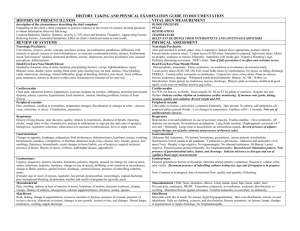
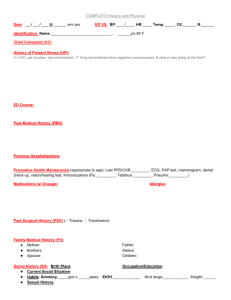
HISTORY OF PRESENT ILLNESS
advertisement
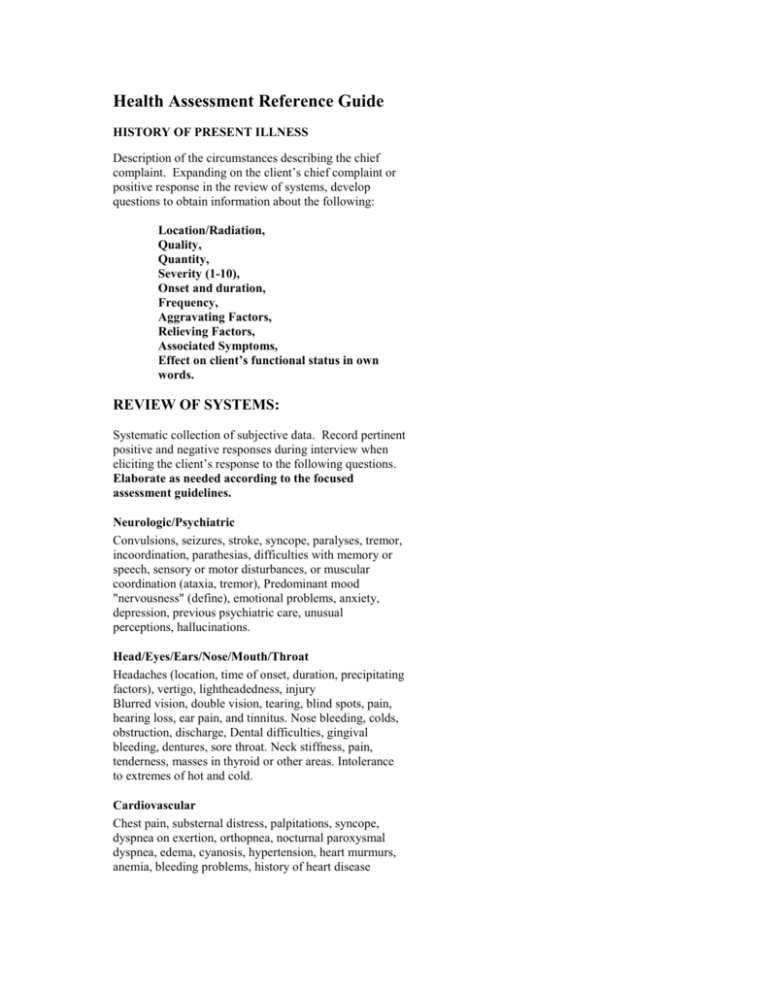
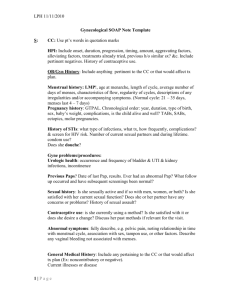
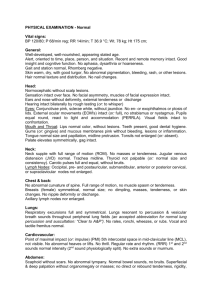
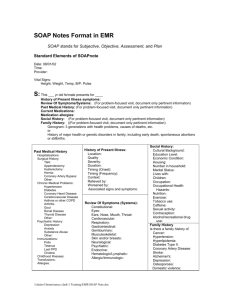
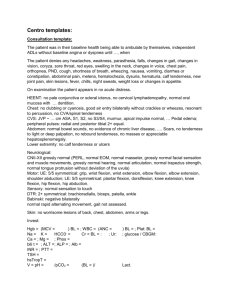
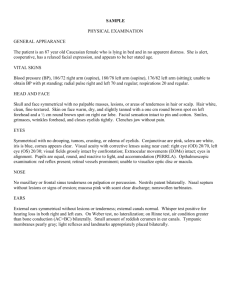
Health Assessment Reference Guide HISTORY OF PRESENT ILLNESS Description of the circumstances describing the chief complaint. Expanding on the client’s chief complaint or positive response in the review of systems, develop questions to obtain information about the following: Location/Radiation, Quality, Quantity, Severity (1-10), Onset and duration, Frequency, Aggravating Factors, Relieving Factors, Associated Symptoms, Effect on client’s functional status in own words. REVIEW OF SYSTEMS: Systematic collection of subjective data. Record pertinent positive and negative responses during interview when eliciting the client’s response to the following questions. Elaborate as needed according to the focused assessment guidelines. Neurologic/Psychiatric Convulsions, seizures, stroke, syncope, paralyses, tremor, incoordination, parathesias, difficulties with memory or speech, sensory or motor disturbances, or muscular coordination (ataxia, tremor), Predominant mood "nervousness" (define), emotional problems, anxiety, depression, previous psychiatric care, unusual perceptions, hallucinations. Head/Eyes/Ears/Nose/Mouth/Throat Headaches (location, time of onset, duration, precipitating factors), vertigo, lightheadedness, injury Blurred vision, double vision, tearing, blind spots, pain, hearing loss, ear pain, and tinnitus. Nose bleeding, colds, obstruction, discharge, Dental difficulties, gingival bleeding, dentures, sore throat. Neck stiffness, pain, tenderness, masses in thyroid or other areas. Intolerance to extremes of hot and cold. Cardiovascular Chest pain, substernal distress, palpitations, syncope, dyspnea on exertion, orthopnea, nocturnal paroxysmal dyspnea, edema, cyanosis, hypertension, heart murmurs, anemia, bleeding problems, history of heart disease Peripheral vascular Pain, numbness, swelling in extremities, temperature changes, discoloration or changes in color, varicose veins, infections, or ulcers. Claudication, asymmetry. Respiratory History of lung disease, pain (location, quality, relation to respiration), shortness of breath, wheezing, stridor, cough (time of day, of productive, amount in tablespoons or cups per day and color of sputum), hemoptysis, respiratory infections, tuberculosis (or exposure to tuberculosis), fever or night sweats. Gastrointestinal Changes in appetite, dysphagia, indigestion, food intolerances, abdominal pain, heartburn, nausea, vomiting, hematemesis, jaundice, constipation, or diarrhea, abnormal stools (clay-colored, tarry, bloody, greasy, foul smelling), flatulence, hemorrhoids, recent changes in bowel habits, use of laxatives, surgical incisions, presence of drains. History of ulcers, cirrhosis, gallbladder disease, appendicitis. Genitourinary Urgency, frequency, dysuria, nocturia, hematuria, polyuria, oliguria, unusual (or change in) color of urine, stones, infections, nephritis, hesitancy, change in size of stream, dribbling, acute retention or incontinence, change in libido, potency, genital lesions, discharge, venereal disease, presence of indwelling catheters, stents. (Female) Age of onset of menses, regularity, last period, dysmenorrhea, menorrhagia, vaginal discharge, postmenopausal bleeding, dyspareunia, number and results of pregnancies (gravida, para) Musculoskeletal Pain, swelling, redness or heat of muscles or joints, limitation, of motion, muscular weakness, atrophy, cramps. History of arthritis, osteoporosis, calcium supplementation, fractures, strains, sprains Skin/Breast Rash, itching, change in pigmentation, excessive moisture or dryness, presence of wounds, presence of invasive devices, alterations in texture, changes in hair growth , texture or loss, nail changes. Breast lumps, tenderness, swelling, nipple discharge VITAL SIGN MEASUREMENT BLOOD PRESSURE, PULSE, RESPIRATIONS TEMPERATURE Record relevant readings from intermittent and continuous monitors in the appropriate system assessment. PHYSICAL ASSESSMENT: Systematic collection of objective data utilizing the IPPA format. I: inspection P: palpation P: percussion A: auscultation Neurologic/Psychiatric Alert and oriented to person, place, time. Cooperative. Speech clear, appropriate, posture relaxed. Recent/remote memory intact. Cranial nerves II-XII intact. Sensation to pinprick, light touch intact. Motor: no atrophy, weakness or tremors bilaterally. Ambulates with steady gait. Negative Romberg’s sign. Performs alternating movement. DTR’s intact. Note if falls precaution is in effect and restraints in use Head/Eyes/Ears/Nose/Mouth/Throat Normocephalic, atraumatic. Facies symmetric, no weakness or involuntary movements noted. Visual acuity intact.20/20/ OD, OS. Full visual fields intact by confrontation. No ptosis, no lidlag, discharge PERRLA. Corneal reflex symmetric no strabismus. Conjunctive clear, sclera white. Pinna no masses, lesions, tenderness, drainage. Whispered words heard bilaterally. Rhinne: AC>BC. Weber: no lateralization. Nares patent, no tenderness, lesions, discharge. Pharynx pink, no lesions, dentition in good repair, uvula rises on midline, positive gag reflex. Cardiovascular No JVD. No heaves, no thrills. Heart sounds: S1, S2 no S3 S4 gallop or murmurs. Regular rate and rhythm. Indicate cardiac rhythm on continuous cardiac monitoring. If murmur note grade, timing, location, quality and radiation. Record weight and I/O. Peripheral vascular Color pink, no lesions, varicosities, symmetric bilaterally. Hair present. No edema, calf tenderness, all peripheral pulses present (Grade +), no changes in temperature. Capillary refill < 3 seconds. Note use of antithrombotics devices Respiratory Respirations even and unlabored, no use of accessory muscles. Trachea midline. Chest symmetric, AP diameter not increased. No tenderness on palpation. Lung fields resonant. Diaphragmatic excursion (4-7 cm) and = bilaterally. Lungs clear to auscultation, no adventitious sounds. Record presence of adjunct oxygen therapy, use of pulse oximetry and presence of thoracic tubes. Gastrointestinal Abdomen flat, symmetric. No lesions, herniations, gas patterns, venous patterns or pulsations. Normoactive bowel sounds in all quadrants. Tympanitic to percussion. Abdomen soft nontender. Liver span (7cm). Murphy’s sign negative. No organomegaly. No rebound tenderness, McBurney’s point negative. Femoral pulses present bilaterally. No lymphadenopathy. No CVA tenderness. Record bowel elimination pattern. Note presence of gastrointestinal tubes, drains, and dressings. Indicate tolerance to diet type and use of capillary blood sugar measurements Genitourinary External genitalia no lesions or discharge. Describe urinary pattern: continence, frequency, volume, color, odor clarity. Document presence of indwelling catheter noting size, type and if irrigation is in progress. Note if menses is in progress, date of menstrual flow, quality and quantity of bleeding. Musculoskeletal (TMJ, Neck, shoulders, elbows, wrists, hands, spine, hips, knees, ankle, feet) No joint pain, tenderness, FROM. Extremities symmetric, no tenderness, weakness, discoloration, or swelling. Maintains flexion against resistance. Vertebra nontender, no curvature, no deformity. Skin/Breast Skin pink warm dry to touch. No lesions, hyper/hypopigmentation. Hair even distribution, texture, no pest inhabitants. Nails no clubbing, cyanosis, and discoloration. Breasts symmetric: no lesions, lumps, changes in pigmentation or nipple discharge. No lymphadenopathy. FOCUSED ASSESSMENT GUIDE According to Carpenito-Moyet (2007), a focus assessment is a directed query or examination determined by the judgment of the nurse when a problem is suspected. It is derived from the client’s baseline assessment but generates specific data that either supports or refutes a diagnostic label. For the purpose of discussion, we will label a suspected problem as a tentative nursing diagnosis or collaborative problem. The query and examination are represented by the defining characteristics of the tentative nursing diagnosis or the presence of risk factors or clinical manifestations of a collaborative problem (medical diagnosis). In order to prepare to collect the appropriate subjective and objective data, the nurse categorizes the client’s condition, researches the diagnoses and collaborative problems associated with the condition and collects the subjective and objective data that either supports or rejects the presence of the diagnosis. If history taking and examination reveals the presence of the defining characteristics of the tentative diagnosis, then the nurse can make the diagnosis and develop a plan of care to treat it. If the client’s condition strongly supports the risk of experiencing the diagnosis but the defining characteristics are not present, the nurse develops a ‘risk for’ diagnostic statement and designs nursing actions that will control for the development of the problem. If the tentative diagnosis is not relevant to the client’s condition, the diagnosis is not included in the plan of care. References: Carpenito-Moyet, Lynda Juall (2007). Understanding Nursing Process: Concept Mapping and Care Planning for Students. Philadelphia, Pa. Lippincott Williams & Wilkins. Jarvis, Carolyn (2003). Physical Examination and Health Assessment, 4th Edition, Philadelphia, PA. W.B. Saunders Co. This product is intended for use by registered nursing students. It can not be sold, duplicated or distributed without permission of the author. Inquiries should be directed to Susan McCabe at mcjacobs@optonline.net