Neuroscience 20b & c – Personality & Personality Disorders
advertisement

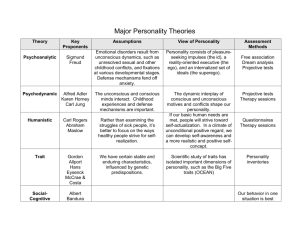
Neuroscience 20b & c – Personality & Personality Disorders Anil Chopra 1. Show how personality can be identified as a separate level of functioning from other mental disorders 2. Illustrate the effect of personality disturbance on the outcome of mental disorders 3. Describe some of the treatments for personality disorder 4. Give a brief idea of how the UK government deals with dangerous and severe personality disorder Schizophrenia - 1 in 100 affected - Onset 15-35 years. - More common in city areas. - Positive symptoms o Hallucinations etc o Delusions, o Thought disorder, poor concentration, not finishing off work, muddled thinking o Feelings of being controlled, - Negative symptoms o Lack of drive o Inability to look after oneself. o Losing insight into reality - Strong genetic link (1 in 10 with parents, 1 in 2 for identical twin) - Offspring of wartime famine has increased risk due to poor nutrition. - Drugs and alcohol exacerbate symptoms Treatment for Schizophrenia Cognitive Behavioural Therapy – CBT for Psychosis - Coping with psychotic symptoms (e.g. reading aloud, listening to music) - Dealing with delusion - Dealing with beliefs about self and others. - Discussing family interventions and reactions Double Bind: a communicative situation where a person receives 2 contradictory messages. People suffering from schizophrenia are believed to be more or less vulnerable as a result of biological or psychological factors. This can arise from previous events that have taken place in the person’s life, problems that occur when an environmental stress is present even at a low level. Personality Personality is defined as how people differ on life history, needs, motives, goals, traits and specific behaviours: Eysenck’s theory: he proposed 3 factors to personality, extraversion – E (positive traits), neuroticism - N (negative traits), and psychoticism (evil traits), which could be measured and analysed by factor analysis to produce 4 main personality types originally proposed by Hippocrates. • High E, High N (‘Choleric) • Low E, High N (‘Melancholic’) • High E, Low N (Sanguine’) • Low E, Low N (‘Phlegmatic’) Costa and McCrae: proposed 5 personality traits using the anagram OCEAN: • Openness - creative, independent, seeking new experiences • Conscientiousness - reliable, persistent, hardworking • Extraversion - sociable, outgoing, cheerful • Agreeableness - cooperative, trusting, conciliatory • Neuroticism - nervous, worrying, subject to negative emotions DSM IV Personality Disorder – enduring patterns over a range of social and personal contexts. Generally inflexible and persistent across a broad range of personal and social situation. The DSM – Diagnostic and statistic manual of mental disorders has guidelines on whether people can legally be defined as having a personality disorder. It groups the disorders into 5 different clusters: CLUSTER A (Odd, eccentric): • Paranoid: distrust and suspiciousness • Schizoid: social detachment, restricted emotional expression • Schizotypal: acute discomfort in close relationships, cognitive or perceptual distortions, and eccentricities of behaviour CLUSTER B (Dramatic, emotional): • Antisocial: disregard/violation of others’ rights • Borderline: instability in interpersonal relationships/self-image/affects, and marked impulsivity • Histrionic: excessive emotionality/attention seeking • Narcissistic: grandiosity, need for admiration, and lack of empathy CLUSTER C (Anxious): • Avoidant: social inhibition, feelings of inadequacy, and hypersensitivity to negative evaluation • Dependent: submissive and clinging behaviour related to an excessive need to be taken care of • Obsessive-Compulsive: preoccupation with orderliness, perfectionism, and control. Treatment Of Personality Disorders Livesely: The goal of personality disorder is to adapt people’s traits so that they are socially acceptable, not to change them. Livesely proposed that they are 4 stages to treatment: • Problem recognition - how personality problems affect other aspects of his/her life • Exploration - patient is helped to recognise connections between different aspects of thinking, feeling and behaviour, to reframe negative thoughts more adaptively, and to observe and monitor his/her behaviour • Acquisition of alternative behaviours, development of new skills and inhibition of maladaptive patterns of behaviour • Consolidation and generalization - the application of new skills to everyday. Young: He proposed a schema-focused cognitive therapy. This took place in 2 phases: Phase 1 – Assessment and education: • Identify & educate the patient about his/her schema • Link schemas to presenting problems & life history • Bring patient in touch with emotions surrounding their schema (imagery, role play) • Observe patterns in therapy sessions • Identify dysfunctional patterns of maintenance, avoidance & compensatory behaviour Phase 2 – Change techniques • Restructure thinking related to schema: develop a “healthy voice” • Experiential exercises to rediscover early emotions: anger, distress etc • Institute behavioural & interpersonal changes • Reframe past events • Utilise therapy relationship to understand schemas & carry out limited “parenting” Government Acts Mental Health Act 1983: this defines mental illness as “persistent disorder or disability of mind…which results in abnormally aggressive or seriously irresponsible conduct” It outlines how those with mental illness should be treated according to their condition: » Detention in hospital only if the individual is likely to benefit from treatment, including prevention of deterioration » Special Hospital if the individual presents a grave and immediate danger and cannot be treated in lesser security Psychopathy It also defines the criteria for a patient to be “psychopathic” using the PCL-R (Psychopathy Check-List Revised) and has a series of 20 items, each of which can be rated with either 0 points (absent), 1 point (partial), or 2 points (present). A score of 30 or more indicates psychopathy. Treatment for psychopathy involves: • Highly structured environment • Strong staff support and supervision • Active and entertaining programme • Control treatment interfering behaviours • Focus on risk reduction interventions • Emerging evidence of brain dysfunction