Go here for NBRC hints
advertisement

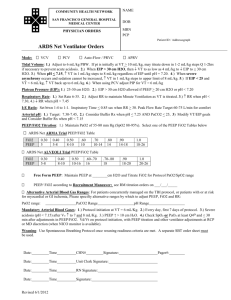
Billy Bob's Protocol Guide to the NBRC Hospital
Revised: Oct. 13, 2008
Adult CMV Rules
Intubate and Ventilate if:
PaCO2 with pH < 7.30 (Hypercarbia with Respiratory Acidemia)
Initial Ventilator Settings; use (adult)
A/C or SIMV (add PS +512 cwp to WOB through ETT)
f = 812 breaths per min.
Vt = 1012 ml/Kg (or 89 ml/Kg if 1012 not a choice)
Use only 10 ml/Kg Vt for child
For exacerbation of Severe COPD try1st: V/M @ 28% or 2 L/m N/C if V/M not an option; but avoid N/C b/c
delivery is estm.
2nd: BiPAP - if pH is < 7.30 (see: N COPD ABG)
where IPAP adjusts ventilation (1015 cwp)~ Vt with pH
and EPAP adjusts oxygenation (4 cwp) ~ PaO2
3rd: CMV with smaller Vt & FIO2 initial parameters or
If fails, switch to SIMV with PS
f = 812 breaths per min.
Vt = 6 10 ml/Kg (b/c hypercompliant)(also adjust with IPAP)
FIO2 = 30% 40%
PEEP = 2 5 cwp will help prevent air-trapping causing
intrinsic PEEP or auto-PEEP
For ARDS with PIP; can use Permissive Hypercapnea with
Vt = 57 ml/Kg allowing PaCO2 & keep pH > 7.25 (see below)
Initiate Pressure Control Ventilation (PCV) when Pplat > 3540 cwp or PIP > 50 cwp
b/c of chemical mediator release lung damage (ALI= acute lung injury)
Initial PCV settings;
PIPPCV estm. = at 50% of PIPA/C (on A/C) or = Pplat, then
target Vt by adj. PIPPCV where 5 7 ml/Kg IBW
(See Permissive Hypercapnea above) and add
PEEPPCV = 50% of PEEPA/C
FIO2 = 100% or 1.0
I:E = 1:2 or inverse ratio with pt. sedation; caution
2:1 ratios or > b/c Auto- PEEP can occur
Monitor Vt Exh. b/c PIP limit determines Vt: CL or Raw changes affect Vt Exh
PCV also indicated in pleural air leak where
set PIPPCV = PPlateau adjusting f to control PaCO2
For NMD with fatigued muscles and stable Cst - use Bilevel ventilation
Ventilation - Always treat FIRST; a combination of PaCO2 and pH; ventilation when
respiratory acidosis < 7.30 pH; remember respiratory alkalosis is not a ventilation problem
Exceptions:
Severe COPD:- try BiPAP 1st b/c hard to wean from CMV
initiate IPAP~15 cwp with an EPAP~ 4 cwp (See: COPD normal ABG's)
NMD:- Respiratory Insufficiency (i.e.: RR >35 b/min., HR>100 b/min.
& even though N acid/base balance = intubate & CMV b/c impending AVF
Cerebral Trauma:- (i.e.: MVA, Sub-Arachnoid Hemorrhage) keep
PaCO2 = 25-30 Torr so pH is alkalotic to ICP (via vessel constriction) &
keep PaO2 ~ 100 Torr (i.e.: FIO2 as needed)
Oxygenation – Always treat 2nd; after evaluating ABG for
Respiratory Alkalosis (Acute or Uncompensated) with Mod. Hypoxemia
FIO2 to 60% max., then start CPAP b/c refractory hypoxemia
Wean from FIO2 and CPAP (or PEEP) by FIO2 1st till reach 60 %, then
PEEP until = 5 cwp, and then FIO2 again in 10% increments to ~ 40-30%
b/c O2 toxicity is 1st concern and barotraumas is 2nd
Can MV if FIO2 and PEEP is not an option (i.e.: f, Vt, add PS) to PaO2
Tissue Hypoxia exists if PvO2 < 30 Torr & or SvO2 < 56 %
DC all O2 therapy if PaO2 = > 5 X FIO2 %
Supplemental O2 Adult ~ should be in range of 30% to 60% FIO2
NRB (100%) ~ indicated ONLY in emergency or trauma conditions
CMV - Weaning Parameters: weanable ifVC 1015 ml/kg IBW; measures for effective cough (monitor daily)
MIP ≤ -20 cwp; measures strength for effective cough (monitor daily); N= -50100cwp
Vt spont 3 ml/lb. or 6.6 ml/Kg of IBW indicates "continue weaning"
RSBI = RRspont./Vt spont.(L) ; # < 100 = weanable; # > 100 = needs CMV
(A-a)G on 100% < 350 Torr before weaning attempted; where N = 60100 Torr; b/c
>350 Torr V/Q mismatch or diffusion deficit [i.e.: (A-a)G should be ]
VD/Vt < 0.60 = pt ready to wean; where 25%35% (i.e.:0.25 0.35)= N
Where:
VD/Vt = PaCO2 - PECO2
and therefore
PaCO2
VD = PaCO2 - PECO2 X Vt
PaCO2
PEP > 40 cwp = weanable b/c effective cough (also: MEP, MEF)
Always choose MIP, VC, RRspon, Vt spon., when considering weaning, even if on A/C= 12
ETT Sizes - Adults:
Teenager (16 YO)
Female (average size)
Male
Large Adult
= 7.0 mm;
= 7.5 – 8.0 mm;
= 8.0 – 8.5 mm
= 9.0 – 10.0 mm
CMV - Weaning Strategy
Switch from A/C to SIMV where
f =10, 8, 6, 4 or 2 flow-by; after ABG results reveal respiratory alkalosis
without hypoxemia;
always adjust f (not Vt) to change Valveolar with SIMV or Control modes and
always adjust Vt (not f) to change Valveolar in A/C mode
consider PS of 512 cwp to WOB through ETT (or 510 cwp)
FIO2 to 60 %, then PEEP/CPAP to 5 cwp, then FIO2 until 4030 %
Make changes b/c of :
ABG results reveal respiratory alkalosis without hypoxemia
or b/c pt. is resting comfortably with good spontaneous ventilation
measurements
or b/c MIP & VC (done daily) are acceptable
Note: Small ventilator changes are better than big changes
Remember: Adjust f to alter PaCO2 in SIMV or Control modes AND
Adjust Vt to alter PaCO2 in A/C (where VE is best changed)
Auto-PEEP (intrinsic PEEP) - Monitor expiratory flow curves returning to zero;
causes risks of barotrauma & CO
ABG for Severe COPD; Normal values
PaO2 = 50 65 Torr
PaCO2 = 50 60 Torr or
pH
= 7.30 7.35
HCO3- 32 mEq/L
Note - COPD chemoreceptors not depressed until PaO2 ~ >70 Torr
IBW Calculation (NBRC)
female = 105 lb for 60" plus 5 lb/in. over 60"
male = 106 lb for 60" plus 6 lb/in. over 60"
Estimate VE, PaCO2, Vt or f, where:
f(Desired) X PaCO2 (Desired) = f(Actual) X PaCO2 (Actual)
and therefore the following can be formulated:
fdesired = (f current) (PaCO2 current)/ PaCO2 desired ; where (↑)(↓) = (↓)(↑) or (↓)(↑)=(↑)(↓)
.
.
VE desired = (VE current)(PaCO2 current) , Also
PaCO2 desired
Vt desired = (VE current)(PaCO2 current)
PaCO2 desired
Neonatal Rules
(3,000 g or 3 Kg is normal birth wt. ~ 6.6 lbs.; anything less is probably a premie)
Initial Ventilator Settings for babies; Switch baby to PCV from CPAP after:
CPAP = 8 10 on 80% with PaO2 < 50 Torr and PaCO2 > 60 Torr (see neonate N ABG below)
Pressure Control for neonates with
f = 40 breaths per min.(or in range 3050 b/min.)
where normal RR = 4060 b/m
PIP = 25 cwp (or in range 1525 cwp)
FIO2 = 0.60 (b/c baby was on CPAP at 0.60)
PEEP = 2 4 cwp (only after initial therapeutic setting of 45cwp)
*Note - when PEEP, Vt will b/c of PC mode (i.e.: Vt=PIP-PEEP)
HFV = 3 types
1) HFPPV: where f = 60100/min., Vt = 35 ml/Kg, I:E = 1:3 or <
2) HFJV: where f = 100600/min., PIP ~ 810 cwp, I:E = 1:11:4
Alarms: PLow
3) HFO: where f = 603,600/min., Vt < VD anatomic
Also:
ECMO is indicated for those infants not responding to PC ventilation
Surfactant replacement is indicated for infants with RDS to open
up atelectatic alveoli; given within 1224 hours of 1st symptoms
Ventilator Changes for Neonates
Ventilation - Always treat first; a combination of PaCO2 and pH
Oxygenation – Always treat 2nd a combination of FIO2 and PEEP
PEEP by only 24 cwp at a time
Caution with PPHN (Persistent Pul. Hypertension Neonate) b/c compressed
alveolar capillaries patent ductus arteriosis & or Foramen Ovale
FIO2 = 0.10 max. at a time, unless option exists to:
Titrate FIO2 to maintain SpO2 93%
Extubate when CPAP is @ 2 cwp (b/c normal FRC is maintained with CPAP = 2 cwp)
Apgar Scores: 5 parameters @ 0, 1 & 2 pts with 10 pts max.
710 = N = observe, sx upper awy w bulb syr., place in warmer
4 6 = moderate asphyxia = BVM stimulate & place on O2
0 3 = severe asphyxia = immediate resuscitation, ventilation with FIO2
ABG for Neonates:
PaO2 = 50 70 mmHg
(Sills PaO2 neonate = 60 – 70 Torr)
PaCO2 = 35 45 mmHg
pH
= (7.25) 7.35 7.45
HCO3- = 2026
where, ROP (retinopathy of prematurity) ~ PaO2 > 80 Torr
also, Umbilical ABG = Radial ABG
Capillary Gases for Neonates:
PcO2 = 4050 Torr
PcCO2 = 4050 Torr
N Vital Signs for Neonates:
HR = 130-150 b/min., BP = 75/45 (9060/6030); RR = 4060 b/min.
acrocyanosis (peripheral cyanosis) is N after birth;
however, central cyanosis is NOT Normal and O2 trx must be initiated
Serum Glucose Levels should be measured in INFANTS
CBC should be assessed for O2 carrying capacity of the blood & infection
Ductus Arteriosus – detected via two PTCO2 electrodes i) R upper chest (preductal) &
ii) L chest, abdn, or thigh (post ductal)
CPAP for Neonates:
Start CPAP ONLY when pt demonstrates hypoxemia on 60 % FIO2 (indicates atelectasis)
Remove ETT when CPAP = 2 cwp b/c < will ↓ FRC below N
CPAPmax. Neonates = 12 cwp (Sills p. 402)
ETT Sizes (neonates): 3,000 g or 3.0 Kg is normal birth wt.; anything less is probably a premie)
Pre-Term 2.5 Kg
= 2.5 mm;
Full Term (3840 wks gestational) = 3.0 mm;
1 year old
= 4.0 mm
CSE- DO NOT ORDER ON INFANTS - PEFR, MIP, VC as inappropriate
EKG
Recommend 12-lead ECG = to dx. signs/symptoms of acute serious cardiac arrhythmia
Atrial Fibrillation = Cardioversion is indicated; energy level = 25100 joules
Ventricular Fibrillation (also: Pulseless Ventricular Tachycardia) = Defibrillation is indicated;
200 J initially, then energy to 360 Joules if 2nd or 3rd is not successful.
All other cardiac arrhythmias are trxed w medication
Medication vs. Cardiac conditions:
Lidocaine - trx. Ventricular Fibrillation, Ventricular Tachycardia & PVCs
Epinephrine - trx. Ventricular Fibrillation, Sinus Arrest & Asystole
Atropine - trx. Sinus Bradycardia & Asystole
HR measured via EKG grid lines as: 300 (60/0.2), 150, 100, 75, 60, 50 (6th box or 60/1.2)
Equipment Rules
Flow Conversion to L/sec:
60 L/min = 1.0 L/sec
50 L/min = 0.83 L/sec
45 L/min = 0.75 L/sec
40 L/min = 0.67 L/sec
30 L/min = 0.50 L/sec
5 L/min = 0.0833 L/s; i.e.: 20 L/m = 4(0.08333) = 0.33 L/s
Air:Oxygen Ratios: 60% = 1:1
50% = 5:3
45% = 2:1
40% = 3:1
35% = 5:1
30% = 8:1
28%= 10:1
26%= 15:1
24% = 25:1
Heliox:
ONLY delivered via NRM
80/20 mixture = 1.8 X O2 flow = actual flowHeliox
shortcuts = multiply O2 flowmeter rate by 2 & round to estm. He/O2 flow
= divide He/O2 Rx by 2 & round for O2 flowmeter flow to use
70/30 mixture = 1.6 X O2 flow = actual flowHeliox
shortcuts = multiply O2 flowmeter by 1.5 & round estm. He/O2 flow
= divide He/O2 Rx by 1.5 & rd for O2 flowmeter flow to use
70/30 is lowest He concentration delivered b/c O2 is heavy
LOX:
1 lb LOX = 344 L gaseous O2
1 L LOX = 2.5 lb LOX = 860 L gaseous O2
Cylinder to Empty
Textbook calculation
# min = (# psig)X[(0.28~E; 3.14~H )]
# L/min
# min = # hours
60 min/hr.
Billy Bob's Shortcut:
* for E cylinder ~ substitute 0.28 to 0.3
* drop one zero from the # psig and multiply by 3
* divide by # L/m, which ~ # min
* drop the last digit and divide by 6, ~ # hours
* choose the # min or hours that is slightly lower than calculated
* for H cylinder: substitute 3 for 3.14 and round up
Capnography - N exhaled air contains CO2 = 4.55.5% or 3545 Torr
If ETT is in the esophagus, then this value will be near zero % (i.e.: 0.5%)
Note: PaCO2 > PETCO2 and
P(a-ET)CO2 + PETCO2 estimates PaCO2 also
P(a-ET)CO2 = 15 Torr
P(a-ET)CO2> N or is indicates Pulmonary Emboli, LHF or COPD
Also: exhaling to END Max Exhalation can differentiate PE above: i.e.
P(a-RV)CO2> N = PE where P(a-RV)CO2= N indicates LHF or COPD
Transcutaneous O2 Analyzers – PTCCO2 zeroed on RA: think Perfusion & Diffusion
IS - min VC => 10 ml/kg otherwise chg to IPPB
UAC ~ distal tip @ T6 T10; b/c lower causes cyanosis of lower extremities
CPT with head ~ if not tolerated add 10% FIO2 or change to PEP Device
NO (nitric oxide) is adm @ 10 ppm initially & to 20 ppm, where PVR>240 dynes.sec.cm-5
Reminder: PVR = N = 1.5 3.0 Torr or 80 - 240 dynes∙sec∙cm-5
SPAG - set the nebulizer as high as it will go, then add enough drying flow to =
15 L/min total; also, drying chamber should have < 10 L/min. or no aerosol
Oropharyngeal Awy - used ONLY for unconscious pt. to maintain patent upper airway.
Combitube (ETC: Esophageal Tracheal Combitube) - an emergency awy device
inserted with minimal skill; not used with pediatric nor short adult pt.s;
use a colorimeter or capnography to determine where the tube is placed
Chest Tubes:
placed in 2nd 4th anterior intercostal space to evacuate air
placed in 6th 8th intercostal space to evacuate fluid
vacuum set at -20 cwp for Pleur-Evac System, or at
-15 cwp for direct line suction (b/c of < sx control)
Galvanic Fuel Cell – “recalibrate” before replacing fuel cell, if FIO2 measurement a problem
LMA – Laryngeal Mask Airway:
- inserted by minimally skill or perhaps an anesthesiologist during surgery (vs. ETT)
- lubricate posterior mask; insert with the index finger over epiglottis f/b
mask inflated 60 cwp
- can NOT be used on conscious nor semiconscious pts (b/c of gag reflex)
(must be unconscious)
- gastric distention = bagging or CMV where PIP > 20 cwp b/c LMA will leak
- aspiration can still occur
Pulse Oximeters –
think Perfusion & shine a Light through the blood
Hemodynamics
CVP = N = 6 1 Torr; reflects RH pressure (also reflects RV preload)
PAP = N = 25/10 Torr (3020 Torr/155 Torr), reflects RH pressure
PAP when PVR or PCWP; then CVP also
also PAP b/c of PaCO2, pH, or PaO2, hypervolemia (start Lasix)
PAP b/c hypovolemia (add fluids), pul. vasodilation, or PaO2
PCWP; N = 124 Torr; measures L Atrial press. & LV end-diastolic press.; where
PCWP = left heart abn.s (i.e.: CHF, Mitral & Aortic Valve Stenosis)
PCWP > 18 Torr b/c of "Cardiogenic PE" from CHF (LHF)
Also, increased b/c aortic stenosis, mitral valve regurgitation)
PCWP < 4 Torr = hypovolemia;
NOTE: PE with N PCWP indicates "Noncardiogenic PE" (i.e.: ARDS);
Balloon tip inflation hold for < 1520 sec. to prevent infarction
PVR = N = 1.5 3.0 Torr or 80 - 240 dynes∙sec∙cm-5
if PVR = pulmonary hypertension (b/c of acidemia, hypercapnia, hypoxia, then PAP)
then CVP & PAP are also
SVR (Systemic Vascular Resistance) = N = 900 - 1400 dynes∙sec∙cm-5;
SVR < 900 ~ hypovolemia;
SVR > 1400 ~ hypervolemia
Tissue Hypoxia = SvO2 < 56% & or = P vO2 < 30 Torr: where N. P vO2 = 40 Torr (3743)
CI =Cardiac Index =QT/BSA N QT = 2.54.0 L/min/sm2of body surface area
= a reflection of QT (cardiac output)
CI < 2.5 ~ hypovolemia;
CI > 4.0 ~ hypervolemia
QT =
VO2 __________ = Cardiac Output (or total perfusion),
[C(a-v)O2] X 10
where VO2 = O2 consumption
C(a-v)O2 = Arteriovenous O2 Content = (1.34)(Hb)[S(a-v)O2] + (0.003)[P(a-v)O2]
N = 4 6 vol% or where > 6 ~ CO (maybe trx w fluid intake)
and < 4 ~ CO (septic shock or anemia may be indicated)
If PvO2 after PEEP, then QT demonstrated; therefore PEEP to previous level
RQ = V/Q = 4.2/5.0 = 0.8 = N
Lab Data
Air bubble - should be suspected in an ABG when PO2 + PCO2 > 140 Torr on RA
Sputum:
Green ~ pseudomonas (foul smelling)
Yellow ~ WBC's or staph
Color vs. disease:
CB = viscous yellow or green
CF = viscous yellow or green
PE = Pink & frothy
Asthma without infection = Clear, white
Electrolytes:
Na+ = 135 145 mEq/L; ~ 140; Na+ = muscle weakness & difficult vent weaning
K+ = 3.5 5.0 mEq/L; ~ 4; K+ = muscle weakness & AVF; cardiac arrhythmias &
flatted "T" wave; difficult vent. Weaning
Cl = 95 105 mEq/L; ~ 100; Cl- = K+ also ; Cl- = weakness
Ca+ = 4.25 5.25 mEq/L; ~ 5; Ca+ = muscle weakness & difficult vent weaning
Others:
WBC > 11k = infection; > 17k = severe infection
Sweat Chloride Test - for CF; positive > 60 mEq/L
HTLV-III ~ test for HIV infection
L/S Ratio = N = 2:1; 1.5:1 = 50% chance RDS; 1:1 = 90% chance RDS (start surfactant)
Umbilical ABG = Radial ABG
Cardiac Enzymes - Lab blood test run to determine if MI occurred
BUN ~ blood/urea/nitrogen = in renal failure
HbCO measurement is an effective test for smoking cessation program noncompliance
Pathology:
Tension Pneumothorax - suspect when PEEP, with suddenly restless, agitation,
BS on a lateral side, asymmetrical chest movement, tracheal movement away from midline; Trx - insert Lg bore needle/rubber catheter into 2nd (between 2&3) intercostal space.
Severe COPD - typical ABG's
PaO2 = 50 - 65 Torr
(chemoreceptors are activated in this range)
PaCO2 = 50 to 60 Torr
(respiratory acidosis)
pH = 7.30 - 7.35;
(partly compensated respiratory acidosis)
HCO3- = 34 - 37 mEq/L
(metabolic alkalosis compensation)
Note - chemoreceptors not depressed until PaO2 ~ >70 Torr
Try NIPPV (BiPAP) first before intubating b/c hard to wean COPDers from CMV
I-Hold or Ipause = helps to distribute Vt more evenly to all lung areas; Gas diffusion,
intrathoracic pressure, atelectasis, P(A-a)G & oxygenation
Percussion ~ tapping over pt.s chest & listening to the sound
Flat sound - over areas of sternum, muscles, atelectasis (tissue or bone)
Dull sound - over areas that are fluid filled (heart, liver, pleural effusion, pneumonia)
Resonant – normal
Hyperresonant – over hyperinflated areas i.e. COPD, Status Asthmaticus
Palpation ~ to touch for, or listen to:
Abnormalities of anatomy or areas of tenderness: ie.: tracheal shift, fractured ribs
Tactile fremitus – “99” is spoken with changes in vibrations felt
Vocal fremitus – 99’ is spoken with normal air muffling heard via stethoscope
IPPB indicated post-op for a sedated pt. requiring prevention of atelectasis trx
when IS not tolerated
PFT Rules:
Interpretation of Results
# > 15% = significant response (improvement) to bronchodilator
mild, moderate and severe
Inspiratory flow = N = 2530 L/m
When interpreting PFT results, look at the choices~ 3 incorrect choices will type a
wrong pathology (i.e.: restrictive vs. obstructive). Choose the other single type.
MVV - performed for 5 -12 sec only (Sills); 10, 12, 15 sec's (Persing); @70-120 bpm
Geisler Tube Ionizer- a nitrogen analyzer used to measure ing exhaled N2 during
inspiration of 100% O2 for the determination of RV, FRC and TLC\
However, use helium washout with COPD pts b/c 100% O2 not used
Physiology Calculations:
Alveolar-Air Equation
PAO2 = (PB - PH2O)FIO2 - PaCO2(1.25); simplify where
shortcut
PAO2 = (7)O2% - PaCO2 + 10
i.e.: PB = 747, FIO2 = 50 and PaCO2 = 35
= (7 X 50) - (35+10) = 350 - 45 = 305 Torr
Desired FIO2 ; where FIO2 = PaO2 therefore divide; i.e.: where FIO2/PaO2 = 1; or
Desired FIO2 = Actual FIO2
Desired PaO2
Actual PaO2
simplified
Desired FIO2 = (Desired PaO2) X (Actual FIO2)
Actual PaO2
Also via math: where (↑)(↓) = (↓)(↑) or (↓)(↑)= (↑)(↓)
Bubble in ABG if:PaO2 + PaCO2 > 140 Torr on RA; {should be < or = with (A-a)G}
Dead Space:
Anatomic normal: VD anatomic = 1 ml/lb. IBW = 2.2 ml/kg IBW
Intubated Pt.: VD Intubation = 0.5 ml/lb. IBW = 1 ml/kg IBW
↑VD = ↑ PaCO2 (i.e.: pulmonary emboli)
Capillary Refill = N = or < 3 sec.; If
> 3 sec. = indicates ↓perfusion, hypotension or a cold extremity
Cyanosis ~ 5 g/dL Hb is unsat.: or Hb > 5 g/dL
Oxygen Content = CaO2 = (1.34)(Hb)[SaO2] + (0.003)[PaO2]
Where N = 15 20 vol % (NO REFERENCE)
IBW Ht.
5'0"
5'2"
5'4"
5'6"
5'8"
5'10"
6'
M(lb./Kg)
106/48
118/54
130/59
142/65
154/70
166/76
178/81
F(lb./Kg)
105/48
115/52
125/57
135/61
145/66
155/71
165/75
Peak Flow Conversions:
50 L/min = 0.83 L/sec
40 L/min = 0.67 L/sec
30 L/min = 0.5 L/s
Cstatic (adult) = Nadult = 100 ml/cwp
Nventilator = 6070 ml/cwp
Cst (neonate) = Nneonate = 5 ml/cwp (3 Kg)
Cst = N = Vt exh________
Pplat - PEEP
Cdyn = N = Vt exh________
PIP - PEEP
Raw = PIP - Pplat / # L/sec ;
Nnonintubated = 0.6 2.4 cwp/L/s;
Nintubated = 5 cwp/L/s
NBTsat = 47 mmHg (PH2O) = 44 mg H2O/Lgas
Pharmacology
Mucomyst - ONLY adm for thick & tenacious secretions i.e.: Bronchiectasis &
CF; also: can bronchospasms
Lidocaine(Xylocaine) - instilled directly into ET tube - will cease coughing due to
bronchospasm (see cardiac conditions below) and
- also adm for ventricular arrhythmias via IV or ETT if IV not available
Sedate & Paralyze is most efficient method of treating combative pt on CMV
Valium (diazepam) - a sedative commonly administered during a bronchoscopy\
(a short acting antianxiety med.)
Versed (midazolam) - a sedative commonly administered during a bronchoscopy
(a short acting barbiturate)
succinylcholine (Anectine) - muscle relaxant facilitates intubation;
paralysis X 5', 2 mg (should add sedative)
pancuronium (Pavulon)- paralysis while on CMV; reversed with Tensilon (neostigmine)
nitroprusside sodium (Nipride)- a potent fast-acting peripheral vasodilator to BP(hypertension)
Inderal - adm to BP (hypertension)
Servanta (artificial surfactant) - indicated for RDS with CXR revealing ground-glass appearance
or L:S < 2:1; adm. 12-24 hrs after symp. appear; PaO2 will as atelectasis reverses
Narcan - reverse effects of narcotics
Hypertonic Saline - 1.8% (2 X 0.9) to induce cough
Theophylline - AOP (apnea of prematurity); an oral Bd in COPD; 10 20 mg/L
Added to regime only after albuterol, Atrovent & IV steroids fail to reverse B.spasm
Tobramycin (Tobi)- antibiotic(pseudomonas); 300 mg X 2/day aerosolized
digoxin (Lanoxin) - adm to SV and CO b/cpumping action of heart i.e. CHF
dornase alpha (Dnase)- trx copious secretions of CF; adm. 1 X /day aerosolized
Atropine - adm to HR (rev. bradycardia): can occurrence of PVC's if present
dopamine (Inotropin) - adm to BP; also HR after atropine failed
nitric oxide - inhaled to trx PVR; a pulm. vasodilator; 10 ppm initial, where >20 ppm is toxic
Bretylium - for pulseless V-tach and V-fib
epinephrine - for pulseless V-tach and V-fib; also a standard for CPR to BP and HR;
NOT if PVC's present as can their occurrence
Mestinon (pyridostigmine Br.) - for trx of MG (cholinesterase inhibitor); a neostigmine
prototype
Mannitol (osmitrol) - adm to ICP (# >25 cwp), a neurologic diuretic
Luminal (phenobarbital) - sedative - hypnotic (barbiturate) - for fighting CMV
Dilantin - Trx seizure activity
Medication vs. Cardiac conditions:
Lidocaine - trx. Ventricular Fibrillation, Ventricular Tachycardia & PVCs
Epinephrine - trx. Ventricular Fibrillation, Sinus Arrest & Asystole
Atropine - trx. Sinus Bradycardia & Asystole
Other:
- Stop bronchodilator if HR > 20 b/m or >20%
- med. dose will adverse reaction
CSE - Assessment for Level of Respiratory Distress
CMV
Ventilator function - quick check of vent for appropriate settings/function
Ability to pass suction catheter - ensures tube patency from secretions/kink
BS - to check for bilateral inflation or adventitious (bad) sounds
Chest percussion - assessing percussion note can help diagnose pul. problem
Manually ventilate - to assess compliance and Raw
Chest excursion - unequal or asymmetrical chest movement
Heart rate - to assess level of distress
Tracheal shift - palpate suprasternal notch for midline or shifted (pneumothorax)
Quick Assessment ~ Choose ONLY those assessments that can be performed visually &
at bedside (stage 1 & 2; No ABG, CXR, CBC, etc.)
CSE - POSSIBLY SELECT ON THIS EXAM
Muscle tone - pt with NM disease or premature infant
Clubbing - consider age of pt. (except CF adolescents)
Deep tendon reflex - differentiates GB vs. MG b/c weakness () with GB diseased
pt vs. normal in MG (MG/Myasthenia Gravis; GB/Guillain-Barre’)
QT - for pt with cardiac disease only
PAP - only for cardiac pt or where a Swan-Ganz catheter is already inserted
PvO2 only where a Swan-Ganz catheter is already inserted
Allen's test - only before performing an arterial stick at the wrist
Ability to swallow - only in NM disease pt (swallowing difficuly may require intubation)
Swallow ability- for toddler R/O epiglottitis or upper awy obstruction
CVP - only a cardiac pt. or where a central line has been inserted
ABG's - evaluates ventilatory & oxygenation status; however, this painful test
may NOT be necessary if pt is resting comfortably or SpO2 = N
ICP - only in head trauma pt's; zero on RA and ONLY before attachment
Tracheal position - ONLY when pneumothorax is suspected
Serum glucose level - only for diabetes or neonatal pt's
Breathe mints - are helpful after pentamidine trx b/c of bad taste
Pulmonary angiogram - procedure to detect pulmonary embolus
Response to painful stimuli - select only when pt is unconscious
Babinski reflex - bottom foot rubbed with dull object, toes inward = N,
toes outward = neurologic defect ONLY i.e. brain damage, - GB; +MG
Gag reflex - tested with NMD determines level of paralysis; also unconscious or
semiconscious - determines depth of depression; caution b/c can cause
vomiting and aspiration; assess level of hazard chocking with MG & GB but
not performed if pt. eating/drinking properly
Electromyography – EMG tests muscle weakness & endurance of NMD i.e. MG
Sx - ONLY PRN; Never q10 or q20, etc.
ABG - ONLY PRN; Never q day
Urine Output - measured (40 ml/hr) to assess cardiac (perfusion) or kidney failure
Bilateral grip test - in NMD tests muscle endurance via hand muscles
CBC (infant) - 30k at birth, 18k at 1 wk, 11k at 2 wk (Wilkens; Assess, p223)
Post Extubation - if offered, choose SVN with Epinephrine X 2 over 2 hour & or
Beclovent MDI X 2 over 2 hour (remember: only if offered)
IPPB with FIO2 1.0 ~ Choose when ABG demonstrates 1) poor ventilation &
2) poor oxygenation and more assessment information is needed
Carotid Artery Message or Valsalva Maneuver ~ common nonelectrical trx for SVT
(Supraventricular Tachycardia) via vagal stimulation.
Lukens Trap- used for collection of sputum during sxing
Expiratory Retard- use to help splint obstructive awys (ie.: wheezes) to remain open
Heimlich Maneuver- performed 1st during choking (do not clap on pts. back)
Urine output and color – if a trauma patient b/c can demonstrate internal bleeding
Peripheral Pulses – Only if cardiac pt. & to evaluate foot perfusion (dorsalis pedis)
CSE - ALWAYS SELECT
VS - should always be a part of pt evaluation; Also
BP - to assess CV status
Pulse & respiratory rate - assess CP status
Body Temperature - assess presence of infection
LOC - important to evaluate in any pt.
BS - essential to evaluate adventitious air movement through areas of the lungs
MIP - evaluates respiratory muscle strength
cough effort & production - can pt protect airway & presence of Pul infection
Vt spon. - evaluates respiratory muscles for effective alveolar ventilation
VC - evaluates effectiveness of cough to protect airways (should be >1,000 ml)
Sputum production - can be diagnostic for infection or other conditions
CBC - to determ O2 capacity (Hb) and presence of infection (WBC>11K)
CSE - DO NOT SELECT ON THIS EXAM
Hering-Breuer reflex - stretch receptors cannot be evaluated
bowel sounds - provides little relative information about respiratory status
VD/Vt ratio - time consuming and difficult to assess
O2 Consumption - hard to tolerate by pt; is also expensive and time consuming
MVV - performed in the PFT lab, it is stressful and offers little information
Moro reflex - performed on infants (startled, they raise their arms up & out)
EEG – can be mistaken for ECG or EKG
PA CXR – must be an AP view ONLY (pt.s are very sick & can not stand)
100 ml VD is NEVER added to spontaneous breathing pt b/c will PaCO2
Silverman Score - newborn assessment
Dubowitz Score - estm. gestational age of newborn
DO NOT ORDER ON INFANTS
PEFR, MIP, VC
CSE - ALMOST ALWAYS SELECT
SpO2 - Except for suspected HbCO poisoning
MIP, VC, RRspon, Vt spon., RSBI, BS, VS, T, CBC, LOC, CXR, Pulse, when
considering weaning, even if on A/C= 12 but without major acute health issues
Also called bedside spirometry; weaning parameters