EDEMAS IN BURNS
advertisement

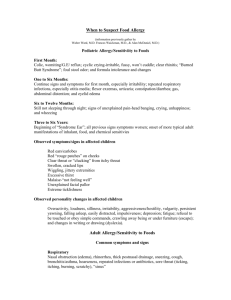
Update: February 24, 2002 Module C (III. and IVth year). Basic clinical problems Course 8: Edema. Summary of the syllabus: Disorders of water and sodium balance – Physiological and pathophysiological aspects Pathological anatomy of edema General principles of pharmacological treatment Clinical causes of edema Edema of cardiac and vessel origin Edema in renal diseases Edema in liver diseases Edema in connective tissue diseases Hormon induced edema and edema due to disorders of nutrition Edema in pregnancy Brain edema Upper airways edema Allergic edema Edema in burns I. Physiology and pathophysiology of edema / 4 hours MUDr. Klára Bernášková Disequilibrium of sodium and water metabolism. * basic clinical terms. a) distribution of body fluids into compartments b) serum osmolality distribution into intracellular and extracellular space brain cells and extracellular space osmolality c) osmotic gap d) body fluid distribution into intravascular and extravascular space (Starling´s hypothesis) * physiology and pathophysiology. a) regulation of volume homeostasis natriuresis and diuresis subject to blood pressure effective circulating blood volume renin-angiotensin-aldosterone system sympathetic nervous system atrial natriuretic factor (ANF, atriopeptide) b) osmoregulation adiuretin- vasopressin concentration and dilution of urine in kidneys c) integration of the various circuits and parameters of volume homeostasis d) effect of hypernatremia and hyponatremia on the central nervous system e) oedema formation * clinical and pathogenetic aspects a) overview of symptoms in disequilibrium of internal and external fluid homeostasis b) oedema types of oedema c) internal fluid disbalance hyponatremic syndrome hypernatremic syndrome II. Pathological anatomy MUDr. Jana Náprstková * oedema of cardiac origin * oedema of renal origin- in diseases characterised by the nephritic or nephrotic syndrome * angioneurotic oedema * lymphoedema III. Pharmacological treatment of oedema / 3 hours MUDr. Jitka Patočková Diuretic agents - definition of the whole group, - main principles in the mechanism of action Classification of Diuretics : - according to the mechanism of action - according to the intensity of the diuretic effect Main groups of diuretics : 1) Loop agents main drugs : Furosemide, Ethacrynic acid - mechanism of action (pharmacodynamics), basic pharmacocinetics 2) Thiazides main drugs : Hydrochlorothiazide, Chlorothiazide, Chlortalidone - mechanism of action (pharmacodynamics), basic pharmacocinetics 3) Potassium - sparing diuretics main drugs : Spironolactone, Triamterene, Amiloride - mechanism of action (pharmacodynamics), basic pharmacocinetics 4) Carbonic anhydrase inhibitors main drugs : Acetazolamide - mechanism of action (pharmacodynamics), basic pharmacocinetics 5) Agents enhancing primarily water excretion main drugs : Osmotic diuretics (Mannitol), ADH Antagonists (Li salts, Tetracycline derivates) - mechanism of action (pharmacodynamics), basic pharmacocinetics Mainly used combinations of diuretic agents : loop diuretics + thiazides (acute therapy) thiazides + potassium sparing diuretics (chronic therapy) IV. Causes of edema Edema of cardiac and vessel origin MUDr. Rudolf Špaček,CSc. Edema is defined as a palpable swelling produced by expansion of the intersticial fluid volume. In the development of cardiac edema and edema of vessel origin the rise of capillary hydraulic pressure play the most important role. Increase of capillary pressure is a result of sodium retention and consequent increase of plasmatic volume ( congestive heart failure and cor pulmonale ) or venous obstruction ( acute pulmonary edema, deep venous trombosis). 1. Congestive heart failure Etiology The prevalence of the clinical syndrome of congestive heart failure is about 2-9% and rapidly incerases with age. The most common causes of systolic and diastolic heart failure are ischemic heart disease ( 50% ), hypertension, cardiomyopathies and chronic lung diseases. In forward heart failure the primary disorder is decreased cardiac index followed by decrease of periferal tissue perfusion. The compensatory response is sympathetic - renin - angiotensin - aldosteron system activation which tend to promote sodium and water retention and finally to edema. Clinics The main symptoms are induced by accumulation of fluid and decreased cardiac output. Increased left ventricular end-diastolic and left atrial pressures are transmited back through the pulmonary veins into the pulmonary capillaries. Pulmonary congestion leads to dyspnea, first on effort than paroxysmal nocturnal and finally on rest. Typical physical finding are rales on the lung bases left ventricle dilatation, S3, pulsus alternans or peripheral cyanosis. Symetrical pitting leg edema finally radiates proximally. Usually there is also increase in jugular venous pressure, hepatomegally, fluidothorax and possibly ascites or anasarca. Because of decrease of cardiac output patients suffer from weakness and fatigue. The symphatetic stimulation leads to tachycardia and perspiration. Patients with coronary heart disease may complain also of chest pain. Diagnosis and assessement Detailed history remain the mainstem approach to etiology and staging of heart failure. We are interested about previous angina pectoris, hypertension, alcohol abuse, virosis, cardiac murmurs or rheumatic fever. Chest X ray help us to distinguish between primary heart or lung disease. In heart failure we find cardiothoracic index over 50% , signs of lung congestion or pleural effusion, mostly rightsided. Cardiac shape is also typically changed in end-stage valvular disease. Normal ECG did not support the diagnosis of systolic heart failure. The gold standard is echocardiographic assessement. It gives informations about ejection fraction of the ventricles, presence of cardiac muscle hypertrophy, pericardial effusion, structure and function of the cardiac valves. Doppler measurements have good correlations with cardiac output, valve gradients, diastolic dysfunction or pulmonary hypertension. Dobutamin echocardiography can discover ischemic dysfunction or presence of hibernating myocardial muscle whose contractilily returns to normal after appropriate revascularisation. Coronary angiography is indicated in all patients with new onset of heart failure especially if associated with chest pain. Therapy First choice therapy in patients with congestive heart failure are ACE inhibitors which can improve short and long term survival and reduce morbidity. Diuretics remove excess of extracelullar fluid, relief symptoms and improved quality of life. We usually start with low dose thiazid diuretic and finally switch to loop diuretic or combination. Chronic use of ACEI prevent loss of potassium during diuretic therapy. Symptomatic improvement can be achieved with digoxin and nitrates. In refractory edema especially in patients waiting for heart transplantation arteriovenous hemofiltration or dialysis take place. Prognosis Patients may expirienced sudden cardiac death or can die for progresion of heart failure. The most important predictors of death are LV ejection fraction < 20%, NYHA III-IV, VO2max < 10ml/kg/min, high LVEDP, CI < 2l/min/m2, complex ventricular arrhythmias, increased concentration of catecholamines and BNP. 2. Cor pulmonale Etiology This disorder is defined as a disturbance of structure and function of the right ventricle as a result of precapillary pulmonary hypertension in chronic lung disease. The most common cause is chronic obstructive lung disease (COLD ). Right ventricular failure may resulting in prominent edema in the lower extremities and perhaps ascites. More often we find normal ejection fraction of the RV at rest and even during exercise and normal glomerular filtration fraction. In these patients edema is a result of hypercapnea, which leads to increased reabsoption of bicarbonates followed by pasive reabsorption of sodium chloride and water in the kidney. Also chronic hypoxemia and consequent vasoconstriction in renal vascular bed and reduction of sodium excretion play a role. Clinics Symptoms are nonspecific. Except of periferal edema we can find exertional dyspnea, fatigue, cough, hemoptysis, chest pain or syncope. More severe RV failure may be associated with anorexia and dyspeptic syndrome due to splanchnic congestion. Developement of ascites is not commmon even in severe pulmonary hypertension. Diagnosis We use the same methods like in congestive heart failure. Other helpfull assessements are spirometry and right side cardiac cathetrisation which can quantify pulmonary hypertension. In some patients pulmonary biopsy may verify the etiology. Therapy In the most common form of the disease caused by COLD the basic is long term oxygenotherapy which can decrease lung vasoconstriction and improve long term survival. Diuretics may improve ejection fraction of both ventricles and remove edema. During chronic diuretic therapy it is recommended to monitor plasmatic levels of kreatinin and urea to prevent excesive loss of extracellural fluids. Developement of metabolic alcalosis and supression of breathing centre is another possible complication of chronic diuretic therapy. Prognosis Moderate to severe pulmonary hypertension and peripheral edema is associated with bed prognosis. These patients 5-year survival is about 30%. 3. Cardiac pulmonary edema Etiology The most common causes of systolic and diastolic LV dysfunction are ischemic heart disease, hypertension, dilated cardiomyopathy, specific diseases of cardiac muscle and heart valvular disease. Increased left ventricle filling enddiastolic pressure radiates backward into the pulmonary vascular bed. As postcapillary pulmonary hypertension get more severe intracapillary pressure + intersticial oncotic pressure overcomes intracapillary oncotic pressure. This leads to transsudation of the fluid first into the lung intersticial space and than into the alveolar space. For limited period of time there is some compensatory incerase in intersticial lymphatic drenage bud after that manifest pulmonary edema appears. Clinics When the pulmonary capillary wedge pressure is over 25 mmHg plasmatic fluid soaks into lung intersticial space which irritates J receptors and compress small bronchi. Main symptoms are dyspnea, tachypnoe, orthopnoe, cough and protodiastolic gallop. Typical wet rales appears at the lung bases during paroxysmal night dyspnea and also spastic fenomena are possible. Intraalveolar edema appears when wedge pressure exceeded 35mmHg. Patient is in orthopnoic position, anxious, pale, sweating and the sputum is pink foamed. Rales are accented and diffuse. Diagnosis We can use the same methods like in other disorders of cardiac origin. Right side cardiac cathetrization help us to distinguish cardiac pulmonary edema from edema of noncardiac origin ( ARDS ) which is associated with normal pulmonary wedge pressure. Therapy Most effective is cause treatment of cardiac pulmonary edema i.e. early reperfusion in acute myocardial infarction, rapid lowering of blood pressure in emergent hypertensive crisis, immediate surgery in mechanical complicatin of AMI or elective surgery in valvular heart disease. Sometimes therapy can be only symptomatic like at present in dilated cardiomyopathy. Supportive measures are inhalation of 100% oxygen, assisted ventilation + PEEP, application of morphin or loop diuretic i.v. and others. In patients with normal or elevated blood pressure use of i.v. nitroglycerin is indicated. In hypotension we should use dopamin alone or in combination with dobutamine. Prognosis The prognosis of the patient with cardiac pulmonary edema depends on its etiology and treatment possibility. 4. Local edema of vessel origin Etiology Most often is localized unilateral edema of one lower extremity due to deep vein system trombosis or deep vein system valves inssuficiency in so called postphlebitic syndrome. Risc factors of deep vein trombosis are age over 40, orthopedic or abdominal surgery, long time bed rest, malignant tumors, congestive heart failure, obesity, varices and hemostatic disorders. Trombus formation leads to increase of intracappilary hydraulic pressure folowed by transsudation of the fluid into intersticial space. Less often edema may be of lymphatic origin due to decrease uptake of intersticial fluids. Lymphatic vessels can be damaged in repeated inflammations, malignant blockade or congenitally. Clinics Edema is usually pale and painfull localized distally of the site of the trombosis. Colateral circulation in superficial vein system is more prominent and painfull palpable resistence is present. During vein slow flow the involved extremity can be cyanotic ( phlegmazia caerulea dolens ). In chronic vein insuficiency except of edema also trofical changes like culf ulcer may be present. Other signs can be nonspecific like increase in erythrocyte sedimentation, leucocytosis or subfebrile temperatures. Diagnosis Gold standard method is contrast venography. Most sensitive and specific noninvasive assessement is ultrasonography with color wave Doppler mapping. Usefull may be also pletysmography and D-dimer estimation which negative predictive value is about 99%. In diferencial diagnosis muscle contusion, joint distorsion, edema associated with leg paresis or Baker cyst in gonartrosis must be consider. Therapy In the presence of deep vein trombosis appropriate anticoagulation is indicated. We can use unfractioned heparin or LMWH and switch to Warfarin after relief of the symptoms. LMWH can be used in uncomplicated outpatients. Prognosis Diseases associated with localized edema usually dont change the longevity unless pulmonary embolization is not a complication. Literature I Málek, J Toman, M Štejfa Doporučení pro diagnostiku a léčbu srdečního selhání Cor Vasa 1998;40(1):K16-28 M Štejfa et al. Kardiologie, Grada Publishing, s.r.o. 1995,s.557 J Widimský Srdeční selhání, Triton, 1996,s.77 E Braunwald Heart disease, 5th edition, 1997,s.1996 Edema in renal diseases MUDr. Miroslava Horáčková, CSc. Oedema in renal disease develops due to 2 different mechanisms: * Primary oedema: retention of salt and water primarily by the kidneys (overflow theory). Suppression of renin-angiotensin system activity, primary suppression of plasma renin and aldosterone. * Secondary oedema: retention of salt and water by the kidneys as a consequence of adaptive measures in decreased plasma volume and decreased effective circulating volume (underfill theory). Plasma renin and aldosterone are elevated, the release of adiuretin- vasopressin is also increased. Differential diagnosis. 1. nephropathy with primary oedema: * some primary glomerulopathies with nephrotic syndrome * acute glomerulonephritis * nephropathy leading to acute renal failure * nephropathy in end-stage chronic renal insufficiency. 2. nephropathy with secondary oedema: * some glomerulopathies, including secondary types, with nephritic syndrome. The nephrotic syndrome (NS) Pathogenesis: injury to the glomerular membrane is always involved in the pathogenesis of this syndrome. This injury leads to greater membrane permeability for plasma proteins. Adaptation events lead to secondary oedema. In some patients with the NS, intra-renal factors that cause primary salt and water retention (sustaining primary oedema formation) may be in play. Most probably, though, a combination of both these factors leads to the development of oedema. Clinical and laboratory findings: oedema generally involves the lower extremities in mobile patients and the sacral region in bed-ridden ones. Oedema easily forms in areas with little fibrous tissue (periorbital region, scrotum). In advanced disease, a hydroptic syndrome occurs with increased subcutaneous oedema of the lower extremities and abdomen, the collection of fluid in the peritoneal, pleural and pericardial space. In extreme cases, non-cardiac pulmonary oedema may develop. In some patients, there are concurrent signs of effective circulating volume contraction (orthostatic hypotension, orthostatic vertigo, tachycardia, increased sensitivity to diuretic administration- accentuation of the pathological signs of effective circulating volume contraction). Typical laboratory findings include: hypoproteinemia and hypoalbuminemia, dyslipoproteinemia, (increased cholesterol plasma concentration), and hyperfibrinogenemia due to secondary increased proteosynthesis in the liver, anaemia due to defective iron utilisation because of loss of transport proteins, hypogammaglobulinemia due to renal losses of immunoglobulins. Normo/hyponatremia, depending on the ECT/ICT state of equilibrium. Diagnosis and differential diagnosis: NS develops following injury to the glomerular membrane due to immunological and non-immunological insult. If the underlying cause is known (approx. 20% of cases) then secondary NS is diagnosed. If the underlying injury is not known, the diagnosis of primary (idiopathic) NS is made. Examination: Oedema due to the NS is characterised by: * hypoproteinemia, hypoalbuminemia, hypogammaglobulinemia, decreased antithrombin III * hypercholesterolemia, prolonged prothrombin time (increased concentration of haemocoagulation factors, fibrinogen!) * hyponatremia (dilution) and hypokalemia (in secondary hyperaldosteronism). Treatment: in secondary NS, one must consider removing the underlying cause of increased basal membrane permeability. In most cases of NS only symptomatic treatment is possible- treating oedema by pharmacological, and in exceptional circumstances, non-pharmacological means. Treatment of the hypercoagulation syndrome. The effectiveness of statin administration in the treatment of attending hypercholesterolemia depends on the stage of renal insufficiency. Prognosis: in a small percentage of patients, the identification of underlying causes and their causal treatment is possible. In most patients, though, this is not so and their prognosis is hence clear. In some cases, immunosuppressive therapy may successful. This treatment, though, is attended by a number of complications which, to a great extent, affect the prognosis of patients as well as their ability to continue working. Nephropathies accompanied by „primary oedema“ Pathogenesis renal retention of salt and water represents the key element in the etiopathogenetis. Retention is caused by various mechanisms, depending on the underlying nephropathy. Typical clinical and laboratory findings: the most significant clinical symptoms include hypertension caused by extracellular compartment expansion, and left heart insufficiency or failure with pulmonary oedema. Brain oedema with the development of neurological symptoms such as qualitative alterations of the level of consciousness (amentia), seizures as well as quantitative alterations (coma) may also occur. Patients often have oligo/anuria (decreased micturition). Typical laboratory findings include hyperazotemia (elevated creatinine and BUN), especially in cases of acute or end-stage chronic renal failure, and hyperuricemia. The extent of proteinuria depends on the underlying nephropathy. The same applies to urinalysis findings. End-stage chronic renal failure is characterised by anaemia, hypocalcemia, hyperphosphatemia, normo/hyponatremia (dilution), elevated EFNa (relation between the amount of Na excreted and the glomerular filtration rate), hyperkalemia, metabolic acidosis with anion gap. Diagnosis and differential diagnosis: The main step in the differential diagnosis is distinguishing between acute and end-stage chronic renal failure. The architecture and size of the kidneys on ultrasound imaging, laboratory findings and special tests (special laboratory findings: ASLO, C3,C4, ANCA, ANA, anti-dsDNA, anti-GBM, urine cytology, renal biopsy) in relation to the history and overall clinical state may provide helpful clues. Examination: Oedema and concurrent signs of extracellular volume expansion, oligo/anuria and hyperazotemia should be categorised as possible causes of renal insufficiency (pre-renal/renal/postrenal), depending on laboratory tests and results of imaging methods (CAT, US). Treatment: severe hyperazotemia, metabolic acidosis, hyperkalemia and hyperhydration together with progression of pulmonary oedema and oligo/anuria require urgent treatment, regardless of their aetiology. Such treatment , apart from conservative measures (salt and water replenishment in accordance to hemodynamic parameters and diuresis, diuretics, urological invasive intervention) consists of one of the haemo-purification methods. The choice of method depends on the technical facilities available, the erudition of the medical staff involved and on individual choice, always keeping in mind the constellation of laboratory findings and clinical signs and symptoms including haemodynamic parameters (hemodialysis, CVVH, CVVHD). Prognosis. Patient prognosis depends mainly on the presence or absence of chronic irreversible renal failure. Most patients with chronic renal failure require one form of life-long kidney function replacement (hemodialysis, peritoneal dialysis, transplant). Prognosis depends on the adaptation to this replacement. This is given by the underlying nephropathy, multiple morbidity and age. Acute renal failure need not always be a cause of permanent disability. Much depends on the aetiology, possibilities of treating the underlying cause and other factors (age, multiple morbidity, complicationsfailure of other vital organs). Idiopathic oedema. Pathogenesis: there is no consensus on the cause of idiopathic oedema. It is possible that increased capillary permeability, hyperaldosteronism, decreased effective circulating volume (especially when trying to treat oedema with diuretics) and hyperprolactinemia may play a role. Clinical and laboratory findings: women are practically always affected. They complain of generalised oedema. oedema of the lower extremities, oedema of the fingers or of the palpebra. Sometimes the oedema is cyclic and dependent on the phase of the menstruation cycle. Usually, there are discrepancies between the objective findings and the intensity of patient complaints („true psychic oedema“). Laboratory findings are non-specific. Diagnosis and differential diagnosis. oedema caused by increased capillary hydraulic pressure and oedema due to decreased colloid-osmotic pressure must be ruled out. Oedema due mainly to increased capillary permeability is usually easy to distinguish (trauma, burns, inflammation, sepsis, ARDS, treatment with interleukin-2). Allergic aetiology should be sought. Treatment: pharmacological intervention is not possible. Diuretics aggravate symptoms and their withdrawal leads to a marked rebound phenomenon with weight gain due to increased fluid retention. This phenomenon often leads to dependency on diuretic treatment with all the negative consequences this entails (pseudo-Bartter´s syndrome, kaliopenic nephropathy, severe hypokalemia with arrhythmia, kaliopenic paralysis). Psychotherapy is recommended. Prognosis: If no treatment with diuretics is attempted, the prognosis is good, and there is no change in the patients ability to work. Incorrect treatment with diuretics and dependency on these drugs may lead to serious complications including sudden death from malignant arrhythmia and the development of renal insufficiency due to kaliopenic nephropathy. Edema in liver diseases MUDr. Blanka Cieslarová Typical manifestation of edema in liver diseaseas is ascites. Ascites = fluid in abdominal cavity. ETIOLOGY: combinations of some factors: 1. decrease of oncotical pressure - hypalbuminaemia 2. portal hypertension 3. lymphostasis 4. increase retention of water and natrium 5. decreased renal perfusion and redistribution of renal circulation 6. endocrinal changes - secondary hyperaldosteronism, elevated secretion of renin and ADH 7. elevated activity of sympathetic division 8. elevated concentration of prosthaglandins PATHOGENESIS: 1.theory: primary are hemodynamic changes, when the renal blood flow is decreased, renal cortex ischemia, impairing of renal functions, compensatory is elevated Na retention to keep plasmatic volume, thus the complete vascular volume is elevated. 2. theory: primary portal hypertension with fluid accumulation in abdominal cavity decreases plasmatic volume and sequential regulatory mechanisms elevate Na retention to “keep” plasmatic volume. CLINICAL PICTURE: SUBJ: sensation of full abdomen, abdominal discomfort, flatulence (“ the wind comes before the rain”), the thirst, sometimes edemas of legs, weight changes, breathing complaint. OBJ.: fatigue appearance, dry skin and mucosa, enlarged abdominal volume, colateral circulation, sometimes “ caput medusae”, or striae. DIAGNOSIS:detection of ascites during physical examination is possible if there is about 2000ml of fluid in abdominal cavity present ( positive undulation). Ultrasonography detects amount fluid of 200ml, the same does CT examination and certainly laparoscopy. DIAGNOSTIC PUNCTURE: in each ascites. In cirrhosis is ascitic fluid clear, or with yellow or green hue. The ascitic fluid is transudate ( specific weight is 1018, lower content of protein: 10-20g/l). Rivalt test: positive in exudate, negative in transudate. Sediment: in cirrhosis only solitary erytrocytes and leukocytes, total amount to 500/mm 3 DIFFERENTIAL DIAGNOSIS: 1. liver congestion ( right-side cardiac failure , constrictive pericarditis, Budd-Chiarri syndrom) 2. infections ( bacterial, tbc, parazital, mycotic) 3. primary and secondary tumors 4. hypalbuminaemia ( nephrotic sy, enteropathia with loss of proteins, malnutrition) 5. pancreatic diseases, ovarial diseases ( Meigs syndrom ). THERAPY: * basic precautions: confinement to bed in hospital, abstinence of alcohol,diet with limited level of natrium ( max. 3 g NaCl daily), reduction of fluids uptake to 1 litre per day, rather vegetarian foods. * diuretics: basic precautions are usually deficient, in therapy are prefered aldosteron antagonists spirolacton 200-400mg/day, daily we meassure : weight, fluids uptake and output, abdominal circumference, we monitor mineral levels in serum and urine (Na, K). If we don´t succeed it is possible to elevate the spirolacton dosis to 800mg and to add furosemid or thiazid diuretic. Reduction of ascites is necessary to perform slowly, diuresis should increase max. 1 litre daily. Decrease of kalium in plasma to the levels round 3 mmol/l and encephalopathia are the reason to interrupt diuretic therapy. Hyponatremia is due to dilution and bodily distribution, prolongated hyponatremia means bad prognosis. *paracentesis ( ascites puncture) in refractery ascites, in tensioned ascites and like the start step in therapy of bulky ascites. During the puncture is necessary to perform prevention for saving of plasmatic volume, the best is albumin infusion, temporary is albumin usually suplemented with Dextran or Haemacel ( 6g / 1 litre of ascites = 100ml 6% solution) * alternative methods are ascites reinfusion, or Le Veen shunt or TIPS (Transjugular Intrahepatic Portosystem Shunt) implantation. PROGNOSTIC AND REVIEW PROBLEMS: Prognosis is serious, patient has to be informed about dietary, regimen and therapeutic precautions and their observance. Prognostic factors are determined also with the basic disease which caused ascites. Based on these datas is given also review problematic and individual access to patients. LITERATURE: Edema in Systemic Rheumatic Diseases.The wiew point of rheumatologist. Doc.MUDr. Marie Valešová,CSc Edema in rheumatic diseases - usually the result of synovial membrane hyperplasia and inflammation (synovitis) which could be followed by inflammation of the other structures of joint (arthritis). - less frequently changes in skin, muscules, tendons, ligaments and their sheets and other so called soft tissues. The presence of swelling or excess of joint fluid is usually nonspecific often reflecting traumatic, inflammatory or infectious etiologies. It can be due to increased levels of physical activity or the result of a preexisting intraarticular lesion. Etiology is unknown Pathogenesis Ethiological agent is unknown - possibilities: a) Infective agent b) Alteration of immune system c) Immunogenetical aspects d) External factors which could led to disorders in nutrition, hormonal regulation, psychical stage etc. or their combinations. Immune mechanisms: Acute or chronic inflammatory reaction of joint synovial membrane due to interaction among: - lymphocytes - macrofages - polymorfonuclelear leucocytes-neutrofils - other cells like fibrocytes, chondrocytes etc. The interaction takes place inside the joint. It is provoced by unknown factor, which comes into this milieu. Immune response to this agent can be divided into four steps: 1.Accumulation of monoclonal cells and presentation of the antigen 2. Proliferation of lymphocytes 3. Local production of antibodies 4. Tissue injury by immune complexes These immune processes led into nonspecific immune response and biochemical reactions. They combine to releasing of degradational enzymes from macrophages, polymorphonuclears, chondrocytes and from the cells of granular tissue, which forms inside the inflammed joint. The substrate for enzymes activity are the macromoleculs of the connective tissue, cartilage and bone proteoglycans and collagen. Pathology Pathological changes in joints: - vasculitis - increased permeability - multiplying of infiltrative T and B lymphocytes, polymorphonuclears and plasmatic cells The stroma of the joint surface is infiltrated by the cells which are multiplicated also inside the joint cavity. The enzymes produced by the synovial and granulation tissue cells paticipate on joint destruction, too. Hydrops of the joint - patological increase of the joint fluid swelling - change of joint shape pain - from joint capsula distention and inflammation They could be 3 types of fluid inside the joint 1) exudate 2) blood 3) pus During the inflammation the character of the fluid could change Typical clinical and laboratory findings There is only a little of joint fluid in a normal joint. The capsula does not curve otwards. It is not possible to demonstrate the fluid by palpation. Only after patological excess of joint fluid production it is possible to distinguish fluctuation. By pressing on one side of the joint increase of tension is felt on the other side of joint capsula. In extraarticular structures like tendons an their sheets, ligaments, enthesis and muscles differentiation of their edema is very difficult and needs some experience or it could be done only by imaging methods. Procedure of examination Clinical The joint has characteristic signs of inflammation 1) Increased temperature on the joint surface 2) Colour is usually unchanged ( erythema- redness could be seen only in arthrtitis of infectious origin or crystal- induced arthritis) 3) Pain in the movement 4) Limitation of joint function Laboratory 1)Analysis of synovial fluid It provides the physician with unique and valuable information about what is going on inside joint. 2)Analysis of serum Acute phase reactants, autoantibodies, circulating immune complexes, and immunochemical tests are evaluated in the assesment of systemic rheumatic illnesses. Imaging techniques and others 1) Conventional radiography, tomography 2) Computed tomography (CT) 3) Magnetic resonance imaging (MRI) 4) Arthroscopy 5) Biopsy (synovial membraine, bone, muscle, skin) Treatment Edema in systemic rheumatic diseases is a result of inflammation of the artricular or extraarticular structures. The aim of present therapy is to decrese joint inflammation, to provide pain relief, and more importantly, to maintain or restore joint function and prevent bone and cartilage destruction. 1) Symptomatic medical therapy - Nonsteroidal antiinflammatory drugs (NSAIDs) - Corticosteroids - Disease - modifying antirheumatic drugs (DMARDs) - antimalarial, sulfasalazine, parenteral gold salts and cytotoxic agents. 2) Physiotherapy 3) Physical therapy - is a part of the treatment program. The goal of exercise is to maintain or improve muscle tone, prevent or correct deformities and maitain or increase joint mobility and function. Prognosis Case reports Literature: Harrison´s Principles of Internal Medicine, Mc Graw Hill, 1995 Souhami,Moxham: Texbook of Medicine, Churchil Livingston ,1994 Kelley et al.: Textbook of Rheumatology, Saunders, Fourth Edition, 1994 Hormonal induced edema and edema due to disorders of nutrition Oedemas due to starvation Nutrition disorders: definition types: marasmus, kwashiorkor, combined disorders adaptation and its metabolic consequences main causes of malnutrition main clinical consequences of malnutrition Oedemas due to starvation: pathogenesis clinical picture Oedemas of endocrine origin Oedema is one part of some endocrine syndromas. Usually it is not dominant symptom. More often oedemas are not visible but hyperhydration is present (increasing of body weight due to extracellular fluid expansion) Oedemas due to hypothyreosis – myxoedema: pathogenesis clinical picture Pathogenesis of water and electrolyte balance disorders due to: Cushing´s disease and Cushing´s syndrome Primary hyperaldosteronism –Conn´s syndrome Pregnancy oedemas Premenstrual oedemas MUDr. J.Jenšovský Hypothyroidism: classical appearance of patients suffering hypothyroidism is caused by periorbital and peripheral oedema. Patients have rough features of the face, oedema of the upper lid, the skin is coarse-grained and thick. There may be some problems in differential diagnosis between oedema of the legs caused by cardiac failure and hypothyroidism. This classical description is quite rare nowadays. Hypothyroidism is diagnosed in subclinical or only mild stages of the disease. Then the skin is only dry and cold, there are no oedemas. The skin is mostly yellowish colour and pale. Patients with hypothyroidism suffer anaemia quite often which contributes to this symptom. The whole- body content of natrium and water is increased, plasma volume on the other hand may be decreased. Patients may develop hyponatraemia, laboratory values of urea and creatinine remain in normal range. Above mentioned characteristic features often result in visceral, pericardial and other effusions. Typically cardiologists have keep in mind diagnosis of hypothyroidism in pericardial effusions of unknown origin. Water retention may cause weight gain but-hypothyroidism is not the cause of obesity. Other hormones which may cause oedema are estrogens. These cause water retention during menstrual cycle and are able to do the same in pharmacological doses/oral contraceptives, hormone replacement therapy etc./. Excessive effusions can be seen in the "overstimulation" syndrome during fertilisation attempts. One of the new causes of hormonally dependent oedemas is treatment with growth hormone. Patients with growth hormone deficit suffer from decreased water content and oedema during treatment is marker of overtreatment. This should not happen in low-dose treatment and during gradually increased doses of growth hormone. References: Wilson J.D. et al: Williams textbook of endocrinology, 9th ede., W.B.Saunders, 1998 Greenspan S.F et al: Basic and clinical endocrinology, 5th ed., Appleton and Lange, 1997 Edema and Starvation 1) Pathophysiology and biochemistry of starvation 2) Malnutrition – marasmus, kwashiorkor a) clinical features of malnutrition - anamnesis, examination. Biochemical and metabolic abnormalities in marasmus and kwashiorkor. b) etiology of malnutrition c) epidemiology of malnutrition d) body composition in undernutrition 3) Case report Literature 1) Diet, nutrition and the prevention of chronic diseases, Report of a WHO Study Group, WHO Technical Report Series, No. 797, WHO, Geneva, 1990, p. 16-21 2) Brown M. L.(edit.): Present Kowledge in Nutrition, 6th Edition, ILSI Press, Washington, 1990, p. 39 46 3) Heepe F.: Diätetische Indikationen, Springer-Verlag, Berlin, 1990, p. 250-251 4) Hamilton E., Whitney E., Sizer F.: Nutrition: Concepts and Controversies, West Publishing Company, St. Paul/New York, 1988, p. 159- 161, 537-567 5) Lener J. et al.: Medical Hygiene, Karolinum, Prague, 1997 6) Barasi M.: Human nutrition – a Health Perspective, Arnold, London, 1997 Edema in pregnancy MUDr.R.Pokorný Edema in a pregnancy is relatively frequent although its incidence is considered to be less important in last few years. It is especially connected with preeclampsia and eclampsia (edema, albuminuria, and hypertension) shortly with diseases connected with pregnancy. A hypertension and an albuminuria in the pregnancy are called preeclampsia. This disease could culminate in eclampsia itself, which is connected with high mortality of a pregnant (10%) and a fetus (30%) as well. It is generally presented that the edema is one of the first signs of the eclampsia. The first stage of edema (perimaleolar) is from orthostatical reasons; the second one (peritibial) requires higher attention especially if it remains after the night rest. The third one (generalized), which is connected with edema of the face, requires particular examination of the pregnant. The edema in connection with hypertension and albuminuria makes the tries of the eclampsia sings. But they also could completely fail in this disease. Pathogenesis of this disease is not known yet. There are a lot of theories for instance multifactorial or prostaglandin one, but no one explains ethiopathogenesis of this disease completely. Incidence of the eclampsia is more frequent in primiparae, especially very young women or vice versa in women older than 30 years of age. Women coming from lower economic status are also of higher risk of having this disease. Disposal factors for this disease are chronical cardiovascular or renal diseases and diabetes mellitus as well. If there is the hypertension before the pregnancy, we call that superimposed preeclampsia or eclampsia. The most significant sign in clinical image of eclampsia is blood pressure with S/D 140/90 and more, proteinuria more than 0.3 g/l in 24 hours, generalized edema with increase of weight more than 1 kg per week. The changes on a retina are although very significant the headache including as well. The symptoms are more frequent before the eclamptic attack. There is a kinetic anxiety, disturbance of sight, emesis, nausea and epigastrium pain. The eclamptic attack itself starts with tonic convulsions chewing and breathing muscles. The woman is in epistotonus and her hands are closet in the fists. This status continues about 20-30 seconds. It passes in the clonic convulsion with clones of facial and limbs muscles with rattling and spume in the mouth. It takes about 1-3 minutes. This status passes in the eclamptic coma – the stage with deep uncousniousness with a hyporeflexy and a dilation of the pupils but with deep and regular breathing. Very common is total amnesia after this attack. The attacks could be repeated (eclampsia status) or there could be unconsciousness without the convulsion status (eclampsy without eclampsy). Laboratory investigation: blood count, biochemical inv. of the kidney – uric acid is higher, urea and creatinin are higher in harder status, biochemical inv. of the liver (SGOT, SGPT, bilirubin is higher), iontogram, the value of protein could be lower. There is a necessity of fetoplacental monitoring (HCG, estriol, ultrasound, ctg.). Complications: Decrease of placental perfusion and chronical placental insufficiency could cause in abruption of the placenta. In severe stages there could be the defect of coagulation of blood, failure of renals, lungs edema and edema of the brain. Differential diagnosis could be epilepsy, hypoglycemia, uremic coma, and tumors of the brain, hysteria. Therapy: The most important is the prevention and timely diagnosis of the first signs of the disease during the prenatal care. In the lighter cases is recommended diet sedative therapy (plegomazine diazepamum), hypotensives (dihydralazin) quiet atmosphe recontinual care about the pregnant, fetoplacental unit, MGS04. In severe stages the sedatives hypotensives MGSO4 and diuretics are recommended, hypertonic solutions, albumin quiet and dark place. If the conservative therapy fails, there is necessary to terminate the pregnancy apart from the fetus. Cesarean section is mostly recommended. Recommended literature: Macků – Porodnictví V. Fuchs – Nemoci v těhotenství G. Martius, M. Beckworld, A. Pfleiderer – Gynekologie a porodnictví Z. Štembera, K. Poláček, V. Vlach – Rizikové těhotenství a dítě B. Vedra – Hypertensní a renální choroby v těhotenství Edema of upper airwais Brain edema Doc.MUDr. Pavel Kalvach,CSc. A) Neurological Aspects of Brain Edema a) Brain edema means an increased hydratation of cerebral tissue. The elevated volume of water is situated either inside of the cells - as in intracellular edema, or in the intersticium - as in extracellular edema. The etiology of both these types of brain edema is different. Intracellular edema arises from cytotoxic or ischemic or traumatic causes. In a failure of the Natrium - Kalium pump on the cellular membrane Natrium enters into the cells and Kalium escapes out of the cells. Na - due to its higher solvatation pulls water inside, the cell swells and the tissue augments its volume. The expanding effect of the damaged tissue is prone to compress the surrounding tissue and to spoil its perfusion gradients. This type of edema is immobile, bound locally to the cellular cytoplasm. On a cut through the tissue the water doesn´t flow out and consequently this edema has been earlier designated as a "dry" edema. Extracellular edema appears from vasogenic reasons. This means an abnormally loosened blood-brain-barrier (BBB). The plasmatic filtration crosses the BBB, in contradistinction to the intracellular edema, where a plasmatic ultrafiltration is being moved into the cells. The extracellular, intersticial edema is mobile and does not cause an expansion of the lesion. Due to its mobility it spreads according to the hydraulic laws in a direction of the least resistance. Therefore it dwells preferentially in the white brain matter. On a tissue cut it flows out and so it deserved a designation "wet" edema. Its specific form is the periventricular intersticial edema, arising in the tight neighbourhood of cerebral ventriculs in obstructive hydrocephalus. b) The augmented brain volume due to edema is a dangerous state in the closed intracranial (i.c.) space. In smaller lesions the compression of capillary perfusion affects the immediate surroundings, in bigger lesions it puts in danger even distant parts of the brain. The increasing brain hemisphere pushes the midline to the other side and exerts pressure on contralateral structures against narrows of the i.c. space. This is important mainly in the tentorial incissure and in the great occipital foramen. The clinical signs therefore are due to local damage as well as to general i.c. hypertension. The focal signs are combined in more severe stages with conus signs. c) The particular local lesion in intracellular edema is caused by the original etiology (most often ischemic malacia in perfusion failure) in the extracellular edema by the damaged blood-brain-barrier (in tumors, abscesses, metastases or in later stages of ischemic infarction). d) The local edema should be understood as a consequence of the primary pathology in the centre. It is substantial to distinguish the initial stages of intacranial hypertension and conus signs: headache with vomiting, meningeal syndrom, a developing peduncular mesencephalic lesion and signs of a compressed oblongata with a severe brain stem syndrom. The asymetry of pupills with signs of a rostro-caudal deterioration of the brain stem are leading symptoms in our examination. e) The therapy of a cytotoxic/ischemic edema is based on the treatment of the primary etiology. Most often then on attempts to improve brain circulation (anticoagulation, thrombolysis, improvement of blood viscosity, securing of cardiovascular efectivity). The extracellular edema is usually treated by corticosteroids. In urgent conus stages the most important step is a restauration of CSF (cerebral spinal fluid) pathways in cases of obstructed CSF straits: a surgical shunting - usually from the lateral ventricle. f) The preservation of vital functions in intensive care units (ICU) can save life in many patients with edema. The critical period may often be only 7 till 10 days. The healing of the original - particularly traumatic or cerebrovascular affection - often brings, after surpassing of the acute stage, a dramatic improvement. B) Neurogenic edema in somatic tissues A tissue edema in afflictions of peripheral nerves is rare. Sometimes chronic edema complicates a reflex sympathetic dystrophy, usually in its severe stages. The pathogenetic mechanism of its rise in this disease is unknown. Another rare phenomenon is a neurogenic lung edema. The pathogenetic principle is a sudden elevation of intracranial pressure, for instance in i.c. bleeding. This elicites an increase of systemic pressure. The accute elevation of peripheral resistance, trying to compensate cerebral perfusion, may lead to a left-sided heart faillure with a consequent lung edema. Literature: Raymond D.Adams, Maurice Victor: Principles of nerology, New York, St. Louis, San Francisko, McGrawHill,1977, 1286 pgs. Anne G Osborn: Diagnostic Neroradiology, St. Louis, Baltimore, Boston, Mosby, 1994 Edema in burns MUDr. Monika Valová A) Pathogenesis : 1. Disorder of volume homeostasis ( disorder in Starling ´s homeostasis ) : a) vasodilatation precapillary b) increase of interstitial osmotic pressure c) obstruction of veins distal d) increase of microvascular permeability for macromolecules ( collapse of microcirculation ) e) damage of endothelium by thermal noxa f) decrease of oncotic plasma pressure , loosening of the interstitial matrix, hypoproteinemia g) disorder of cell membrane by decrease of general membrane potential a) b) c) d) e) f) 2. The hormonal and humoral aspects : activation of the sympathoadrenal and hypothalamic-pituitary-adrenal axis, shock mediators the renin – angiotensin –aldosterone system ADH kallikrein – kinin system clotting and fibrinolytic cascade complement system arachidonic acid cascade B) Sorts of the edemas : 1. Local : a) collateral edema in burns, specific form of edema in electrical burns b) visceral forms of local edemas – cardial and non-cardial edema of lungs, edema of brain, hydrops ( hydrothorax, hydropericardium, ascites ) c) the other forms of edemas – for example blockade of venous outlet, lymphedema, inflammatory edema, allergic, static edema , edema like complication of internal diseases, iatrogenic edemas 2. General : a) interstitial and intracellular edema b) general forms of edemas in visceral involvement ( cardial, renal, hepatic ) c) iatrogenic general edemas of extracellular space – overexpansion C) Diagnostics : 1. Physical investigation 2. Laboratory investigation 3. Monitoring of the basic vital functions ( total, visceral circulation, plasma volume ) 4. visualizing methods ( US, Doppler, echocg ,rtg, CT, DSA, phlebographia, lymphographia) D) Therapy : goal : restore and maintain perfusion of tissues, first in the level of microcirculation , prevent from the tissue ischemia , prevent from the development of multiple organ dysfunction and failure 1. Principles of replacement fluid therapy in burns 2. Monitoring of total, visceral circulation, plasma volume 3. Therapy of hypovolemic shock : a) sorts of resuscitation solutions b) sorts of resuscitation diagrams according to extent, weight, age, body surface c) complication of therapy ( local, total, visceral ) C) Prognosis : according to weightiness of burns : 1. mechanism of thermic injury 2. extent and depth 3. age of patient 4. localization 5. anamnesis – personal, family, work D) Verdict standards : 1. forms of injuries ( work, out – of work ) 2. mechanism of injury 3. extent, depth, localization of injury 4. age of patient 5. permanent consequences 6. anamnesis 7. criminal acts E) Case Studies Literature : Rozsáhlé popáleninové trauma, Avicenum , the second printing ,1990, Prof. MUDr. Radana Konigová, spol. Total Burn Care, D. N. Herndon, W. B. Saunders Comp., 1996, the second printing Burns management , John A. D. Settle, Churchill Livingstone, 1996, the first printing Edema – allergy or idiosyncrasy MUDr. P.Kučera Pathogenesis Angioedema (angioneurotic edema, edema Quincke) is caused by edema of deep dermis and subcutaneous tissue. An area involved with angioedema has swelling as the prominent manifestation, the appearance of skin can be normal or can occur together with urticaria, erythema. It lasts about 24 to 72 hours. The pathogenesis and trigger factors of allergic edema are very heterogeneous. The basic mechanism is the basophil and tissue mastocyte activation and releasing of vasoactive mediators. Histamine, tryptase and chymase are the most important one, causing the early symptoms of edema. Later released mediators, like cytokines, arachidonic acid metabolites amplify allergic reaction. Mastocyte activation is caused by bridging of two high affinity receptors for IgE (FcRI) or by nonimmunologic pathway, stimulation by morphine, codeine, substance P. Sometimes, the exact mechanism is unknown. Decreased concentration or low function of C 1 inactivator is a pathway of hereditary angioedema ( HAE). This swelling is based on increased vascular permeability caused by kinin-like mediators, activated proteins from complement cascade. Symptoms and laboratory findings. Angioedematous swelling often involves the face (eyelids or cheeks), tongue, extremities or genitalia. They are asymmetrically distributed and transient, angioedema and urticaria can occur together. In deeper skin layers are fewer mast cells and sensory nerve endings, the lesions have little pruritus and swelling may be painful or burning. Hereditary angioedema is not associated with urticaria, skin lesions, visceral involvement (laryngeal edema, gastrointestinal wall edema) are typical. Abdominal attacks last usually 3-4 days, they can be inherited or acquired. Diagnosis, differential diagnosis Diagnosis is based on clinical symptoms. Investigations Etiopathogenetic diagnosis is based on the data from past history, the past history can bring information about impact of allergens or nonimmunological triggers. We can test the type I hypersensitivity by allergen skin tests, measuring of specific IgE in serum. Typical finding for hereditary angioedema is quantitative of functional drop of C I inactivator, C2 or C4 parts of complement. Treatment, aspects depending on locality and etiology Therapy of acute attacks consists of antihistamines, adrenaline, corticosteroids. In the case of HAE we use steroids, sometimes adrenaline, preferentially C I inactivator concentrate, preventive treatment consists of anabolic steroids. Treatment has to be aggressive in the cases of edema with high risk – airway or gastrointestinal obstruction. Approach to the patients There is usually no problem to setup the diagnosis, but part of patient with angioedema doesn’t respond to therapy, patients are usually able to work. Cases will be demonstrated during tutorials References: Stites DP, Terr AI,: Základní a klinická imunologie, Victoria Publishing a.s. Praha, 1994 Fucíková T: Klinická imunologie v praxi, Galén 1993, 1995 Kay AB: Allergy and Allergic Diseases, Blackwell 1997 Literature : B.G. Katzung : Basic and Clinical Pharmacology 7th edition, Prentice-Hall International , 1998 Rang, Dale, Ritter : Pharmacology 3rd edition, Churchill Livingstone, Edinburgh, 1995 Mycek, Harvey, Champ : Lippincott´s Illustrated rewiews Pharmacology 2nd edition, Lippincott-Raven, Philadelphia, 1997