Baseline Obstetric Visit
advertisement

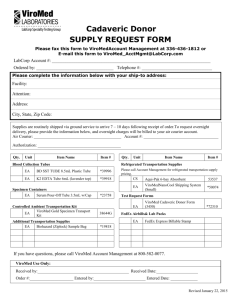
CHAPTER 4 BASELINE OBSTETRIC VISIT 4.1. Purpose The purpose of the Baseline Obstetric visit is to collect data on participant medical and obstetric history and medication use, and to collect OB examination data and specimens. 4.2. Timing / Scheduling of the Baseline OB Visit The Baseline Obstetric data collection occurs after a participant’s study eligibility has been confirmed, study consent has been obtained and the participant has been enrolled. The visit can also occur in part or in whole immediately following recruitment and enrollment. For example, demographic and medical history forms, and maternal blood serum can be completed immediately after enrollment (during the same clinic visit) even if another participant appointment is needed to complete the OB Baseline data collection. If an additional clinic visit is required to complete the baseline data collection, the visit should be scheduled as soon as possible after eligibility is determined. Both the Obstetric and Periodontal baseline visits must be completed before participant randomization, with no specified order required. All baseline visits are documented on data collection forms as visit = 02. Randomization can occur at the same clinic visit as the Baseline OB and Periodontal visits, after data collection procedures are completed. Randomization and all treatment visits must be completed prior to 236 weeks gestational age. Randomization should occur after baseline visits have been completed and a conclusive fetal anomaly ultrasound has been performed to confirm the inclusion/exclusion criteria. For institutions that use ultrasounds prior to 16 weeks gestation to confirm inclusion criteria, this ultrasound is sufficient for randomization. 4.3. Staffing Staff involved with collection of MOTOR data and specimens must have completed appropriate training and certification procedures (see Chapter 2). 4.4. Sequence of Procedures and Forms The following procedures and data collection forms are required at the baseline OB visit: Baseline Demographic Form (BDF) Baseline Obstetric Form (BOF) Maternal Blood Collection Form (MBF) CHAPTER 4: Obstetric Baseline Visit 9/13/06 Page 4 - 1 Baseline OB Specimen Collection Form (BSF) Maternal Serum Sample Collection o Specimen Collection Packet #1 Speculum Examination with Specimen Collection o Specimen Collection Packet #3 o Fetal Fibronectin Collection o Vaginal pH Collection o Gram Stain slide Collection o Vaginal Paperpoint Samples Note: Specimens are to be collected only on participants who have given consent for collection. Note: See Appendix 3 for instructions on specimen shipping, and the Specimen Shipping and Tracking Log (SSL). Baseline Demographic Form ID: ___ ___ ___ ___ ___ ___ ___ ___ Form: BDF Ver: A Visit #: 02 Name: _________________________ Staff ID: __ __ __ Date: __ __ / __ __ / 20__ __ Seq #: 01 Instructions: This form is to be completed for each participant after enrollment at the Baseline OB Visit. Information is obtained through participant interview. 1. Participant date of birth __ __ / __ __ / 19 __ __ 2. Are you of Hispanic origin (ethnicity)? (circle one) 1 = Yes 2 = No 3 = Don’t know / Refused 3. Which of the following best describes your race? (check all that apply) a. White b. Black or African-American c. Asian or Pacific Islander d. Aleut, Eskimo, or American Indian e. Other ______________ f. Don’t know / Refused 4. How many years have you lived in the United States? (circle one) 1 = Born in the U.S. 2 = Less than 3 years 3 = 3+ years (but not born here) 4 = Don’t know / Refused 5. How would you describe your current marital status? (circle one) 1 = Single 2 = Widowed 3 = Married / Partner 4 = Divorced 5 = Separated 6 = Don’t know / Refused 7. What is your current occupation? (circle one) 1 = Employed - full-time 2 = Employed - part-time 3 = Self-employed 4 = Homemaker 5 = Retired 6 = Disabled 7 = Unemployed 8 = Refused to answer 8. What is your current household income? (circle one) 1 = < $10,000 2 = $10,000 – 19,999 3 = $20,000 – 39,999 4 = $40,000 – 59,999 5 = ≥ $60,000 6 = Don’t know / Refused 9. What medical insurance do you currently have? (circle one) 1 = Private insurance 2 = Medicaid 3 = No insurance 4 = Don’t know / Refused 10. Are you currently receiving public assistance? (include WIC or Food Stamps) (circle one) 1 = Yes 2 = No 3 = Don’t know / Refused 6. What is your educational level (or total years of education completed)? (circle one) 1 = None 2 = Elementary (1-6 years) 3 = Junior high (7-8) 4 = High school (9-12) 5 = College (13-16) 6 = Graduate (17+) 7 = Don’t know / Refused 4.4.1. Baseline Demographic Form (BDF) The Baseline Demographic Form (BDF) is to be completed by study staff after enrollment, as part of the Baseline Obstetric visit. Data collection is done through participant interview. Refer to the BDF QXQ’s for specific instruction on completing this data collection form. Baseline Obstetric Data Form 4.4.2. Baseline Obstetric Form (BOF) The Baseline Obstetric Form (BOF) is to be completed by study staff after enrollment during the Baseline OB visit. The BOF form focuses on the physical exam, past pregnancy history, and smoking, alcohol, and drug use histories. Data collection involves abstraction from the clinical site’s medical records and participant interview. Refer to the BOF QXQ’s for specific instruction on completing this data collection form. ID: ___ ___ ___ ___ ___ ___ ___ ___ Form: BOF Ver: A Visit #: 02 Name: _________________________ Staff ID: __ __ __ Date: __ __ / __ __ / 20__ __ Seq #: 01 Instructions: Complete this form for all participants at the OB baseline visit. Information should be obtained from medical record; if unavailable, information should be supplemented by participant interview. Responses that are unknown or refused are coded ‘U’. PHYSICAL EXAM 1. Pre-pregnancy Weight (in kg or lb) __ __ .__ kg __ __ __ .__ lb 2. Weight measured today (in kg or lb) __ __ .__ kg __ __ __ .__ lb 3. Height measured today (in cm or in) __ __ __ .__ cm __ __ .__ in OB / Pregnancy HISTORY 4. Uterine anomaly 5. Previous pregnancies If YES, record the number of: a) ____ Full-term births Y N U Y N U ____ ____ ____ Pre-term births (<37) Abortions Live births 6. Cervix ever been treated? 2. GA: __ __ Wt: __ __ lbs __ __ oz Type of delivery reported : ___ 7. Infertility treatment for this pregnancy? U Y N U 8. Did you smoke cigarettes before you Y found you were pregnant? N U 9. Have you smoked cigarettes at any Y N U time during this pregnancy? If YES, average # cigs/day in last week __ __ 10. Have you had alcoholic drinks at any Y time during this pregnancy? If YES, average # drinks/ week N U __ __ (enter 0 if less than 1/week) 11. Have you used “street drugs” at any time during this pregnancy? If YES, Cocaine or Crack? 3. GA: __ __ Wt: __ __ lbs __ __ oz Type of delivery reported : ___ Delivery Codes: 1 = Spontaneous labor / PROM 2 = Maternal indication 3 = Fetal indication 4 = Unknown 9/13/06 N (enter 0 if less than 1/day) b) If Pre-term births>0, record GA, birth weight, and delivery classification code, for each delivery 20-36 weeks. If more than 3, record “worst” pregnancy histories. 1. GA: __ __ Wt: __ __ lbs __ __ oz Type of delivery reported : ___ CHAPTER 4: Obstetric Baseline Visit Y If YES, how? (check all that apply) a. LEEP b. Laser c. Cryo d. Cone biopsy e. Other, specify ________________ Page 4 - 2 Y N U Y N U 4.4.3. Baseline Blood Collection Peripheral blood will be collected from each participant for Buffy coat, plasma, and serum samples. Blood is collected by venipuncture of the antecubital area. A CPT Vacutainer and SST Vacutainer for the blood draws are to be supplied by the sites. All pre-labeled secondary tubes are contained in the collection packets supplied by UNC. Section 4.5 details the procedures for serum and buffy coat drawing, processing, and storage. Storage and shipping instructions are found in Appendix 3. 4.4.3.1. Baseline Blood Collection Packet #1 Motor Specimen Collection Packet #1 contains 2 yellow caped tubes (ending in ‘501’ and’502’) for buffy coat for eventual DNA analysis, a blue caped tube (‘601’) for plasma from the CPT, and 4 red caped serum tubes (‘301 – 304’) for cytokines and cotinine analysis. In addition, extra pre-coded labels ending with ‘000’ are included for use in processing (such as centrifuge tubes) and for the ‘paperwork’ label to be affixed onto the Maternal Blood Collection Form (MBF), see 4.4.3.2. It is important that collection packet #1 supplied with pre-labeled vials is prepared and readied at the beginning of the participants OB visit so that the study samples can be collected at the time of other routine laboratory studies occurring during the participants OB visit. If it is not possible to have obtained the samples at that time, an additional needle stick may be required to collect this sample. 4.4.3.2. Maternal Blood Collection Form (MBF) The Maternal Blood Collection Form (MBF) is used to document the collection of (or inability to collect) the baseline maternal blood specimens, and to provide the linkage of the participant ID number to the specimens that are shipped to the lab. When a specimen is collected, it is noted on the form with the date and time of collection. The extra label (ending in ‘000) from packet #1 to be affixed to the form in the place indicated. Refer to the MBF QXQ’s for specific instruction on completing this data collection form. Note: Baseline visits are recorded on the form as visit=02. Maternal Blood Collection Form ID: ___ ___ ___ ___ ___ ___ ___ ___ Form: MBF Ver: A Visit #: __ __ Seq #: __ __ Name: _________________________ Staff ID: __ __ __ Date: __ __ / __ __ / 20__ __ Instructions: This form is completed when either a baseline or postpartum maternal blood specimen is collected. Code MBF as Visit 02 for baseline and as Visit 04 for postpartum. Attach the corresponding extra label from the specimen collection packet in the box below. 1. Maternal blood sample collected Y N If NO, explain ___________________________________________________________________ ___________________________________________________________________ 2. Date maternal blood sample collected __ __ / __ __ / 20 __ __ 3. Time of maternal blood sample collection (Record in military time) __ __ : __ __ 4. Place extra label from the OB Blood Collection Packet #1 (prenatal) or #4 (post-partum) in the box below. Enter specimen ID number into MOTOR DMS. Label from collection packet #1 (prenatal) or #4 (post-partum) here 5. Comments Y N ______________________________________________________________________________________ ______________________________________________________________________________________ 4.4.4. Speculum Examination ______________________________________________________________________________________ ______________________________________________________________________________________ At the baseline OB visit, a speculum exam will be performed to collect vaginal and cervical samples for microbiological determination. Specimens include fetal fibronectin, vaginal pH, and gram stain slides, and specimens for microbial DNA. CHAPTER 4: Obstetric Baseline Visit 9/13/06 Page 4 - 3 The pelvic exam to collect fetal fibronectin must be conducted prior to performing any other cervical/vaginal exam. A clean (not sterile) speculum, unlubricated or lubricated with water, will be placed in the vagina. Before obtaining vaginal specimens, visualize the cervical os. If the cervical os appears dilated more than 2 cm, or if the amniotic membranes can be seen in or through the cervical os, the participant must be excluded from participation in the study at this time. Dacron swabs must be used to collect fetal fibronectin samples, either Dacron or cotton swabs may be used for vaginal pH or for the gram stain slides. If any other routines, such as a Pap smear or cervical cultures are planned during this exam, the swabs for fetal fibronectin samples and Gram stain must be obtained first in order to minimize blood contamination. 4.4.4.1. Baseline Obstetric Specimen Collection Packet #3 MOTOR Specimen Collection Packet #3 contains the pre-coded labels and/or tubes required for the Baseline OB specimen collection (see Appendix 3) . Slides for gram stain are to be provided by each site. Fetal Fibronectin uses a special kit. The DNA tubes require that sterile TE buffer (also provided by UNC) be added to them before specimen collection, paperpoints for specimen collection are included in the packet. The collection packet also contains an additional ‘paperwork’ label ending in “000”, this label is to be affixed to the Baseline Specimen Collection Form (BSF), item #5, to link the OB specimens to the participant ID. 4.4.4.2. Baseline Obstetric Sample Collection Form (BSF) The Baseline Obstetric Sample Collection Form (BSF) is used to document the collection of (or inability to collect) the baseline OB specimens (described below), and to provide the linkage of the participant ID number to the specimens that are shipped to the lab. The extra label (ending in ‘000) from packet #3 is placed on the form to identify the OB specimens at question # 6. Data entry of the specimen ID number from the labels provides the link to the participant ID. Baseline Obstetric Specimen Collection Form ID: ___ ___ ___ ___ ___ ___ ___ ___ Form: BSF Ver: A Visit #: 02 Name: _________________________ Staff ID: __ __ __ Date: __ __ / __ __ / 20__ __ Instructions: This form is completed at baseline data collection. Indicate all OB specimens collected and attach the extra label from the specimen collection packet in the box provided. 1. Date baseline OB specimens collected __ __ / __ __ / 20 __ __ 2. Time of baseline OB specimen collection (record in military time) __ __ : __ __ 3. Cervicovaginal FFN samples collected? Y N 4. Gram stain smears collected? Y N 5. Paper point samples collected? Y N 6. Place extra label from Baseline OB Specimen Collection Packet # 3 (FFN + gram smear) in the box below. Enter specimen ID number into MOTOR DMS. Refer to the BSF QXQ’s for specific instruction on completing this data collection form. Label from collection packet #3 here 7. Vaginal pH? a. Result: 4.4.4.3. Fetal Fibronectin Collection 8. Comments Y N Y N ___ . ____ ______________________________________________________________________________________ Fetal fibronectin specimen collection kits will be supplied from Adeza Biomedical, CHAPTER 4: Obstetric Baseline Visit Seq #: __ __ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ 9/13/06 Page 4 - 4 these kits will be sent to the sites from UNC Dental. Motor collection kit #3 contains the label, ending in “803”, for use in labeling the specimen tube. The package insert Precautions and Warnings section should be carefully read and understood by the person collecting the specimens. The collection kit contains two sterile Dacron swabs for every clear or white capped vial containing extraction buffer for the preservation of the fetal fibronectin. Avoid storing near equipment that may intermittently generate heat (i.e., refrigerator, incubator, office machines) or near windows that may expose the kits to the sun. Using 1 swab, samples are to be collected first from the cervix and then the posterior fornix. Do not use cotton swabs in place of the Dacron swabs provided in the kits. Collect two FFN specimens per participant. Insert swabs from the kit and gently rotate the swabs around the external cervical os to saturate the swab with secretions (approximately 15 seconds). When using the swabs, do not “dig” or abrade the tissue surface, as one might do when collecting a specimen for chlamydia determination. Avoid the collection of obvious mucous aggregates. Gentle sampling will minimize collection of samples having needless excessive cellular debris which is not required for assay performance. Do not insert the swabs into the cervical canal. After collecting the cervical specimens, gently rotate the swabs across the posterior fornix for approximately 15 seconds until they are saturated. When completed, remove the swabs carefully to avoid contamination. Two swabs may be collected simultaneously. If so, be sure that both Dacron swabs are fully saturated with cervicovaginal secretions. Immerse the Dacron tips of both swabs in the buffer contained in the collection tube, and break the shafts of the swabs at the score marks so that the tube can be recapped containing the swabs and specimens. The shaft will then be aligned with the hole inside the tube cap and pushed down lightly while securing the cap. It is important to align the shaft to prevent leakage. Discard the broken shaft ends, make sure the tube is labeled with the barcode label provided in MOTOR packet #3 that ends in “803”. The sample tube may be stored refrigerated (2-8°C ) for up to 8 hours, and as soon as possible, should be transferred to storage at -70°C or below. Refer to Appendix 3 for storage and shipping instructions. The OB specimen collection packet contains per-labeled bar-coded vials for the swabs. Collection of the specimen is to be documented onto a Baseline OB Specimen Collection Form (BSF), and a label from the packet attached where indicated. 4.4.4.4. Vaginal pH Using a dry dacron or cotton swab with plastic shaft, take a vaginal secretion specimen from the upper third of the vaginal sidewalls. Touch the swab to the reagent block on the ColorpHast indicator strip. The pH must be read after the color has stopped changing, but before the paper dries completely. Only ColorpHast strips which have CHAPTER 4: Obstetric Baseline Visit 9/13/06 Page 4 - 5 been stored away from light should be used to obtain vaginal pH. If the color falls between two values on the chart, round up. DO NOT interpolate between values. Record the results of the vaginal pH as indicated by the indicator strips on the Baseline Obstetrics Sample Collection Form (BSF) in the space provided. 4.4.4.5. Collection for Vaginal Gram Stain Two gram stain slides are to be prepared after measuring the vaginal pH. The MOTOR OB Specimen Collection Packet #3 contains labels for 2 slides ending in “701” and “702”, the site provides the slides. Vaginal secretions are to be taken from the upper vaginal fornix (label/slide #”701”) and from the cervical os (label/slide #”702”). It is important that the slides be labeled correctly in order to identify the specimen location. Secretions are taken using a dry cotton swab. The swab should be gently rolled across the entire glass slide from end to end, avoiding blobbing and in a thin layer. Use a second dry swab to take the 2nd specimen, using the same procedure. Allow to air dry. Slides are stored at room temperature in a slide box for future analysis. Collection of the specimen is to be documented onto the BSF. Refer to Appendix 3 for Storage and Shipping Instructions. 4.4.4.6. Vaginal Paperpoint Samples for Microbial DNA Prior to the obstetrical visit and specimen collection, tubes “801” and “802” should each have 100 ul of sterile TE (Tris-EDTA, provided by UNC) buffer added to them. Break the package of 5 attached paper points (found in MOTOR packet #3) open being careful not to touch the paper points. Attach 2 paperpoints to the sterile ring forceps by opening the ring forceps and closing over the larger end of the paperpoints. The first sample is taken from the posterior vaginal fornix by gently swabbing the paperpoints against the soft tissue thereby saturating the paperpoint ends with fluid. The paperpoints are then placed directly into the vial labeled with a barcode ending in “801” which should have an orange cap. Then a second sterile ring forcep is used to attach the other 2 paperpoints to the ring forcep and the second sample is taken from the cervical os by gently swabbing the paper point. These paperpoints are then placed directly into the vial labeled “802” with a green cap. Once both samples have been obtained, 100 ul of NaOH is added to each vial, the vials tightly recapped, and the samples vortexed to achieve thorough mixing of the buffer and NaOH. Sample vials can be placed on dry ice at that time, and as soon as possible should be stored at or below -70°C until shipment to the central lab at UNC. Refer to Appendix 3 for Storage and Shipping Instructions. CHAPTER 4: Obstetric Baseline Visit 9/13/06 Page 4 - 6 4.5. Baseline Maternal Blood Sample 4.5.1 Preparation of Buffy Coat and Plasma from CPT Collection Tube Whole Blood Specimen 4.5.1.1. Test Summary and Principle The Vacutainer™ CPT™ Cell Preparation Tube with Sodium Citrate combines a blood collection tube containing a citrate anticoagulant with a Ficoll Hypaque density fluid and a polyester gel barrier which separates the two liquids. The result is a convenient, single Tube system for the collection of whole blood and the separation of mononuclear cells. The Vacutainer™ CPT™ Cell Preparation Tube with Sodium Citrate reduces the risk of sample contamination and eliminates the need for additional tubes, pipettes, and reagents. Samples can be transported without removing them from the Tube. The blood separation media takes advantage of the relatively low density of mononuclear cells to isolate them from whole blood. The separation occurs during centrifugation when the gel portion of the medium moves to form a barrier separating the mononuclear cells and plasma from the denser blood components. The mononuclear cells can be collected by pipetting the cell layer, or the cells can be resuspended into the plasma by gentle inversion to improve cell viability if the sample is to be transported. 4.5.1.2. Needed Reagents and Supplies BD Vacutainer tube, cat.# 362760 Pasteur Pipettes Centrifuge with Swinging Bucket Rotor and Tube Carriers/Adapters for 13 x 100 mm and/or 16 x 125 mm tube size. NOTE: Centrifuge must be capable of generating at least 1500 RCF at the tube bottom. CHAPTER 4: Obstetric Baseline Visit 9/13/06 Page 4 - 7 4.5.1.3. CPT™Procedure 1. The Vacutainer™ CPT™ Tube with Sodium Citrate should be at room temperature (18-25° C) and properly labeled for patient identification. 2. Collect blood into the Tube using the standard technique for Vacutainer™ Brand Blood Collection Tubes . 3. After collection, store Tube upright at room temperature until centrifugation. Blood samples should be centrifuged within two hours of blood collection for best results. 4. Centrifuge Tube/blood sample at room temperature (18-25° C) in a horizontal rotor (swing-out head) for a minimum of 20 minutes at 1500 to 1800 RCF (Relative Centrifugal Force). 5. NOTE: Remix the blood sample immediately prior to centrifugation by gently inverting the Tube 8 to 10 times. Also, check to see that the Tube is in the proper centrifuge carrier/adapter. 6. WARNING: Excessive centrifuge speed (over 2000 RCF) may cause tube breakage and exposure to blood and possible injury. To calculate the correct centrifuge speed in RPM for a given Relative Centrifugal Force, go to the Becton Dickinson Web site at the following address: www.bd.com/vacutainer/products/molecular/citrate/procedure.asp At the bottom of the page, enter two of the three values (e.g., radius if centrifuge in cm = 10; RCF = 1600; press the Calculate button and the correct RPM to set your centrifuge on will be displayed. 7. After centrifugation, mononuclear cells and platelets will be in a whitish layer just under the plasma layer (see above figure). Aspirate approximately half of the plasma without disturbing the cell layer. Transfer at least 1.0 ml of this plasma into the Blue-capped storage tube with barcode number ending in “601” from MOTOR packet #1. Collect cell layer with a Pasteur pipette and transfer about half to each of tubes 501 and 502. All 3 tubes (601, 501, 502) can be kept CHAPTER 4: Obstetric Baseline Visit 9/13/06 Page 4 - 8 on dry ice until they can be transferred to storage at -80C or below. The cell washing procedure on the BD package insert does not have to be preformed at the local motor sites. 4.5.1.4. 1. Test Limitations Volume of Blood The exact quantity of blood drawn will vary with the altitude, ambient temperature, barometric pressure, and venous pressure. The minimum volume of whole blood that can be processed without significantly affecting the recovery of mononuclear cells is approximately 3.0 mL for 4 mL draw. 2. Temperature Since the principle of separation depends on a gel movement, and the viscosity of the gel varies with temperature, the temperature of the system should be controlled between 18-25° C during centrifugation. 3. Centrifugation Since the principle of separation depends on the movement of formed elements in the blood through the separation medium, the RCF should be controlled at 1500 RCF to 1800 RCF. The time of centrifugation should be a minimum of 20 minutes. (As noted in the troubleshooting section, some specimens may require up to 30 minutes for optimal separation.) Centrifugation of the Vacutainer™ CPT™ Tube up to 30 minutes has the effect of reducing red blood cell contamination of the mononuclear cell fraction. Centrifugation beyond 30 minutes has little additional effect. If separation is incomplete and the mononuclear cell “band” (or layer) is not disturbed, the Vacutainer™ CPT™ Tube may be recentrifuged. 4. Time Blood samples should be centrifuged within two hours of collection. Red blood cell contamination of the separated mononuclear cell fraction increases with increasing delay before centrifugation. Mononuclear cell recovery decreases with increased time delay before centrifugation, falling to approximately 40% mononuclear cell recovery at 24 hours. 5. Microbial Contamination Microbial contamination of reagents may alter the results obtained on cells separated using Vacutainer™ CPT™ Tubes. Reference: Becton Dickinson Website: Report No. R-91-23-TA-143, Becton Dickinson Vacutainer™ Systems, NJ. CHAPTER 4: Obstetric Baseline Visit 9/13/06 Page 4 - 9 4.5.2. Collection and Storage of Maternal Serum After collection of maternal blood in a 5 ml draw red-topped SST (serum separator tube) the tube should sit at room temperature for 45 minutes to allow clot formation. The SST tube can be labeled with a “paperwork” barcode label (ending in “000”) provided in the MOTOR packet #1 (baseline). After centrifuging the SST for at least 10 minutes (spin time will depend on RCF that can be achieved on the particular centrifuge used) to produce adequate separation of serum, using appropriate PPE (personal protective equipment) for protection from possible bloodborne pathogens, carefully decap the SST and transfer the serum to the red-capped vials barcoded “301” to “304” (suffixes) such that 0.7 to 1.0 ml of serum is placed in each of the 4 vials. These volumes can be judged “by eyeball” by experienced personnel and can be accomplished with uncalibrated plastic transfer pipets, or calibrated pipets (with sterile tips) can be used for this step. Whatever transfer method is used, care should be exercised to use sterile materials and not contaminate the samples or inside of the vials or caps with materials from other subjects, personnel, or material in the serum preparation environment. Once the serum has been aliquoted into the 4 barcoded tubes (making sure to match the first 6 digits of the barcode number on the tubes with the number on the SST collection tube) make sure an identifying paperwork label that matches is affixed to the specimen collection form. After aliquoting the blood, place the tubes (301-304) either on dry ice or, at or below -80°C. CHAPTER 4: Obstetric Baseline Visit 9/13/06 Page 4 - 10