Therapy-related acute myeloid leukemia (monoblastic
advertisement
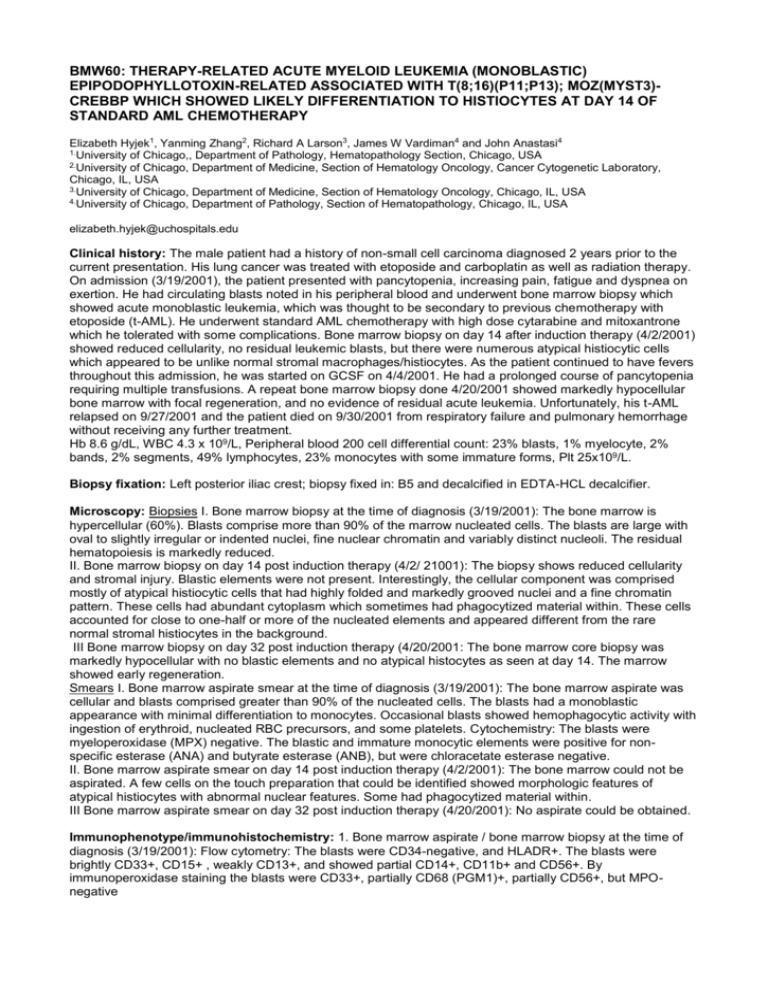
BMW60: THERAPY-RELATED ACUTE MYELOID LEUKEMIA (MONOBLASTIC) EPIPODOPHYLLOTOXIN-RELATED ASSOCIATED WITH T(8;16)(P11;P13); MOZ(MYST3)CREBBP WHICH SHOWED LIKELY DIFFERENTIATION TO HISTIOCYTES AT DAY 14 OF STANDARD AML CHEMOTHERAPY Elizabeth Hyjek1, Yanming Zhang2, Richard A Larson3, James W Vardiman4 and John Anastasi4 1.University of Chicago,, Department of Pathology, Hematopathology Section, Chicago, USA 2.University of Chicago, Department of Medicine, Section of Hematology Oncology, Cancer Cytogenetic Laboratory, Chicago, IL, USA 3.University of Chicago, Department of Medicine, Section of Hematology Oncology, Chicago, IL, USA 4.University of Chicago, Department of Pathology, Section of Hematopathology, Chicago, IL, USA elizabeth.hyjek@uchospitals.edu Clinical history: The male patient had a history of non-small cell carcinoma diagnosed 2 years prior to the current presentation. His lung cancer was treated with etoposide and carboplatin as well as radiation therapy. On admission (3/19/2001), the patient presented with pancytopenia, increasing pain, fatigue and dyspnea on exertion. He had circulating blasts noted in his peripheral blood and underwent bone marrow biopsy which showed acute monoblastic leukemia, which was thought to be secondary to previous chemotherapy with etoposide (t-AML). He underwent standard AML chemotherapy with high dose cytarabine and mitoxantrone which he tolerated with some complications. Bone marrow biopsy on day 14 after induction therapy (4/2/2001) showed reduced cellularity, no residual leukemic blasts, but there were numerous atypical histiocytic cells which appeared to be unlike normal stromal macrophages/histiocytes. As the patient continued to have fevers throughout this admission, he was started on GCSF on 4/4/2001. He had a prolonged course of pancytopenia requiring multiple transfusions. A repeat bone marrow biopsy done 4/20/2001 showed markedly hypocellular bone marrow with focal regeneration, and no evidence of residual acute leukemia. Unfortunately, his t-AML relapsed on 9/27/2001 and the patient died on 9/30/2001 from respiratory failure and pulmonary hemorrhage without receiving any further treatment. Hb 8.6 g/dL, WBC 4.3 x 109/L, Peripheral blood 200 cell differential count: 23% blasts, 1% myelocyte, 2% bands, 2% segments, 49% lymphocytes, 23% monocytes with some immature forms, Plt 25x109/L. Biopsy fixation: Left posterior iliac crest; biopsy fixed in: B5 and decalcified in EDTA-HCL decalcifier. Microscopy: Biopsies I. Bone marrow biopsy at the time of diagnosis (3/19/2001): The bone marrow is hypercellular (60%). Blasts comprise more than 90% of the marrow nucleated cells. The blasts are large with oval to slightly irregular or indented nuclei, fine nuclear chromatin and variably distinct nucleoli. The residual hematopoiesis is markedly reduced. II. Bone marrow biopsy on day 14 post induction therapy (4/2/ 21001): The biopsy shows reduced cellularity and stromal injury. Blastic elements were not present. Interestingly, the cellular component was comprised mostly of atypical histiocytic cells that had highly folded and markedly grooved nuclei and a fine chromatin pattern. These cells had abundant cytoplasm which sometimes had phagocytized material within. These cells accounted for close to one-half or more of the nucleated elements and appeared different from the rare normal stromal histiocytes in the background. III Bone marrow biopsy on day 32 post induction therapy (4/20/2001: The bone marrow core biopsy was markedly hypocellular with no blastic elements and no atypical histocytes as seen at day 14. The marrow showed early regeneration. Smears I. Bone marrow aspirate smear at the time of diagnosis (3/19/2001): The bone marrow aspirate was cellular and blasts comprised greater than 90% of the nucleated cells. The blasts had a monoblastic appearance with minimal differentiation to monocytes. Occasional blasts showed hemophagocytic activity with ingestion of erythroid, nucleated RBC precursors, and some platelets. Cytochemistry: The blasts were myeloperoxidase (MPX) negative. The blastic and immature monocytic elements were positive for nonspecific esterase (ANA) and butyrate esterase (ANB), but were chloracetate esterase negative. II. Bone marrow aspirate smear on day 14 post induction therapy (4/2/2001): The bone marrow could not be aspirated. A few cells on the touch preparation that could be identified showed morphologic features of atypical histiocytes with abnormal nuclear features. Some had phagocytized material within. III Bone marrow aspirate smear on day 32 post induction therapy (4/20/2001): No aspirate could be obtained. Immunophenotype/immunohistochemistry: 1. Bone marrow aspirate / bone marrow biopsy at the time of diagnosis (3/19/2001): Flow cytometry: The blasts were CD34-negative, and HLADR+. The blasts were brightly CD33+, CD15+ , weakly CD13+, and showed partial CD14+, CD11b+ and CD56+. By immunoperoxidase staining the blasts were CD33+, partially CD68 (PGM1)+, partially CD56+, but MPOnegative II. Bone marrow biopsy on day 14 post induction therapy (4/2/2001): Immunohistochemistry demonstrated numerous CD33+ histiocytic cells some of which showed an abnormal CD56 expression ssimilar to the leukemic blasts at the time of diagnosis. III. Bone marrow biopsy on day 32 post induction therapy (4/20/2001): Immunohistochemistry demonstrated a few areas of CD33+, CD68+ histiocytes, which were fairly mature appearing. Virtually no CD56+ histiocytes could be identified. Cytogenetics: 1. Bone marrow aspirate at the time of diagnosis (3/19/2001): Abnormal mosaic male karyotype with t(8;16)/MOZ(MYST3)-CREBBP fusion. 46,XY,t(8;16)(p11;p13)[3]/ 47,idem,+8,i(8)(q10)[10]/ 46,idem,der(7)t(7;8)(p22;q21)[7]/ 45,idem,der(11)t(8;11)(q21;q25),-20[1]/ 46,idem,der(19)t(8;19)(q21;p13)[1] FISH with CEP8 probe showed +8 in 12% of 400 cells analyzed. The cut-off value is 2% for a positive result. II. Bone marrow on day 14 post induction therapy (4/2/2001): There were only very few cells available for analysis and only FISH with a CEP8 probe could be performed, which showed +8 in 4.5% of cells, consistent with residual disease. III. Bone marrow on day 32 post induction therapy (4/20/2001): Cytogenetic analysis was not performed on bone marrow from 4/20/2001, but it was performed on bone marrow from 5/03/2001, which showed normal male karyotype: 46,XY[20]. FISH analysis was negative for the presence of trisomy 8. At the time of relapse on 9/28/2001 the bone marrow showed abnormal mosaic male karyotype with t(8;16) the MOZ(MYST3)-CREBBP fusion and many additional numerical and structural aberrations, indicating clonal evolution. 48,XY,t(2;19)(q23;p13.3),+8,i(8)(q10),t(8;16)(p11;p13),dic(1;12)(p22;p13),+13,del(17)(p11.3;p13)[5]/48,idem,dic(1;12),+der(12)t(1;12)(p22;p13)[8]/48,idem,dic(1;12),+add(12)(p13)[5]/48,idem,der(2)t(2;19)(q23;p13.3)add(2)q23),-dic(1;12),+add(12)(p13),del(17)(p11p13),+der(17)t(1;17)(q11;p11)[1]/48,idem,-dic(1;12),+der(12),+der(12)t(1;12)(q21;p13)[1]. Proposed diagnosis Therapy-related acute myeloid leukemia (monoblastic) with hemophagocytosis and associated t(8;16)(p11;p13); MOZ(MYST3)-CREBBP which showed likely differentiation to histiocytes at day 14 of standard AML chemotherapy. Interesting feature(s) of the submitted case This case represents a rare type of t-AML with monoblastic features associated with hemophagocytosis and t(8;16)(p11;p13); MOZ(MYST3)-CREBB secondary to topoisomerase II inhibitors and radiation therapy. The presence of atypical histiocytes at day 14 of chemotherapy which showed hemophagocytosis, and which were morphologically distinct from normal stromal histiocytes suggests that the leukemic monoblastic cells differentiated to mature histiocytes. This was supported by the persistence of the immunophenotypic abnormality of the leukemic cells noted at diagnosis (CD56-partial positivity), and by the persistence of cytogenetic clonality identified by FISH (trisomy 8). The case suggests that differentiating agents may have a potential role in the treatment of this type of leukemia.