SOAP note - Nicole Elizabeth Kosmala
advertisement
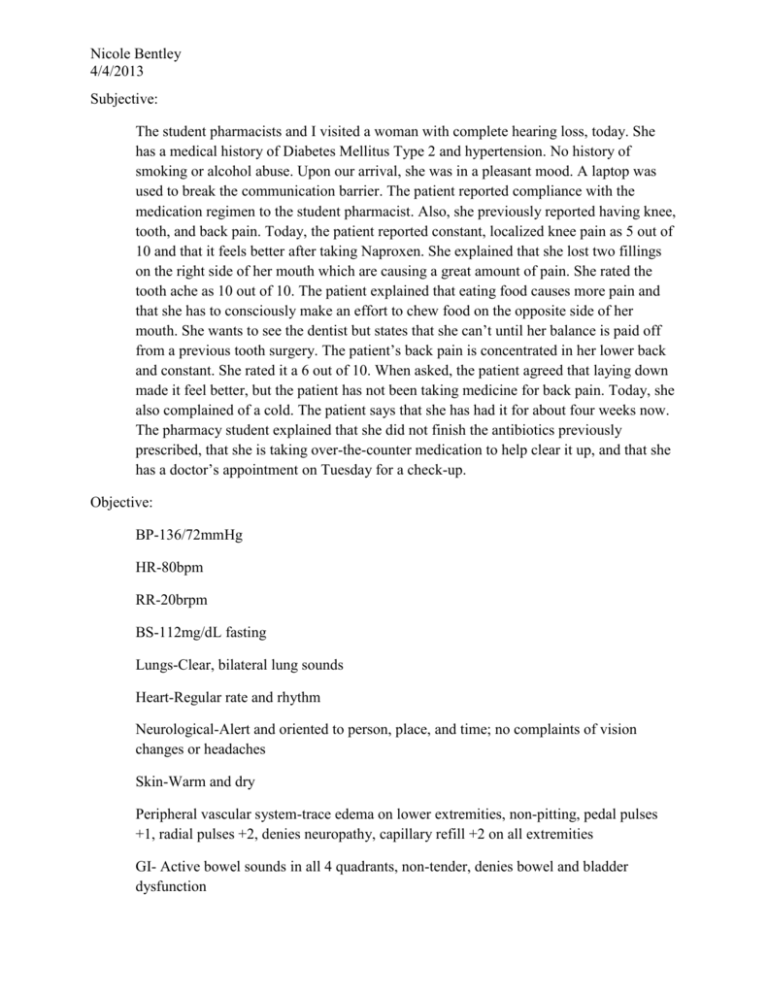
Nicole Bentley 4/4/2013 Subjective: The student pharmacists and I visited a woman with complete hearing loss, today. She has a medical history of Diabetes Mellitus Type 2 and hypertension. No history of smoking or alcohol abuse. Upon our arrival, she was in a pleasant mood. A laptop was used to break the communication barrier. The patient reported compliance with the medication regimen to the student pharmacist. Also, she previously reported having knee, tooth, and back pain. Today, the patient reported constant, localized knee pain as 5 out of 10 and that it feels better after taking Naproxen. She explained that she lost two fillings on the right side of her mouth which are causing a great amount of pain. She rated the tooth ache as 10 out of 10. The patient explained that eating food causes more pain and that she has to consciously make an effort to chew food on the opposite side of her mouth. She wants to see the dentist but states that she can’t until her balance is paid off from a previous tooth surgery. The patient’s back pain is concentrated in her lower back and constant. She rated it a 6 out of 10. When asked, the patient agreed that laying down made it feel better, but the patient has not been taking medicine for back pain. Today, she also complained of a cold. The patient says that she has had it for about four weeks now. The pharmacy student explained that she did not finish the antibiotics previously prescribed, that she is taking over-the-counter medication to help clear it up, and that she has a doctor’s appointment on Tuesday for a check-up. Objective: BP-136/72mmHg HR-80bpm RR-20brpm BS-112mg/dL fasting Lungs-Clear, bilateral lung sounds Heart-Regular rate and rhythm Neurological-Alert and oriented to person, place, and time; no complaints of vision changes or headaches Skin-Warm and dry Peripheral vascular system-trace edema on lower extremities, non-pitting, pedal pulses +1, radial pulses +2, denies neuropathy, capillary refill +2 on all extremities GI- Active bowel sounds in all 4 quadrants, non-tender, denies bowel and bladder dysfunction Nicole Bentley 4/4/2013 Mobility-requires no assistance with ADLs Assessment: Her DM Type 2 seems to be controlled at this time due to her FBG<130. 1. Risk for decreased cardiac output: She is compliant with her medication regimen, but her blood pressure has been slightly elevated at the past couple of visits. The patient’s goal blood pressure is <130/80. Her systolic blood pressure was higher than goal, but overall the medication is managing her hypertension 2. Acute Pain: She reported a high pain scale rating for her tooth ache and moderate pain scale ratings for her knee and back pain. 3. Excess Fluid Volume: She has trace edema, non-pitting, in her lower extremities. Plan: DM-Encouraged her to continue with the medication regimen and diet to keep DM Type 2 under control. HTN-Counseled to be aware of the following changes related to hypertension: edema, headaches, visual disturbances, dizziness, and shortness of breath. Pain-Encouraged to continue to take Naproxen for pain and to tell someone if it gets worse. Continue to monitor pain levels for improvement at upcoming visits. Continue to monitor knees for fluid pockets that cause the patient pain. In future visits, the patient should be encouraged to try Orajel to alleviate some tooth pain. A heating pad, cold compress, or IcyHot could be suggested to alleviate back pain, as well. Further evaluation on whether or not these are viable options for the patient’s socioeconomic status should be assessed. Edema-Encouraged her to exercise more throughout the day to help resolve edema in her lower extremities. Encouraged to prop her feet up when sitting to help resolve this matter, as well. Education: Uncontrolled hypertension- signs and symptoms that need to be reported: edema, headaches, visual disturbances, dizziness, and shortness of breath. Edema-exercise and elevation of legs when sitting or laying