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 17 of 29 Case Management for Complex Care Strengthening and sharing successful Māori models of health Strengthening Whānau Knowledge of Health and Prevention Health literacy is a cornerstone of people being able to make informed choices and to take care of their own health. It enables people to make sound health decisions in everyday life. Improving health literacy underpins any activity to prevent and manage chronic diseases and long-term conditions. People with poor health literacy skills are at greater risk of experiencing poor health outcomes. People with poor health literacy are less likely to: recognise the first signs of medical problems, access health care services, communicate well with health professionals, understand health information and instructions, and sufficiently manage their long-term/chronic condition. People with poor health literacy skills also incur higher health care costs both for themselves and the system as they are: less likely to use prevention services and therefore enter the health system for treatment, less likely to have the skills to manage their medication which can have serious health implications and cause wastage, are more likely to use emergency services, and are more likely to visit and be admitted to hospital with preventable cases. Improving service responsiveness through coordinated care Co-ordinated Care means people have access to the right service, provided by the right person, in the right place at the right time. This is a style typically adopted by Māori Health Providers (see section 3, case studies). At the population level, co-ordinated care for chronic conditions management is about identifying risk, targeting interventions, and undertaking ongoing monitoring of long-term conditions within a particular population. Screening programmes are examples of proactive care as are services that facilitate the early detection of undiagnosed risk factors. Measures, such as risk stratification, can be used to inform planning for different levels of care for local populations. It means broadening the range of care that is offered in through primary health care by going to where people are. For example taking services to schools, workplaces, community centres and homes, and working in partnership with organisations and individuals in the community. It also means targeting specific populations at risk of or with long-term conditions as well as looking systematically about how health care funding and practices can be improved to ensure proactive long-term conditions management. Co-ordinated care means everyone works in a joined up way regardless of discipline, sector, or funding source. It is continuous and connected care consistent with peoples’ needs and life context and enables people to be cared for closer to home. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 18 of 29 This joined-up working is especially important for people with long-term conditions as their needs cut across multiple providers as their condition progresses. Too often there is fragmentation and a lack of communication, as services and attitudes are not fully aligned to the co-ordinated care concept. Successful programmes designed by Ngati Porou Hauora and Raukura Hauora o Tanui included the following approaches to improving service responsiveness: service providers speaking the same language as patients; providing transport; providing multiple services on the same site; proximity of clinics to patients’ homes; having a holistic person-centred approach that addresses the diverse needs of patients and their family/whānau/community; delivering a service by Māori for Māori; the attitudes and behaviour of staff; the cost of health care services; flexible consultation time; subsidisation of medication; and partnership with iwi. Supporting the role of the Whānau in Self Management Supporting self-management is an evidence-based approach that has the potential to not only improve health outcomes, resource utilisation, treatment adherence, but also quality of life and general well-being. Self-management helps moves people from passive recipients of health services to becoming active and informed partners. Supported self-management requires a planned approach. This is the simple question of who will do what, when and how. Mechanisms are needed to ensure routine prevention, screening and sustained follow-up. The roles and responsibilities within multi-disciplinary teams need to be resolved including how workloads are divided. There are also consequences for how a practice is set up and run. Implementing self-management requires a shift in the health system culture. Such an approach will fundamentally change how health care is provided and will only be effective if entire teams embed self-management into usual practice. Self-management changes the nature of relationships with a focus on behaviour change rather than solely clinical recommendations and treatment. Primary health care providers, in particular GP’s, have a pivotal role in ensuring people can access the support they need for self-managing. This means working together with whānau and family, pharmacists, community health workers, specialists, hospitals, social services and community and voluntary organisations. Referrals and recommendations from GPs and nurses can also have a significant influence on people attending a selfmanagement programme. Work to improve supported self-management must also focus on supporting and building the evolving capacity and skills of Māori providers, as key players in the prevention and management of chronic care management and long-term conditions. These providers need to be working in an integrated way with mainstream health providers so that their patients receive proactive and co-ordinated care. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 19 of 29 Improving complex care (Case Management) People with more complex conditions need more intensive case management and coordination of care. They are vulnerable to rapid deterioration of their condition, putting them at high risk of unplanned hospital admissions. Evidence has shown that intensive, on-going and personalised case management can improve the quality of life and outcomes for these people, dramatically reducing hospital admissions and enabling more rapid return to home. Case management is particularly important during end of life stage. The addition of appropriate palliative care to case management greatly enhances the quality of care for patients with long-term conditions particularly in the last 12 months of life. This approach involves integrated and seamless care across the continuum, regardless of whether the setting is in the home, in primary health care, hospice or hospital maintaining patient autonomy and choice. These high-risk patients need not only good management of their specific disease, but a holistic overview of their full health and social care needs. Key to meeting these needs is a case manager or lead worker. General practice teams, in particular, have a core role to play in case management. However, depending on a person’s needs, this case manager role may transfer to other members of the inter/multidisciplinary team. Case management is particularly important for integrating care between primary and secondary services and rehabilitation. It involves people having the right level of care when they need it. Strengthening and sharing successful Māori models of health Māori health providers are a key feature of this sector. Growing from a figure of 20 providers in the early 1990s, there are now approximately 250 providers located throughout the country. Māori health providers are typically small, relatively new organisations with a strong not-for-profit philosophy. What differentiate Māori health providers from other mainstream providers are the underlying cultural values and principles, or kaupapa, guiding their operation and development. Many see their work as an extension of their community with personnel directly drawn from within the community they serve. Many are also linked with providing a broader range of non-health services like family violence initiatives, alternative education programmes, budgetary advice, youth related initiatives and so on. A number of these providers have worked with District Health Boards, Primary Health Organisation, Tertiary Institutes or Māori communities to design a range of health programmes that respond to chronic conditions. Three of these programmes are highlighted in the next section. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 20 of 29 APPENDIX ONE: MINISTRY DIRECTION Purpose of this section This section provides an overview of the role of the Ministry of Health. Ministry of Health The Ministry of Health is the Government’s primary agent in the health and disability system. The Ministry has overall responsibility for the management and development of that system. It also acts as the Minister’s principal advisor on health policy, and is a funder and regulator of health and disability services. The Ministry provides an important leadership role across the system and is the primary means of driving performance improvements within the system. The Ministry also plays an important advisory role to the Government in supporting effective decision-making. Health policy is complex and challenging, with a multitude of difficult and potentially contradictory policy choices. There is considerable public pressure on governments to expand public spending on new medical technologies and greater levels of care and interventions. However, the Government has only limited funding and must make the best choices possible. Complicating decision-making is the increasingly sophisticated nature of treatments and choices, as well as shifting expectations about what constitutes acceptable levels of ailments and limitations on ‘good health’. The increasingly complicated nature of health and disability technology and policy choices, means there is a need to keep patients and local communities involved in decision-making, as well as balancing the management of the system while supporting clinically led decision-making. As well as its key advisory role to the Government and the health and disability system, the Ministry also aspires to be a trusted and respected source of reliable and useful information about health and disability matters in New Zealand for all New Zealanders and the wider international community. The Ministry’s core functions are to: improve, promote and protect the health of New Zealanders advise the Minister on strategy, policy and system performance, including advice on improving health outcomes, reducing disparities, ensuring fairness and increasing participation; nationwide planning, co-ordination and collaboration across the sector; and the implementation of the four key strategies currently in place (Health, Disability, Māori Health and Primary Health Care) Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 21 of 29 act on behalf of the Minister to monitor and improve the performance of health sector Crown agencies and District Health Boards, which are responsible for the health of their local communities administer legislation and regulations on behalf of the Crown, and meet legislative requirements fund and purchase health support services on behalf of the Crown, including the maintenance of service agreements, particularly for public health, disability support services and other services funded by the Ministry service Ministers’ offices and ministerial advisory committees. The Ministry also has health professional and advisory roles to provide clinical and technical advice to the Minister, and within the Ministry and the sector. Some of these functions also have clinical decision-making and/or statutory responsibilities (such as the Director of Public Health). Strategic Direction for Māori Health He Korowai Oranga: Māori Health Strategy sets the direction for Māori health development in the health and disability sector. The strategy provides a framework for the public sector to take responsibility for the part it plays in supporting the health status of whānau. The overall aim of He Korowai Oranga is whānau ora - Māori families supported to achieve their maximum health and wellbeing. He Korowai Oranga recognises that both Māori and the Government have aspirations for Māori health and critical roles in achieving the desired whānau outcomes. He Korowai Oranga also recognises that there must be partnership between Māori and health and disability organisations if those aspirations are to be realised. The two broad directions of He Korowai Oranga acknowledge this partnership. He Korowai Oranga acknowledges the contributions that Māori have made in leading health sector change, and a major focus of the strategy will be to strengthen opportunities for whānau, hapū, iwi and Māori communities to contribute in the future. He Korowai Oranga supports whānau, hapū, iwi and Māori community aspirations to have more control over their own health and wellbeing. It upholds the structures based around whānau, hapū and iwi. It also recognises that there are a range of other community groups in Māori society that make valuable contributions to the advancement of whānau ora. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 22 of 29 Figure 1:Overarching framework of He Korowai Oranga: The Māori Health Strategy Whānau ora Overall aim Māori aspirations and contributions Broad directions Key threads Pathways Rangatiratanga Whānau, hapū, iwi development Māori participation Crown aspirations and contributions Building on the gains Reducing inequalities Effective service delivery Working across sectors Source: Ministry of Health (2002). He Korowai Oranga outlines four pathways central to realising whānau ora. Whānau, hapū, iwi ,and community development Māori participation in the health and disability sector (eg, supporting effective Māori health providers and a highly skilled Māori workforce). Effective health and disability services. Working across sectors to address the broader determinants of health (such as social development, education, and housing). Six actions consistent with the four pathways central to realising whānau ora are as follows. Ensuring programmes and services are culturally appropriate; located within a Māori worldview; and in the context of communities, whānau, hapū, and iwibased structures and settings that sustain them; delivered by Māori delivery systems (eg, Māori community-led or a Māori service provider); and supported by the development and strengthening of the Māori health workforce. Ensuring Māori whānau and communities receive the right information and tools in a culturally appropriate mode to make informed choices. Supporting and resourcing Māori-led research to inform Māori communities and the Government about interventions that work for Māori communities. For example, interventions to prevent obesity, interventions to treat and manage obesity, interventions based on Māori models of healthcare paradigms and methodologies, and methods to improve service delivery to urban and rural Māori populations. Developing Māori services. Māori providers play a pivotal role in improving access to and the effectiveness and appropriateness of health and disability services. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 23 of 29 Improving mainstream services to make sure they are effective for Māori. Improvements will emphasise cultural competence in the health sector and recognise the need to proactively guide whānau to and through health care services to better realise their desired health outcomes. The Government’s Health Targets The Government’s Health Targets are a set of national performance measures specifically designed to improve the performance of health services. The targets provide a focus for action. They also provide a way of measuring whether or not the health and disability system is making a difference in improving health for all New Zealanders. The Ministry and the Minister review the Health Targets annually to ensure they align with Government health priorities. The Government has identified two major areas for focusing action: improving hospital productivity and speeding up the implementation of the Primary Health Care Strategy. Under these two broad headings are six targets to improve the health sector’s performance and ensure our health and disability system is contributing to maintaining and improving health outcomes in these important areas. Table 1: Health Targets and how they are measured Health Target Measures Improving hospital productivity Shorter stays in emergency departments 95% of patients will be admitted, discharged or transferred from an emergency department within 6 hours. Improved access to elective surgery The volume of elective surgery will be increased by an average 4000 discharges per year (compared with the previous average increase of 1400 per year). Shorter waits for cancer treatment Everyone needing radiation treatment will have this within 4 weeks by December 2010. Primary Health Care Strategy Increased immunisation 90% of 2-year-olds will be fully immunised by July 2011, and 95% by July 2012. Better help for smokers to quit 90% of hospitalised smokers will be provided with advice and help to quit by July 2011, and 95% by July 2012. 80% of patients attending primary care will be provided with advice and help to quit by July 2011, and 90% by July 2012. Better diabetes and cardiovascular services An increased percentage of the eligible adult population will have had their cardiovascular disease risk assessed in the last 5 years. An increased percentage of people with diabetes will attend free annual checks. An increased percentage of people with diabetes will have satisfactory or better diabetes management. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 24 of 29 The Ministry of Health and the District Health Boards are collectively responsible for the Health Targets. Each District Health Board has its own local targets, which take into account the particular health needs of its community. Collectively these targets contribute to a national improvement in each area. The Ministry of Health has appointed ‘target champions’, who work with and provide support to the health sector. The Ministry reports on District Health Board achievement against these targets throughout the year. The Diabetes and Cardiovascular Disease Quality Improvement Plan (QIP) The Diabetes and Cardiovascular Disease Quality Improvement Plan (QIP) is a clinically-led action plan that identifies priorities and recommends actions for continuous improvement of diabetes and cardiovascular (CVD) services. A sector steering group oversees implementation of the Plan and identifies priorities to be progressed each year. The QIP work programme contains a number of initiatives that are designed to make a difference to people with diabetes and their families/whanau. There is a particular emphasis on reducing the inequalities experienced by Maori in terms of access to services and health outcomes. The initiatives in the work programme include: producing tools and advice to health professionals to provide effective advice to individuals and whanau, based on updated diabetes guidelines establishing demonstration pilots testing interventions to reduce the impact of kidney disease resulting from diabetes improving retinal screening and diabetic foot care to reduce the impact of blindness and amputation improving responsiveness to Māori with chronic conditions through primary care diabetes and cardiovascular disease pilots. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 25 of 29 APPENDIX 2: IDENTIFIED KEY GROUPS Te Hotu Manawa Māori An independent national organisation delivering health services “by Māori for Māori” that are tailored to the needs of Māori to improve heart health (Te Hotu Manawa Māori, 1997). Their mission statement is ‘to provide leadership, support, education and advocacy to empower Māori communities to improved health through good nutrition and participation in regular physical activity’. The organisation offers training for improving Māori nutrition and physical activity, health education resources, networking opportunities and an advisory and advocacy role (Te Hotu Manawa Māori, 1997). Māori PHO Coalition The Māori PHO Coalition is a national coalition of 11 Māori led PHOs, which represent urban, rural and tribal entities that support a growing constituency (Simon Royal, 2009). The Māori PHO Coalition supports a range of primary care services, including whānau ora development, for over 200,000 predominantly high need clients. Whānau Ora development is supported through: facilitating effective service development & contracting for outcomes based service models collaborate regionally with other providers to ensure access. providers to ensure access providing management services to support corporate functions and manage delegated funding (Simon Royal, 2009). Te Roopu Mate Huka Te Roopu Mate Huka O Aotearoa (Māori diabetes collective of New Zealand) is a national consumer group working and advocating on behalf of whānau, hapu and iwi with diabetes (Te Roopu Mate Huka, 2006). The collective ensures that all diabetes related procedures at a national level guarantee Māori equitable access to culturally effective and specific health and disability services of the highest quality in accordance with the principle "by Māori, to Māori, for Māori" The five goals of Te Roopu Mate Huka are: 1. develop a suitable kaupapa maori diabetes training program for consumers, diabetes educators and other stakeholders group 2. to monitor diabetes service delivery for Māori 3. develop and strengthen key relationships and effectively process and distribute new resources with all alliances with Te Roopu Mate Huka 4. to promote Te Roopu Mate Huka to iwi and the wider community 5. to uphold the mana of TRMH (Te Roopu Mate Huka, 2006). Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 26 of 29 Te Ohu Rata o Aotearoa (Te ORA): Māori Medical Practitioners Association of Aotearoa/New Zealand An organisation providing Māori medical leadership that represents Māori medical professionals (medical students, doctors, clinicians, researchers and teachers) (Te ORA, 2009). The aims of Te ORA are to: promote and protect the health of Māori people assist Māori medical practitioners in their efforts to advance Māori health facilitate closer links between Māori medical practitioners and other national, professional and community groups. Te ORA currently has 250 Māori medical student and doctors registered with them. Members are provided with opportunities to network and share information, as well as attend regional huis and the annual Te ORA conference (Te ORA, 2009). Hauora.com (National Māori Health Workforce Development Organisation) Hauora.com is a national Māori-led organisation that provides a central point of contact for Māori health professionals, workers and managers. Services include Māori workforce planning, resources, information, health research, career options, advocacy policy analysis and advice (National Māori Health Workforce Development Organisation). The mission of Hauora.com is to ‘grow an effective Māori workforce, so that Māori comprise at least 15% of the total health workforce in Aotearoa/New Zealand’ (National Māori Health Workforce Development Organisation) Tumu Whakare (National Reference Group of Māori Health Strategy Managers within DHBs) Tumu Whakarae provides DHBs with Māori leadership and advocacy (it does not represent Māori). Each DHB is required to have at least one representative on the group. The aims of the group are to: Share information and advocate for Māori health and reducing disparity that will contribute to the achievement of whānau ora Be an agent for changes required for the achievement of whanau ora Lead projects that are related and relevant to whānau ora. Best Practice Advocacy Centre (BPac) Is an independent organisation that promotes healthcare interventions which meet patients needs and are evidence based, cost effective and suitable for the New Zealand context (BPac, 2009). Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 27 of 29 BPac published its first Māori Health edition journal (BPJ 13 – Improving Māori Health) in May 2008. The journal has focused on the following topics, all of which remain priorities for Māori health: cardiovascular disease diabetes asthma and chronic cough rheumatic fever gout. The first journal included a framework ‘practical solutions for improving Māori health’ and talked about disparities across Māori health and how providers can address these. 1 Plan to improve Māori health Change does not happen by accident, it needs a plan. Develop a simple practice plan for addressing disparities. Ask your PHO for a copy of its Māori health strategy. 2 Set realistic practice goals You don’t have to change everything at once. Set priorities. The first goal may be as simple as correctly recording ethnicity or smoking status. 3 Build trusting therapeutic relationships Invest time in building trusting therapeutic relationships with patients and whānau. 4 Engage patients in their health issues Consider each contact as an opportunity to educate and engage patients in their health care and address wider issues. 5 Agree on realistic patient-centred health goals Break up the health issue into manageable pieces. Agree on achievable treatment goals, activity goals and lifestyle changes. 6 Make it easy for patients to come back Give patients a reason and expectation about returning. Use reminders. Make the environment welcoming. Offer solutions for financial barriers. 7 Form partnerships Find out who is taking responsibility for a patient’s healthcare – it may be another whānau member. Involve Māori health providers. Encourage community initiatives. Table 1: “The health system can become a leading solution in the ‘crisis in Māori health’ that is evident in current disparities” (BPac, 2009). Bpac believe successful services targeting Māori can be achieved with careful planning and effective targeting of services and profiled three initiatives: One Heart Many Lives – cardiovascular risk assessment for Māori men in Hawke’s Bay rural general practitioner clinics in central Otago Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 28 of 29 mobile practice nurse services in Hamilton. They found that while there are many successful services targeting Māori around the country, more can and should be done to ensure the momentum continues and improvements to Māori health are prioritised. Whānau ora – families supported to achieve their maximum health and wellbeing – remains an important aim. Discussion Paper: Māori and Chronic Conditions Date: 28 April 10 Version: 1 Page 29 of 29