ENTEROBACTERIACEAE
advertisement
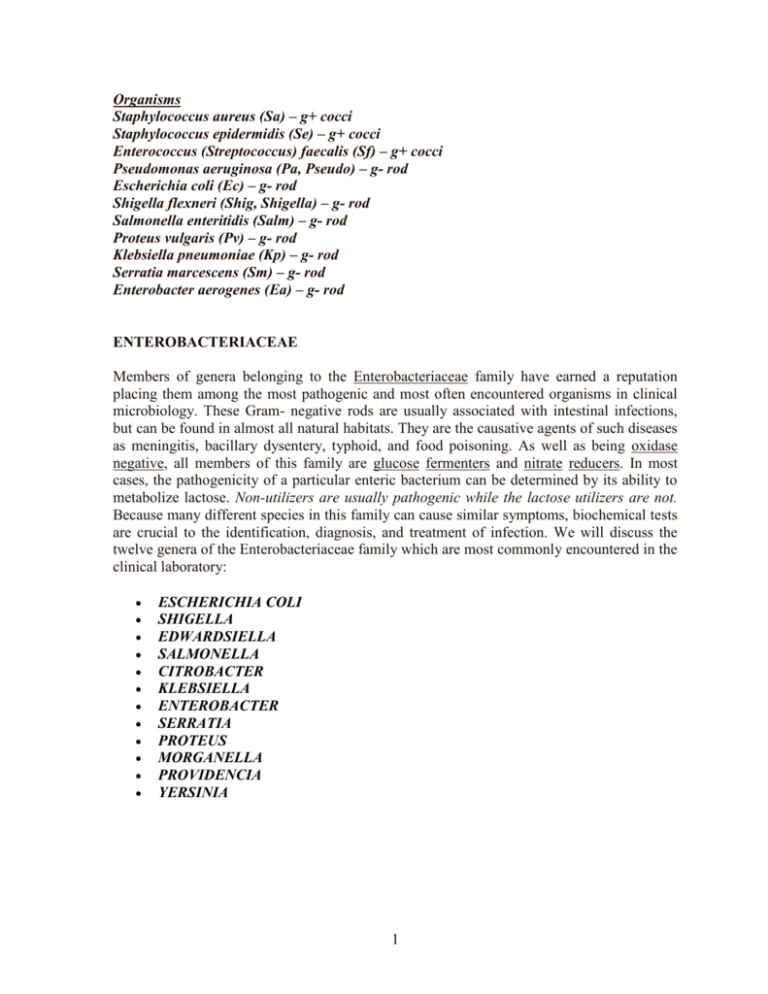
Organisms Staphylococcus aureus (Sa) – g+ cocci Staphylococcus epidermidis (Se) – g+ cocci Enterococcus (Streptococcus) faecalis (Sf) – g+ cocci Pseudomonas aeruginosa (Pa, Pseudo) – g- rod Escherichia coli (Ec) – g- rod Shigella flexneri (Shig, Shigella) – g- rod Salmonella enteritidis (Salm) – g- rod Proteus vulgaris (Pv) – g- rod Klebsiella pneumoniae (Kp) – g- rod Serratia marcescens (Sm) – g- rod Enterobacter aerogenes (Ea) – g- rod ENTEROBACTERIACEAE Members of genera belonging to the Enterobacteriaceae family have earned a reputation placing them among the most pathogenic and most often encountered organisms in clinical microbiology. These Gram- negative rods are usually associated with intestinal infections, but can be found in almost all natural habitats. They are the causative agents of such diseases as meningitis, bacillary dysentery, typhoid, and food poisoning. As well as being oxidase negative, all members of this family are glucose fermenters and nitrate reducers. In most cases, the pathogenicity of a particular enteric bacterium can be determined by its ability to metabolize lactose. Non-utilizers are usually pathogenic while the lactose utilizers are not. Because many different species in this family can cause similar symptoms, biochemical tests are crucial to the identification, diagnosis, and treatment of infection. We will discuss the twelve genera of the Enterobacteriaceae family which are most commonly encountered in the clinical laboratory: ESCHERICHIA COLI SHIGELLA EDWARDSIELLA SALMONELLA CITROBACTER KLEBSIELLA ENTEROBACTER SERRATIA PROTEUS MORGANELLA PROVIDENCIA YERSINIA 1 I. ESCHERICHIA COLI E. coli, the whipping boy of microbiology and genetics labs around the world, is the most encountered bacterium in the clinical laboratory. Besides being the number one cause of human urinary tract infections, E. coli has been linked to diseases in just about every other part of the body. Pneumonia, meningitis, and traveler's diarrhea are among the many illnesses that pathogenic strains of E. coli can cause. As part of the normal flora of the human intestinal tract, E. coli plays a crucial role in food digestion by producing vitamin K from undigested material in the large intestine. Pathogenic strains of E. coli, however, can cause severe cases of diarrhea in all age groups by producing a powerful endotoxin. Treating E. coli infections with antibiotics may actually place the patient in severe shock which could possibly lead to death. This is due to the fact that more of the bacterium's toxin is released when the cell dies. Below are two examples of E. coli growing on eosin methylene blue (EMB) agar. LABORATORY INDICATIONS: Lysine + Citrate Indol + Acetate + Lactose + II. SHIGELLA Shigella is closely related to Escherichia and is considered, by some scientists, to be another strain of E. coli. However, because Shigella is anaerogenic (does not produce gas from carbohydrates) and lactose (-), it is usually discernable from E. coli. In many cases, a Shigella infection will lead to diarrhea accompanied by fever. Shigella is also an invasive pathogen which can be recovered from the bloody stool of an infected host. Invasive pathogens colonize the host's tissues as opposed to growing on tissue surfaces. The four species in this genus are sometimes referred to by a letter designation based on their serologocal antigen: Serotype A- S. dysenteriae Serotype B- S. flexneri Serotype C- S. boydii Serotype D- S. sonnei 2 Strain D is the causative agent of most cases of Shigella-related diarrhea (shigellosis), while strain C species are rarely encountered in the laboratory. Shigella is easily spread from host to host, which should make it the primary suspect in outbreaks of diarrhea. LABORATORY INDICATIONS: Lysine non-motile -/+ TSI reaction (no gas) Acetate Lactose III. SALMONELLA Salmonella bacteria are instigated in more than 50,000 cases of bacterial food poisoning in the United States every year. Transmission of this microbe is usually through uncooked meats and eggs. Chickens are a major reservoir of Salmonella, which explains its ubiquitous presence in poultry products. Ingesting foods contaminated with significant amounts of Salmonella can cause intestinal infection which can eventually lead to diarrhea, vomiting, chills, and a really big headache. The 2200 known species of Salmonella are classified according to their surface antigens. The capsular properties of this Gram-negative rod can cause serious complications in immunosuppressed individuals such as HIV/AIDS patients. In the United States, S. typhimurium and S. enteritidis are the two leading causes of salmonellosis (inflammation of the intestine caused by Salmonella). While most Salmonella are carried by animals, S. typhi is unique because it is only carried by humans. This intracellular parasite can cause typhoid fever (enteric fever) which is characterized by fever, diarrhea, and inflammation of the infected organs. Most Salmonella infections can be treated with ciprofloxacin or ceftriaxone. LABORATORY INDICATIONS: Lysine + Hydrogen sulfide + -/+ TSI reaction (with gas) Indole + Citrate + ONPG Malonate IV. KLEBSIELLA The most clinically important species of this genus is Klebsiella pneumoniae. This large, non-motile bacterium produces large sticky colonies when plated on nutrient media. Klebsiella's pathogenicity can be attributed to its production of a heat-stable enterotoxin. K. pneumoniae infections are common in hospitals where they cause pneumonia (characterized by emission of bloody sputum) and urinary tract infections in catheterized patients. In fact, K. 3 pneumoniae is second only to E. coli as a urinary tract pathogen. Klebsiella infections are encountered far more often now than in the past. This is probably due to the bacterium's antibiotic resistance properties. Klebsiella species may contain resistance plasmids (Rplasmids) which confer resistance to such antibiotics as ampicillin and carbenicillin. To make matters worse, the R-plasmids can be transferred to other enteric bacteria not necessarily of the same species. LABORATORY INDICATIONS: Lysine + Citrate + Indol +/+ TSI (with gas) Non-motile Ornithine V. ENTEROBACTER Enterobacter includes eleven species of highly motile bacteria. The Enterobacter species is biochemically similar to Klebsiella, but unlike Klebsiella Enterobacter is ornithine positive. Although this bacterium is part of the normal flora of the human intestinal tract, several species cause opportunistic infections of the urinary tract as well as other parts of the body. E. aerogenes and E. cloacae are two such pathogens that do not cause diarrhea, but that are sometimes associated with urinary tract and respiratory tract infections. LABORATORY INDICATIONS: Lysine + (except E. cloacae) Citrate + Indol +/+ TSI (with gas) Motile Ornithine + VI. SERRATIA Members of the Serratia genus were once known as harmless organisms that produced a characteristic red pigment. Today, Serratia marcescens is considered a harmful human pathogen which has been known to cause urinary tract infections, wound infections, and pneumonia. Serratia bacteria also have many antibiotic resistance properties which may become important if the incidence of Serratia infections dramatically increases. Serratia can be distinguished from other genera belonging to Enterobacteriaceae by its production of three special enzymes: DNase, lipase, and gelatinase. LABORATORY INDICATIONS: Lysine + Citrate + Indol - 4 +/+ TSI (No gas) DNase + VII. PROTEUS Proteus, like almost every other bacterium in this family, can cause urinary tract infections and hospital-acquired infections. Proteus is unique, however, because it is highly motile and does not form regular colonies. Instead, Proteus forms what are known as "swarming colonies" when plated on non-inhibitory media. The most important member of this genus is considered to be P.mirabilis, a cause of wound and urinary tract infections. Fortunately, most strains of P. mirabilis are sensitive to ampicillin and cephalosporins. Unlike its relative, P. vulgaris is not sensitive to these antibiotics. However, this organism is isolated less often in the laboratory and usually only targets immunosuppressed individuals. P. mirabilis and P. vulgaris can be differentiated by an indole test for which only P. vulgaris tests positive. LABORATORY INDICATIONS: Lysine Hydrogen sulfide + Motile Urease + 5 NONFERMENTERS The nonfermenters are classified as such because of the way they metabolize glucose and other carbohydrates. Specifically, the bacteria discussed in this section are Gram-negative rods that either don't ferment glucose for energy or do not use glucose at all. This is a very diverse group of organisms in that they are not classified by DNA homology. These are also some of the most difficult bacteria to identify because they are negative for so many tests. Many nonfermenters do not grow on MacConkey agar. The two most common identification used for these organisms are the OF-glucose test and the triple sugar iron (TSI) test. We will discuss only the clinically significant organisms. PSEUDOMONAS Pseudomonads are motile, Gram-negative rods that utilize glucose oxidatively. Members of this genus are classified into five groups based on ribosomal RNA homology. These bacteria are clinically important because they are resistant to most antibiotics and they are capable of surviving in conditions that few other organisms can tolerate. They also produce a slime layer that is resistant to phagocytosis. Pseudomonas is often encountered in hospital and clinical work because it is a major cause of hospital acquired (nosocomial) infections. Its main targets are immunocompromised individuals, burn victims, and individuals on respirators or with indwelling catheters. Additionally, these pathogens colonize the lungs of cystic fibrosis patients, increasing the mortality rate of individuals with the disease. Infection can occur at many sites and can lead to urinary tract infections, sepsis, pneumonia, pharyngitis, and a lot of other problems. Rarely will you find Pseudomonas as a cause of infection in healthy individuals. Its non-invasive nature limits its pathogenic capabilities. P. aeruginosa Pseudomonas aeruginosa is the most frequently isolated non-fermenter in the laboratory. It has several features that distinguish it from other species of Pseudomonas: It can grow at 42 degrees celsius Produces a bluish pigment (pyocyanin) and a greenish pigment Characteristic fruity odor The basis of this organisms pathogenicity involves several toxins and chemicals which the bacterium secretes upon infection. The lipopolysaccharide layer helps the cell adhere to host tissues and prevents leukocytes from ingesting and lysing the organism. Lipases and exotoxins then proceed to destroy host cell tissue which then leads to the complications associated with infection. P. aeruginosa prefers to inhabit moist environments but it can survive in a medium as deficient as distilled water. It will also grow on just about any laboratory medium and is beta-hemolytic on blood agar. Treatment of Pseudomonas infection consists of a combination of two antibiotics: for example anti-pseudomonas penicillin and an aminoglycoside. The best way to reduce the spread of P. aeruginosa in the hospital is to use good aseptic technique on hospital instruments and when in contact with patients. 6 LABORATORY INDICATIONS: Oxidase + Beta-hemolytic Characteristic odor and color Motile Triple sugar iron agar (TSI) is a differential medium that contains lactose, sucrose, a small amount of glucose (dextrose), ferrous sulfate, and the pH indicator phenol red. It is used to differentiate enterics based on the ability to reduce sulfur and ferment carbohydrates. As with the phenol red fermentation broths, if an organism can ferment any of the three sugars present in the medium, the medium will turn yellow. If an organism can only ferment dextrose, the small amount of dextrose in the medium is used by the organism within the first ten hours of incubation. After that time, the reaction that produced acid reverts in the aerobic areas of the slant, and the medium in those areas turns red, indicating alkaline conditions. The anaerobic areas of the slant, such as the butt, will not revert to an alkaline state, and they will remain yellow. This happens with Salmonella and Shigella. NOTE: TSI medium should be read after an incubation of only 24 hours because a longer incubation time can cause a false negative. Vigorous fermenters such as Escherichia coli and Entrobacter cloacae will ferment all the available sugars and then begin using the amino acids. This will produce amine groups and cause the medium to turn alkaline. If an organism can reduce sulfur, the hydrogen sulfide gas which is produced will react with the iron to form iron sulfide, which appears as a black precipitate. If the precipitate is formed, it can mask any acid/alkaline results. Sulfur reduction requires an acidic environment, so if the black precipitate is present, some fermentation took place. If the butt of the slant is obscured by the precipitate, look at the top of the slant to determine if the organism could ferment only dextrose (red), or if it could ferment either lactose and/or sucrose (yellow). If the fermentation produced gas, you may see fissures in the medium, or the entire slant may be raised above the bottom of the test tube. 7 Enterobacter cloacae exhibits fermenation of glucose and gas production but no sulfur reduction. This would be read K/A,G. Staphylococcus aureus exhibits acidic fermentation. This would be read A/A. Salmonella typhimurium ferments glucose and reduces sulfur. This would be read K/A, H2S. Micrococcus luteus uses the amino acids and does not grow in the butt of the slant. This would be read K/NC. 8 Bacillus megaterium fermented sugars but did not grow in the anaerobic environment of the butt. This would be read A/NC. Enterobacter aerogenes fermented the sugars but turned to the amino acids. This would be read K/A. Results (slant/butt) Symbol Interpretation Red/yellow K/A Glucose fermentation only; Peptone catabolized Yellow/yellow A/A Glucose and lactose and/or sucrose fermentation Red/red K/K No fermentation; Peptone catabolized K/NC No fermentation; Peptone used aerobically Yellow/yellow with bubbles A/A,G Glucose and lactose and/or sucrose fermentation; Gas produced Red/yellow with bubbles K/A,G Glucose fermentation only; Gas produced Red/yellow with bubbles and black precipitate K/A,G, H2S Glucose fermentation only; Gas produced; H2S Red/no color change 9 produced Red/yellow with black precipitate K/A, H2S Glucose fermentation only; H2S produced Yellow/yellow with black precipitate A/A, H2S Glucose and lactose and/or sucrose fermentation; H2S produced No change/no change NC/NC No fermentation A=acid production; K=alkaline reaction; G=gas production; H2S=sulfur reduction Phenol Red Broth is a general-purpose differential test medium typically used to differentiate gram negative enteric bacteria. It contains peptone, phenol red (a pH indicator), a Durham tube, and one carbohydrate. We use three different kinds of phenol red broths. One contains glucose; one contains lactose, and the last contains sucrose. The objective of the exercise is to determine which organisms can utilize each sugar. Phenol red is a pH indicator which turns yellow below a pH of 6.8 and fuchsia above a pH of 7.4. If the organism is able to utilize the carbohydrate, an acid by-product is created, which turns the media yellow. If the organism is unable to utilize the carbohydrate but does use the peptone, the by-product is ammonia, which raises the pH of the media and turns it fuchsia. When the organism is able to use the carbohydrate, a gas by-product may be produced. If it is, an air bubble will be trapped inside the Durham tube. If the organism is unable to utilize the carbohydrate, gas will not be produced, and no air bubble will be formed. More in-depth information on the biochemical pathways involved in carbohydrate fermentation can be found in your lab manual. Important: When you retrieve the fermentation broths from the racks on the side counter, be sure to label them immediately! If you become confused as to which carbohydrate is in which tube, your results will be useless. 10 Picture coming soon The tube on the far left, which was inoculated with Escherichia coli, produces acid and gas. It would be read as A/G. The second tube from the left, which was inoculated with Enterococcus faecalis, produces acid but no gas. It would be read as A/-. The Alcaligenes faecalis degrades peptone and creates an alkaline by-product. It would be read as K. The Micrococcus luteus provides no reaction and would be read as -/-. 11 The IMViC tests are useful for differentiating the Enterobacteriaceae, especially when used alongside the urease test. When used alone, the IMViC tests are particularly useful for differentiating Escherichia coli, Enterobacter aerogenes, Enterobacter cloacae, and Klebsiella pneumoniae (although colonial morphology and the presence of capsules can also be used to differentiate Klebsiella). The IMViC series includes four tests: Indole production (for which we use SIM medium) the methyl red test the Voges-Proskauer test and citrate production Except for the lowercase “i”, which is added for ease of pronunciation, each of the letters in “IMViC” stands for one of these tests. “I” is for indole; “M” is for methyl red; “V” is for Voges-Proskauer, and “C” is for citrate. Simmons citrate agar tests the ability of organisms to utilize citrate as a carbon source. Simmons citrate agar contains sodium citrate as the sole source of carbon, ammonium dihydrogen phosphate as the sole source of nitrogen, other nutrients, and the pH indicator bromthymol blue. This test is part of the IMViC tests and is helpful in differentiating the Enterobacteriaceae. Organisms which can utilize citrate as their sole carbon source use the enzyme citrase or citrate-permease to transport the citrate into the cell. These organisms also convert the ammonium dihydrogen phosphate to ammonia and ammonium hydroxide, which creates an alkaline environment in the medium. At pH 7.5 or above, bromthymol blue turns royal blue. At a neutral pH, bromthymol blue is green, as evidenced by the uninoculated media. If the medium turns blue, the organism is citrate positive. If there is no color change, the organism is citrate negative. Some citrate negative organisms may grow weakly on the surface of the slant, but they will not produce a color change. 12 When Simmons Citrate agar is inoculated with Salmonella typhimurium, the medium turns royal blue. This is a positive result for the citrate test. When Simmons Citrate agar is inoculated with Escherichia coli, the medium remains green. This is a negative result for the citrate test. Methyl Red (MR) and Voges-Proskauer (VP) broth is used as a part of the IMViC tests as the medium in which both the Methyl Red and Voges-Prosakuer tests can be 13 performed. It is a simple broth that contains peptone, buffers, and dextrose or glucose. Different bacteria convert dextrose and glucose to pyruvate using different metabolic pathways. Some of these pathways produce unstable acidic products which quickly convert to neutral compounds. Some organisms use the butylene glycol pathway, which produces neutral end products, including acetoin and 2,3-butanediol. Other organisms use the mixed acid pathway, which produces acidic end products such as lactic, acetic, and formic acid. These acidic end products are stable and will remain acidic. The Methyl Red test involves adding the pH indicator methyl red to an inoculated tube of MR-VP broth. If the organism uses the mixed acid fermentation pathway and produces stable acidic end-products, the acids will overcome the buffers in the medium and produce an acidic environment in the medium. When methyl red is added, if acidic end products are present, the methyl red will stay red. NOTE: Methyl red differs from phenol red (which is used in the fermentation test and the MSA plates) in that it is yellow at pH 6.2 and above and red at pH 4.4 and below. Phenol red turns yellow below a pH of 6.8. If you get these two pH indicators confused, you will have a difficult time interpreting test results. The VP test detects organisms that utilize the butylene glycol pathway and produce acetoin. When the VP reagents are added to MR-VP broth that has been inoculated with an organism that uses the butylene glycol pathway, the acetoin end product is oxidized in the presence of potassium hydroxide (KOH) to diacetyl. Creatine is also present in the reagent as a catalyst. Diacetyl then reacts to produce a red color. Therefore, red is a positive result. If, after the reagents have been added, a copper color is present, the result is negative. The MR and VP tests are particularly useful in the identification of the Enterobacteriaceae. Important: Instead of making you aliquot inoculated broth into sterile test tubes, we have already divided the broth. Inoculate two MR-VP broths for each organism you wish to test. For the lab exercise, you would inoculate two MR-VP broths with Escherichia coli and two MR-VP broths with Enterobacter cloacae. After incubation, you would perform an MR test on one tube of Escherichia coli and one tube of Enterobacter cloacae, and you would perform a VP test on the other tube of Escherichia coli and the other tube of Enterobacter cloacae. 14 When methyl red is added to MR-VP broth that has been inoculated with Enterobacter cloacae, it turns yellow. This is a negative MR result. When methyl red is added to MR-VP broth that has been inoculated with Escherichia coli, it stays red. This is a positive result for the MR test. 15 When the VP reagents are added to MR-VP broth that has been inoculated with Escherichia coli, the media turns a copper color. This is a negative result for the VP test. When the VP reagents are added to MR-VP broth that has been inoculated with Enterobacter cloacae, the media turns red. This is a positive VP result. 16 SIM medium is a combination differential medium that tests three different parameters, which are represented by the three letters in the name: Sulfur Reduction Indole Production Motility The sulfur reduction test is useful in differentiating enteric organisms. The indole test is a component of the IMViC series of tests, which is used for differentiating the Enterobacteriaceae. The motility test is useful for testing a wide variety of organisms. As a whole, the SIM test is primarily useful for differentiating Salmonella and Shigella. SIM medium contains nutrients, iron, and sodium thiosulfate. One of the nutrients is peptone, which contains amino acids, including tryptophan. If an organism can reduce sulfur to hydrogen sulfide, the hydrogen sulfide will combine with the iron to form ferric sulfide, which is a black precipitate. If there is any blackening of the medium, it indicates the reduction of sulfur and is a positive result. The sulfur and motility test results should be determined before you perform the indole test. Some bacteria possess the ability to produce the enzyme tryptophanase, which hydrolyzes tryptophan. The end products of this hydrolyzation are indole, pyruvic acid, and ammonia, by way of deamination. The Kovac’s reagent that you add to the SIM medium to test for indole contains hydrochloric acid, pdimethylaminobenzaldehyde (DMABA), and n-amyl alcohol. DMABA reacts with indole to produce a red quinoidal compound. If the reagent turns red, the indole test is positive. 17 Before the Kovac’s reagent has been added: Streptococcus pyogenes is negative for motility and sulfur reduction. Serratia marcescens is positive for motility and negative for sulfur reduction. Salmonella typhimurium is positive for motility and for sulfur reduction. The tube on the far right has not been inoculated. 18 With the Kovac’s reagent added: Streptococcus pyogenes is negative for indole production. Escherichia coli is positive for indole production. Salmonella typhimurium is negative for indole production. Proteus vulgaris is positive for indole production. The catalase test identifies organisms which produce the catalase enzyme; this enzyme converts hydrogen peroxide to water and oxygen gas. This enzyme helps protect bacterial cells against hydrogen peroxide. Hydrogen peroxide is a highly-reactive compound which damages cell components. It is sometimes formed when the electron transport chain is used to produce energy. This test is particularly useful in differentiating staphylococci and micrococci, which are catalase-positive, from streptococci and enterococci, which are catalase-negative. When a catalase-positive organism is exposed to hydrogen peroxide, the hydrogen peroxide will bubble. We use 3% hydrogen peroxide, which is the same concentration 19 as the H2O2 you can buy in the store. NOTE: Use the slide test. Do not test organisms from a blood agar plate, as the blood will yield a false positive. Many organisms are catalase-positive; if your unknown tests catalase-positive, it is not necessarily a Staphylococcus. The oxidase test identifies organisms that produce the enzyme cytochrome oxidase. Cytochrome oxidase participates in the electron transport chain by transferring electrons from a donor molecule to oxygen. The oxidase reagent contains a chromogenic reducing agent, which is a compound that changes color when it becomes oxidized. If the test organism produces cytochrome oxidase, the oxidase reagent will turn blue or purple within 15 seconds. You can find the test protocol here. Mannitol Salt Agar (MSA) is a selective and differential medium. The high concentration of salt (7.5%) selects for members of the genus Staphylococcus, since they can tolerate high saline levels. Organisms from other genera may grow, but they typically grow very weakly. MSA also contains the sugar mannitol and the pH indicator phenol red. If an organism 20 can ferment mannitol, an acidic byproduct is formed that will cause the phenol red in the agar to turn yellow. Most pathogenic staphylococci, such as Staphylococcus aureus, will ferment mannitol. Most non-pathogenic staphylococci will not ferment mannitol. The Staphylococcus aureus ferments mannitol and turns the medium yellow. The Serratia marcescens does not grow because of the high salt content. Streptococcus agalactiae does not grow on MSA because of the high salt content. Staphylococcus epidermidis grows but does not ferment mannitol. Eosin methylene blue agar (EMB) is a selective and differential medium used to isolate fecal coliforms. Eosin Y and methylene blue are pH indicator dyes which combine to form a dark purple precipitate at low pH; they also serve to inhibit the growth of most 21 Gram positive organisms. Sucrose and lactose serve as fermentable carbohydrate sources which encourage the growth of fecal coliforms and provide a means of differentiating them. Vigorous fermenters of lactose or sucrose will produce quantities of acid sufficient to form the dark purple dye complex. The growth of these organisms will appear dark purple to black. Escherichia coli, a vigorous fermenter, often produces a green metallic sheen. Slow or weak fermenters will produce mucoid pink colonies. Normally-colored or colorless colonies indicate that the organism ferments neither lactose nor sucrose and is not a fecal coliform. Escherichia coli often produces a metallic green sheen on EMB. Enterobacter aerogenes and Enterobacter cloacae both form pink colonies on EMB. 22 Salmonella typhimurium and Pseudomonas aeruginosa both form colorless colonies. MacConkey Agar (MAC) is a selective and differential medium designed to isolate and differentiate enterics based on their ability to ferment lactose. Bile salts and crystal violet inhibit the growth of Gram positive organisms. Lactose provides a source of fermentable carbohydrate, allowing for differentiation. Neutral red is a pH indicator that turns red at a pH below 6.8 and is colorless at any pH greater than 6.8. Organisms that ferment lactose and thereby produce an acidic environment will appear pink because of the neutral red turning red. Bile salts may also precipitate out of the media surrounding the growth of fermenters because of the change in pH. Nonfermenters will produce normally-colored or colorless colonies. 23 Klebsiella pneumoniae ferments lactose and produces pink colonies on MAC. Micrococcus luteus does not grow in the presence of bile salts and crystal violet. Salmonella typhimurium does not ferment lactose and produces colorless colonies. Pseudomonas aeruginosa also does not ferment lactose, but since it normally produces a diffusible blue-green, water-soluble pigment, its colonies do not appear colorless GRAM-POSITIVE COCCI The Gram-positive cocci are grouped together based on their Gram-stain reaction, 24 thick cell wall composition, and spherical shape. Most of the organisms in these groups are members of the Micrococcaceae family All of the organisms in these groups are non-endospore forming chemosynthetic heterotrophs. We will discuss only the clinically relevent bacteria from Micrococcus and Staphylococcus of the Micrococcaceae family. Streptococcus and Enterococcus (formerly a species of Streptococcus) are discussed as well because of the many diseases they inflict on humans. The chart below shows the paths to identification of the genera discussed. STAPHYLOCOCCUS Clinically, the most important genus of the Micrococcaceae family is Staphylococcus. The Staphylococcus genus is classified into two major groups: aureus and non-aureus. S. aureus is a leading cause of soft tissue infections, as well as toxic shock syndrome (TSS) and scalded skin syndrome. It can be distinguished from other species of Staph by a positive result in a coagulase test(all other species are negative). The pathogenic effects of Staph are mainly asssociated with the toxins it produces. Most of these toxins are produced in the stationary phase of the bacterial growth curve. In fact, it is not uncommon for an infected site to contain no viable Staph cells. The S. aureus enterotoxin causes quick onset food poisoning which can lead to cramps and severe vomiting. Infection can be traced to contaminated meats which have not been fully cooked. These microbes also secrete leukocidin, a toxin which destroys white blood cells and leads to the formation of pus and acne. Particularly, S. aureus has been 25 found to be the causative agent in such ailments as pneumonia, meningitis, boils, arthritis, and osteomyelitis (chronic bone infection). Most S. aureus are penicillin resistant, but vancomycin and nafcillin are known to be effective against most strains. Of the non-aureus species, S. epidermis is the most clinically significant. This bacterium is an opportunistic pathogen which is a normal resident of human skin. Those susceptible to infection by the bacterium are IV drug users, newborns, elderly, and those using catheters or other artificial appliances. Infection is easily treatable with vancomycin or rifampin. LABORATORY INDICATIONS: Anaerobic glucose fermentation with acid production Catalase + Nitrate + Coagulase + 26 MICROCOCCUS Micrococcus is a Gram-positive, aerobic bacterium which is a member of the Micrococcaceae family. Micrococcus cells can be observed under the microscope as spherical cells forming pairs or clusters. If cultured in broth or on nutrient agar, the colonies may be red or yellow when observed unstained. Although these bacteria are a common human skin contaminant, they are relatively harmless to humans because they maintain a saprophytic lifestyle. They can also be found in freshwater environments or in soil. Three common species of Micrococcus are M. luteus, M. roseus, and M. varians. LABORATORY INDICATIONS: o o o Catalase + Oxidative action on glucose Growth on mannitol 27 STREPTOCOCCUS The Streptococcus genus consists of Gram-positive, aerobic bacteria which appear as chains under microscopic observation. The organisms in this genus are characterized by a coccus appearance, a thick cell wall, and aerobic action on glucose. Four different classification systems exist for this important microorganism: CLINICAL Pyogenic Streptococci Oral Streptococci Enteric Streptococci, HEMOLYSYS alpha-hemolysis beta-hemolysis gamma-hemolysis SEROLOGICAL-Lancefield (A-H), (K-U) BIOCHEMICAL(physiological) GROUP A The first group in the Lancefield classification system includes only one species of Streptococcus, S. pyogenes. This particular opportunistic pathogen is responsable for about 90% of all cases of pharyngitis. A common form of pharyngitis is "Strep throat" which is characterized by inflamation and swelling of the throat, as well as development of pus-filled regions on the tonsils. Penicillin is usually administered to patients as soon as possible to quell the possibility of the infection spreading from the upper respiratory system into the lungs. Once in the lungs, the infection could give rise to pneumonia. Some cases also develop into rheumatic fever if left untreated. Other diseases linked to S. pyogenes are skin infections such as impetigo, cellulitis, and erysipelas. LABORATORY INDICATIONS: Catalase Beta-hemolysis Bacitracin sensitive GROUP B The B classification of Lansefield also includes only one bacterium, S. agalactiae. For years this bacterium has been the causative agent in mastitis in cows. Currently, it has been found to be a cause of sexually transmitted urogenital infections in females. Although infection is easily treated with penicillin, proper diagnosis is necessary for women nearing labor because the infection can easily spread to the child via the birth canal. 28 LABORATORY INDICATIONS: CAMP + Beta-hemolysis GROUP D Type D Streptococcus is the next clinically important bacterium because of the multitude of diseases it is known to cause. Although many are harmless, the pathogenic strains cause complications of the human digestive tract. This group has recently been reclassified into two divisions: Enterococcus and non-Enterococcus. The Enterococci include E. faecalis, a cause of urinary tract infections, and E. faecium, a bacterium resistant to many common antibiotics. Diseases such as septicemia, endocarrditis, and appendicitis have also been attributed to group D Strep. Fecal matter from infected individuals is a source for isolation and identification techniques. Once identified, Group D Strep can be treated with ampicillin alone or in combination with gentamicin. LABORATORY INDICATIONS: Hydrolysis of bile esculin (dark brown medium) -this indicates the ability of the bacteria to tolerate bile from the liver Growth in high salt conc. OTHER IMPORTANT STREP Streptococcus pneumoniae Because its surface carbohydrate antigens do not correspond to a specific Lancefield group, S. pneumonia is discussed separately. Although not given a letter designation, S. pneumoniae can be considered a Pyogenic (pus-producing) strain of Strep. It can be distinguished from other Pyogenic bacteria by its high sensitivity to Optochin (no growth zone of inhibition). This bacterium causes pneumonia (obviously!), meningitis, and otitis media. It also demonstrates alpha-hemolytic growth on blood agar. Viridans Group The Viridans Streptococci, consisting of S. mutans and S. mitis, are alpha-hemolytic bacteria. These bacteria inhabit the mouth. In fact, a large percentage of tooth decay can be attributed to S. mutans. 29