Transfusion Reaction Codes - Ohio State University : Pathology
advertisement

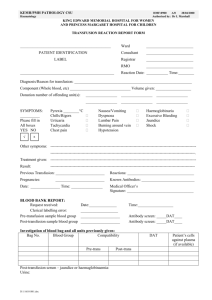
The Ohio State University Medical Center Department of Clinical Laboratories TRANSFUSION REACTION WORKUP TEST CODES TEST CODE Lab Results TRLR1 TRLR2 TRLR3 TRLR4 TRLR5 TRLR6 TRLR7 TRLR8 TRLR9 TRLR10 Signs and Symptoms TRSS1 TRSS2 TRSS3 TRSS4 TRSS5 TRSS6 TRSS7 TRSS8 TRSS9 TRR6.18FA/01 Effective Date: 01/20/09 DESCRIPTION The clerical check showed no errors, no hemolysis was observed and the direct antiglobulin was negative. No laboratory evidence of acute hemolytic transfusion reaction. The clerical check showed no errors and no hemolysis was observed. However, the direct antiglobulin test was positive on both the pre and post transfusion specimens. The clerical check showed no errors. However, hemolysis was observed in the post transfusion specimen. The direct antiglobulin test was negative. The clerical check showed no errors and no hemolysis was observed. However, the direct antiglobulin test in the post transfusion specimen was positive. The direct antiglobulin test was positive with anti-IgG reagent. The direct antiglobulin test was positive with anti-C3d reagent. The DAT was with both anti-IgG and anti-C3d reagent. The elution test was negative for autoantibody or alloantibody. The gram stained smear of the implicated blood bag was negative for organisms. A sample was sent for culture and sensitivity. The gram stained smear of the implicated blood bag was positive for organisms. Culture and sensitivity results are pending. The signs and symptoms are consistent with an urticarial allergic transfusion reaction. The signs and symptoms are consistent with an anaphylactoid or anaphylactic transfusion reaction. The documented signs and symptoms are most consistent with febrile nonhemolytic transfusion reaction. The documented signs and symptoms are most consistent with a febrile nonhemolytic transfusion reaction although bacterial contamination of the transfused blood component is a possibility. The reported signa and symptoms are consistent with circulatory overload (hypervolemia). The reported signs and symptoms maybe caused by transfusion related acute lung injury (TRALI), although hypervolemia may cause similar signs and symptoms. The signs and symptoms suggest possible bacterial contamination of the transfused blood component. The reported signs and symptoms and laboratory evaluation are most consistent with an acute hemolytic transfusion reaction. The reported signs and symptoms are most likely unrelated to the transfusion. Transfusion Service Page 1 of 3 The Ohio State University Medical Center Department of Clinical Laboratories TRANSFUSION REACTION WORKUP TEST CODES Pathophysiology TRPP1 TRPP2 TRPP3 TRPP4 TRPP5 TRPP6 TRPP7 TRPP8 TRPP9 TRPP10 TRPP11 TRPP12 Urticarial and anaphylactic reactions are generally considered to result from antibodies in the patients reacting with proteins or other allergens in the transfused plasma. Rarely, IgG antibodies against IgA may be present in the IgA deficient patient. Febrile reactions are generally considered to result from cytotoxic or agglutinating antibodies directed against donor leukocytes (neutrophils and lymphocytes). The febrile reactions may also occur as a result of accumulated cytokines in the transfused red blood cells or platelets. Circulatory overload may be moderated by slow infusion of blood products, limiting the infusion of oncotic fluids (plasma) and the judicious use of diuretics. Transfusion related acute lung injury (TRALI) is thought to be caused by HLA or neutrophil antibodies in the donor plasma which activate neutrophils and complement in the patient’s pulmonary vasculature, resulting in pulmonary edema. The hallmark is hypoxia, with chest radiograph indicating noncardiogenic pulmonary edema. The DAT pre and post transfusion specimens indicate the findings unrelated to transfusion. A positive direct antiglobulin test (IgG), with negative elution test, may be caused by drug therapy, paraproteinemia or high dose intravenous immune globulin. A positive direct antiglobulin test (C3d), with negative direct antiglobulin test with anti-IgG) may be caused by cold agglutinins, drug therapy or autoimmune disease. A positive direct antiglobulin test with anti-IgG and positive elution test, may indicate warm autoimmune hemolytic anemia. The positive direct antiglobulin test with both anti-IgG and anti-C3 with negative elution test may be caused by drug therapy, paraproteinemia or high dose intravenous immune globulin. The positive direct antiglobulin test with both anti-IgG and anti-C3 with positive elution test may be caused by warm autoimmune hemolytic anemia. The positive direct antiglobulin test with both anti-IgG and anti-C3 with positive elution test is caused by ABO incompatible platelet products. The patient may show anemia, requiring RBC transfusion. Hemolysis, with negative direct antiglobulin test, may be caused by mechanical trauma to the RBCs, such as difficult venipuncture or cardiopulmonary bypass. Recommendations TRREC1 Urticarial (hives) reactions can be treated and/or prevented with administration of antihistamines. TRREC2 Anaphylactic reaction can be treated with administration of intravenous antihistamines, intravenous steroids, and in severe cases, epinephrine. TRREC3 Febrile nonhemolytic transfusion reactions can be treated and prevented with administration of antipyretics, e.g., acetaminophen. TRREC4 Treatment of TRALI should be supportive, with respiratory support and oxygen. Patients usually recover in 3-4 days. TRR6.18FA/01 Effective Date: 01/20/09 Transfusion Service Page 2 of 3 The Ohio State University Medical Center Department of Clinical Laboratories TRANSFUSION REACTION WORKUP TEST CODES TRREC5 TRREC6 TRR6.18FA/01 Effective Date: 01/20/09 Treatment of acute hemolytic transfusion reactions should include adequate fluid and diuretic administration to protect renal function, support of blood pressure, administration of additional compatible blood products as necessary, and monitoring for renal failure, coagulopathy, and shock. No changes in blood product selection or therapy are recommended. Transfusion Service Page 3 of 3