spr competency in haemostasis thrombosis
advertisement

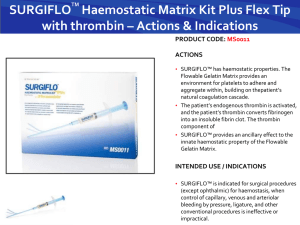
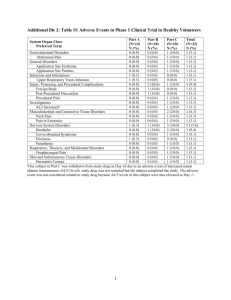
1 SpR Competency Assessment: training in haemostasis & thrombosis Local Hospital Address here Version 1.3 February 2010 2 1.0 Background & methods of assessment 1.1 Aim This document describes the skills and competences required by an SpR in order to meet a satisfactory level of competence in haemostasis and thrombosis in the UK. Competency assessment as described in this document does not constitute part of the formal training programme for SpRs in haematology in the UK as governed by Statutory bodies, for example PMETB, the Specialty Advisory Committee of the RCP or the RCPath's examination for FRCPath. However, it is suggested that the proposal could be used at the discretion of local trainers to objectively inform and contribute to: the RITA/ARCP process & career development; educational supervisor sponsorship for entry to FRCPath examinations; the portfolio of evidence for specialist training for purposes of certfication and validation. The purpose of the proposed competency assessments is to facilitate the ability of trainee haematologists to achieve the competency to deliver high quality patient care. It is anticipated that the assessment programme will promote development of professional competence through to 'safe to undertake unsupervised clinical and laboratory practice' (level 3 and above). It is intended to promote harmonisation of training and competency, both clinical and laboratory, in order to ensure that a trainee has reached a level of competence that is satisfactory for practice as a Consultant Haematologist in the UK. The programme can also be used as a framework for continuous professional development and maintenance of competence. 1.2 Assessment Methods of assessment will be determined by local arrangement. The frequency and opportunity for assessment at different levels of competence will depend on local training programmes and schedules. The competency assessments are intended to bring clarity to the training needs of trainees and identify training opportunities. It is anticipated that trainees will use the curriculum to direct learning and obtain experience and as an indication of when they are ready to present themselves for a competency assessment. It is suggested that competency assessments could be used to objectively inform the RITA/ARCP process through the educational supervisors reports and as part of the trainees e-portfolio and identify when candidates are suitable to proceed to FRCPath examinations. The appendices are suggested competencies at 4 levels. The required competencies will be defined by local trainers and should reflect what can be delivered by a local training programme in combination with what standard is expected for satisfactory performance in the haemostasis and thrombosis sections of the FRCPath examinations. It is anticipated that Version 1.3 February 2010 3 input on the content of the programme from trainee representatives would promote the usefulness of the assessments. It is suggested that the levels of competency assessment reflect the following levels of expertise: Level 1 - able to perform daily duties as an SpR with responsibility for haemostasis and thrombosis, including on-call competency Level 2 - level of competence reflecting standard expected for attainment of part 1 FRCPath Level 3 - level of competence reflecting standard expected for attainment of part 2 FRCPath Level 4 - higher level of competence reflecting special interest in haemostasis and thrombosis Interactive problem solving will be developed locally to reflect clinical and laboratory problems encountered in practice so as to ensure comprehensive training in all aspects of haemostasis and thrombosis. Version 1.3 February 2010 4 2.0 The Training Programme The Programme is informed by and is complimentary to the European Curriculum for Thrombosis & Haemostasis developed by the European Association for Haemophilia and Allied Disorders (EHA) (Astermark et al Haemophilia 2009;15:337 - 344) The SpR must develop competence in haemostasis and thrombosis and possess expertise in the diagnosis, assessment and treatment of patients with congenital and acquired bleeding and thrombotic disorders. As well as understanding the management of adult patients, it is important that there is appreciation of the specific requirements of infants and children as well as their families: direct responsibility for the immediate care of patients with thrombotic disorders, particularly those with venous thromboembolism (VTE), and especially those who present diagnostic or therapeutic difficulties; provide leadership and management of a community anticoagulant service to ensure that patients receive an appropriate level of antithrombotic therapy; provide a consultative service in the area of haemostasis and thrombosis to all hospital specialties and to general practitioners; oversee and advise on the general arrangements for service provision of haemostatic and thrombotic services to a wide range of hospital specialties and to the community; direct responsibility for the provision and management of a comprehensive care haemophilia service. This will require oversight of both the direct clinical care of patients with haemophilia and allied bleeding disorders and the diagnostic coagulation laboratory service. Knowledge of changes in haemostatic systems with age from birth onwards is especially important particularly to ensure that children are treated appropriately; quality control of laboratory and community based testing; the role of audit in the development of provision of care to individual patients. Training in haemostasis and thrombosis should involve supervised periods of responsibility for distinct aspects of both laboratory and clinical service. 2.1 General Competence Includes: the use and interpretation of guidelines; total quality management in the laboratory; understand and demonstrate the importance of comprehensive care and the cooperation with other healthcare professionals, including those who are experienced in looking after children, such that the roles of these professionals are delineated and consistent messages are delivered to the patient and their families; use of molecular biological techniques in diagnosis and in prenatal and family testing (molecular and phenotyping); Version 1.3 February 2010 5 background knowledge of genetic counselling and how to give information to the patient and family in a way that is understandable, encourages discussion and promotes the patient s participation in decision-making; 2.2 participate in interdisciplinary team meetings. Diagnostic procedures Includes: performance and interpretation of laboratory testing including issues relating to instruments/methods and their pitfalls; basic principles of laboratory management (e.g. setting of ranges, quality assurance, laboratory, computing, health and safety, accreditation); genetic features in haemostatic disorders (e.g. structural chromosomal changes, gene mutations, polymorphisms) and the implication of these for inheritance and genetic counseling. 2.3 Patient Safety Includes: Definition and classification of adverse events, risk management, root cause analysis and Patient Safety. Version 1.3 February 2010 6 3.0 Specific Competence 3.1 Use of antithrombotic agents Mechanisms of actions, pharmacology, therapeutic indications, dosing, monitoring, precautions and the side effects of: parenteral anticoagulants, including heparins, synthetic heparin analogues, direct thrombin inhibitors and anti-Xa inhibitors; oral anticoagulants, including warfarin, direct thrombin inhibitors, anti-Xa inhibitors. appropriate tests for anticoagulant control (e.g. INR), including self-testing, and different models of anticoagulant management, including computerised systems and implementation of multi-professional delivery of anticoagulant control; follow-up of patients receiving anticoagulants, including advice on duration and intensity of therapy and management of surgery/invasive procedures; withdrawal in association with invasive procedures and bridging with heparin; fibrinolytic drugs, including Streptokinase, Urokinase, t-PA; antiplatelet agents, including aspirin, dipyridamole, thienopyridrine derivatives and glycoprotein IIb/IIIa inhibitors; optimal management before invasive procedures including discontinuation in high risk situations (e.g. coronary stent and dual antiplatelet therapy). 3.2 Management of thrombotic disorders pathophysiology of and mechanisms involved in venous and arterial thrombosis; gene-environmental interactions in thrombosis; clinical and laboratory evaluation of hypercoagulable states, including age-specific normal ranges; epidemiology, molecular basis, appropriate use of clinical and laboratory methods to reach a diagnosis, including family history, and management of heritable thrombophilia including deficiencies in Protein C, S, antithrombin, factor V Leiden, prothrombin gene variant, dysfibrinogenaemias, abnormalities of fibrinolysis; cost/benefits and clinical effectiveness of screening for inheritable thrombophilias in specific populations; management of acquired hypercoagulable and thrombotic states, including those arising with the use of in-dwelling catheters, in association with malignancies, myeloproliferative disorders and other underlying disorders; Clinical significance of JAK-2 mutation and other cytogenetic abnormalities associated with a hypercoagulable state; diagnostic aspects and clinical management of acquired thrombotic disorders in association with pregnancy and postpartum, the use of oestrogen containing therapies (e.g. combined oral contraceptive and HRT), in the postoperative states and during immobility as well as other disorders; Version 1.3 February 2010 7 diagnostic aspects and clinical management of lupus anticoagulant and antiphospholipid syndrome; pathogenesis, risk factors, diagnosis and management of heparin-induced thrombocytopenia (HIT), including interpretation of bio-and immunoassays and use of alternative anticoagulants; microangiopathic conditions/TTP-HUS; natural history, clinical manifestations and complications of venous thrombosis; diagnostic aspects of VTE (DVT, PE) including the use of pretest probability scoring and D-Dimer; imaging techniques to diagnose VTE and PE; management of thrombosis in all locations including catheter-related episodes; clinical management of thromboembolism during pregnancy; assessment of risk factors and risk of recurrence from clinical assessment; prophylaxis of venous thrombosis and risk assessment; treatment of DVT and PE including the use of IVC filter; management of post-thrombotic syndrome; use and efficacy of mechanical methods employed for the prevention of VTE. epidemiology of arterial thrombosis; pathophysiology and prevention of the atherosclerotic process including cardio-and cerebrovascular risk factors; stroke and associated thrombophilic disorders including antiphospholipid antibodies, and hereditary thrombophilia; antithrombotic management of stroke including anticoagulation, antiplatelet agents and thrombolysis; diagnosis and clinical management of cerebral venous thrombosis; epidemiology, thromboembolism prevention and anticoagulant management of atrial fibrillation; anticoagulants, antiplatelet drugs and thrombolytics in acute events and interventions of acute coronary syndromes, acute myocardial infarction and percutaneous coronary interventions; haemostatic changes secondary to cardiac bypass and management of associated bleeding; thrombotic risk associated with broad categories of prosthetic heart valves, as well as long-term anticoagulation, management of invasive procedures and options in pregnancy. 3.3 Consultative haemostasis & thrombosis 3.3.1 Gynaecology/obstetrics Version 1.3 February 2010 8 effects of gender, pregnancy, oral contraceptive and hormone replacement therapy on haemostatic parameters; evaluation, characterization and treatment of menorrhagia; potential bleeding states arising in carriers of heritable bleeding disorders; management of carriers of bleeding disorders; risk estimation for VTE in pregnancy and in association with the use of OC and HRT in women with inherited thrombophilia; management of postpartum haemorrhage; anticoagulant treatment during pregnancy, postpartum and in the lactation period; diagnosis and management of thrombocytopenia in pregnancy, including gestational thrombocytopenia, ITP, HELLP, familial thrombocytopenia, foeto-maternal alloimmunisation. haemostatic aspects of foetal loss; clinical implications of lupus anticoagulants and antiphospholipid syndrome; diagnosis and management of haemostatic changes associated with pre-eclampsia. 3.3.2 Intensive care haemostatic aspects of the pathophysiology and clinical management of SIRS/Sepsis; pathophysiology and diagnosis of disseminated intravascular coagulation and consumptive coagulopathy, including the use of basic assays, activation markers, inflammatory markers and sepsis-related organ failure assessment; therapeutic options and clinical management of DIC and consumptive coagulopathy, including the use of heparin and physiological anticoagulants such as antithrombin and (activated) Protein C. anticoagulation for venoarterial extracorporeal membrane oxygenation. 3.3.3 Oncology awareness of the haemostatic and thrombotic complications association with malignant diseases due to the pathophysiological process itself or to the use of chemotherapy; awareness of recommendations regarding the prevention and management of haemorrhagic and thromboembolic complications in association with various benign haematological disorders, including ITP, myeloproliferative disorders such as polycythaemia and high platelet levels and malignancies as well as haemostatic aspects of chemotherapeutic and immune modulatory/regulatory agents. 3.3.4 Nephrology haemostatic and thrombotic defects associated with chronic renal failure; anticoagulation in association with dialysis; Version 1.3 February 2010 9 use of antithrombotic and haemostatic agents in patients with renal failure; haemostatic aspects of renal transplantation. 3.3.5 Surgery prevention and treatment of venous thromboembolism; management of surgery in patients with congenital defects of haemostasis; management of invasive procedures for patients with abnormal coagulation tests and patients on anticoagulants; management of patients with intra or postoperative bleeding; pathophysiology and diagnosis of haemostatic alterations in trauma patients including patients with hypothermia, acidosis, dilution, massive transfusion and hypocalcaemia; treatment of bleeding in trauma patients and the use of red blood cell concentrates, platelets, fresh frozen plasma, activated rfVII, fibrinogen, antithrombin, PCCs and antifibrinolytics; 3.4 strategies for replacement therapy in trauma patients. Bleeding disorders Includes: platelet structure and function; mechanisms involved in primary haemostasis including platelet-vessel wall interactions; factors, interactions and mechanisms involved in plasma coagulation; components involved and the principles of fibrinolysis; natural inhibitors and their function; cellular interactions involved in the process of thrombosis and haemostasis; 3.4.1 Haemophilia A & B Includes: relevant and accurate personal and family bleeding history; focused clinical examination to assess for abnormal bleeding; formulate a comprehensive differential diagnosis and management plan. performance, interpretation and limitations of diagnostic methods including screening tests, specific factor and inhibitor assays; genetic counselling of patients with inherited bleeding disorders; structural and functional aspects of the biology of factor VIII (FVIII) and factor IX (FIX); history of haemophilia and the evolution of replacement therapy; an understanding of how haemophilia care is provided in different parts of the world and the difficulties of providing diagnostic and therapeutic services in some countries; Version 1.3 February 2010 10 epidemiology, classification and molecular basis of haemophilia A and B; genetic/molecular diagnosis, inheritance and genetic counselling; understanding of preimplantation genetic diagnosis (PGD); recognise clinical manifestations of haemophilia from early age to adulthood, especially in children, with a special focus on haemarthroses and haemophilic arthropathy, muscular haematomas, pseudotumours, Volkmann's syndrome and intracranial bleeding; performance and interpretation of laboratory testing including the use FVIII/FIX clotting activity, the original Bethesda assay as well as Nijmegen modification, concepts of 'global testing'; therapeutic options and delivery of replacement therapy in various clinical settings for both children and adults, including the principles of primary and secondary prophylaxis, on-demand therapy of bleeds and the use of replacement therapy in association with surgical procedures; drugs to use in the management of bleeds, surgical procedures and for prophylactic therapy (mechanisms of action, pharmacology, indications, dosing, precautions and management of overdosing) including DDAVP, plasma-derived FVIII/FIX concentrates, cryoprecipitate, recombinant FVIII/ IX concentrates, antifibrinolytics, sealant measures, fibrin glues; epidemiology, immunology and molecular basis of inhibitors to FVIII, or FIX, genetic and environmental risk factors in the development of inhibitors in patients with haemophilia A and B; diagnosis, classification and clinical management of inhibitors to FVIII and FIX, including knowledge of pharmacokinetics (recovery, half-life measurement); mechanisms of action, pharmacokinetics, indications, dosing, precautions and management of side-effects of by-passing agents, i.e. recombinant factor VIIa (rFVIIa), aPCC; dosing regimens for immune tolerance induction in patients with inhibitors, as well as in the use of immuno-suppressive drugs, apheresis, immunoadsorption; immune tolerance induction therapy (ITIR) in haemophilic patients with inhibitors to FVIII or FIX, including treatment of intercurrent bleeds, use of CVC, diagnosis and treatment of side effects such as nephrotic syndrome in haemophilia B patients; dental care and the follow-up of patients in collaboration with dentists; physiotherapy and outcome assessment of arthropathy in haemophilia patients; indications, limitations and potential complications of orthopaedic surgery including synoviorthesis and joint replacement; management of gynaecological and obstetric haemostatic complications in carriers of haemophilia A and B. 3.4.2 VWD Version 1.3 February 2010 11 structural and functional aspects of the biology of Von Willebrand Factor (VWF) including interactions with platelets, endothelium and FVIII; understanding of the incidence, inheritance, classification (including molecular and genetic aspects), clinical manifestations, natural history and complications of VWD; principles and interpretation of laboratory testing including the use of the PFA-100 and platelet aggregation, Ristocetin Cofactor Activity (VWF:RCo), VWF:Ag, FVIII:C, Collagen binding assay and vWF multimers; genetic and environmental factors influencing the VWF level; genetic counselling of patients with VWD; therapeutic options in the management of patients with VWD, including mechanism of action, pharmacokinetics, indications, dosing, precautions and management of overdosing; management of bleeding episodes and surgery of patients with VWD; dental care and prevention of complications of patients with VWD in collaboration with dentists; planning and outcome assessment of prophylactic treatment of patients with VWD; diagnosis, treatment and clinical management of patients with VWD and inhibitors, including knowledge of emergency treatment of subjects with anaphylactic reactions; 3.4.3 management of gynaecological and obstetric complications in females with VWD. Inherited platelet disorders Includes: disorders of platelet adhesion, including Bernard-Soulier syndrome; disorders of platelet aggregation, including Glanzmann thrombasthenia; disorders of platelet secretion and dense granule deficiency; disorders of platelet procoagulant activity; intrinsic disorders of platelet function in association with haematological disorders and other organ failure/malfunction; extrinsic platelet disorders associated with various haemostatic drugs, including aspirin, non-steroidal anti-inflammatory drugs (NSAID), ADP receptor antagonists, platelet GPIIb-IIIa antagonists, fibrinolytic agents and various foods; microangiopathic disorders/Thrombotic Thrombocytopenic purpura (TTP) and antiplatelet antibodies (ITP, SLE, alloimmunization). 3.4.5 Rare factor deficiencies pathophysiological mechanisms, incidence, inheritance, clinical manifestations and treatment of deficiencies of factor II, V, VII, X, XI, XIII, combined deficiency of FV + FVIII, combined deficiencies of vitamin K-dependent factors, a/dysfibrinogenaemia, and contact factor deficiencies;. Version 1.3 February 2010 12 principles of biological techniques for molecular diagnosis, and prenatal diagnosis in families with rare factor deficiencies; therapeutic options in the management of patients with rare factor deficiencies; indications, pharmacokinetics and dosing of different plasma-derived products usable in patients with rare factor deficiencies; management of bleeding episodes and surgery as well as aspects on dental care and prevention of complications in patients with rare factor deficiencies; principles of prophylactic replacement therapy for patients with rare factor deficiencies. 3.4.6 Acquired bleeding disorders antithrombotic drugs; vitamin K deficiency; liver disease; Disseminated Intravascular Coagulation (DIC); systemic fibrinolysis; massive blood transfusion; renal failure; malignancies; pregnancy and obstetrics; congenital heart disease and cardiac surgery; diagnostic aspects and clinical management of bleeds in association with: acquired coagulation factor inhibitors including acquired haemophilia, VWD and acquired inhibitors to other factors. special aspects on acquired haemophilia A including the characterization of FVIII inhibitors, the use of by-passing agents (rFVIIa and aPCC) and therapeutic options aiming to eradicate the inhibitor; non-accidental injury, especially in children, and how this is distinguished from those with a haemorrhagic disorder; vascular disorders including vasculitis, vascular malformation and structural disorders. 3.4.7 Plasma derived and recombinant therapeutic agents elimination methods of infectious agents: indications, limitations and potential complications of replacement with fresh-frozen plasma and cryoprecipitate; indications, limitations and potential complications of replacement with prothrombin complex concentrates (PCCs); indications, limitations and potential complications of replacement with highly purified Version 1.3 February 2010 13 plasma-derived molecules; indications, limitations and potential complications of replacement with highly purified recombinant molecules; immunologic complications associated with replacement of the missing clotting factor; indications, limitations and potential complications of replacement with bypassing agents (FEIBA and rVIIa). 4.0 Clinical trials Includes: Good Clinical Practice; Study design types and purposes of clinical trials; estimation of number of study subjects, obtaining ethical approval, recruitment of patients, patient information sheets and consent forms; data collection, statistical analysis and presentation of results. Version 1.3 February 2010 14 Appendices Example levels of competence in relation to local training programme and service needs, e.g. on call competency Level 1 Able to perform daily duties as an SpR with responsibility for haemostasis and thrombosis, including on-call competency Competencies in BOLD required before being on call Applies to all SpRs Competency Date achieved Consultant signature Introduction to department by haemostasis consultant Introduction to Thrombophilia & Anticoagulant Service by Nurse Specialist Introduction to Haemophilia Service by Nurse Specialist Knows how to use anticoagulant computerised decision support system software to review results (1 hr training) Uses protocols for reversal of INR > 5, > 8, or >20 Understands which blood samples are required for coagulation studies including INR Knows the methods used to monitor heparin and warfarin therapy Knows how to investigate a prolonged PT & APTT Is aware of the factor concentrate products available for use and where they are stored Knows how to issue factor concentrate to patients Has been trained in reconstitution and administration of factor concentrates (1 hr training) Has the ability to use the anticoagulant computerized decision support system software to dose and amend patient accounts. Able to advised on heparin bridging therapy Familiar with BCSH warfarin guideline Attendance in Anticoagulant clinic (8 hrs) Attendance in Thrombophilia clinic (8 hrs) Attendance in Womens clinic (8 hrs) Attendance in Haemophilia clinic (16 hrs) Attendance in Anticoagulant service (10 half days) Attendance in Haemophilia service (20 half days) Holder of Coagulation SpR bleep (2 weeks) Satisfactory performance in interactive problem solving reflecting curriculum (level 1) Level 1 COMPETENCY ASSESSMENT SATISFACTORY Version 1.3 February 2010 15 Level 2 Suggested required before enrollment for Part 1 FRCPath examination Competency Date achieved Consultant signature Confirmation of level 1 competencies and further development reflecting experience and reflective thinking Practical knowledge of standardised bleeding scores Understands methods required for investigation of bleeding Understands methods required for investigation of thrombosis & thrombophilia Moderate theoretical knowledge of coagulation system, including cascade model Understands principles and format of SOPs, IQC, EQA including working examples Familiarity with EQA reports Understands principles of pre-analytical variables in collection and preparation of samples Understands and can describe methods for PT, INR, APTT, TT, fibrinogen, factor assays, Bethesda assay, chromogenic assays, tests for LA, PFA-100, platelet aggregation, ELISAs Anticoagulant clinic (9 hrs) Thrombophilia clinic (6 hrs) Womens clinic (6 hrs) Haemophilia clinic (2 hrs) Anticoagulant service (28 half days) Haemophilia service (28 half days) Coagulation SpR bleep (8 weeks) Knows how to interrogate anticoagulant computerised decision support system for individual patient and cohort statistics e.g. Time in Range Able to perform manual PT, APTT, fibrinogen, factor VIII assays Understands and can describe specific methods for factor assays, AT, PC, PS, basic molecular tests (e.g. FVL) Familiar with general and specific competencies - sections 2 & 3 of programme as described Familiar with BCSH & UKHCDO guidelines Satisfactory performance in interactive problem solving reflecting curriculum (level 2) Level 2 COMPETENCY ASSESSMENT SATISFACTORY Version 1.3 February 2010 16 Level 3 Suggested required before enrollment for Part 2 FRCPath examination Competency Date achieved Consultant signature Confirmation of level 2 competencies and further development reflecting experience and reflective thinking Good working knowledge of coagulation system, including cascade model More advanced theoretical knowledge of coagulation system, including cell based model of haemostasis Able to perform automated PT, APTT, fibrinogen, factor assays and chromogenic assays Able to perform ELISA Able to perform PFA-100 analysis and platelet aggregation Understands classification of platelet disorders Aware of advanced methodology - ETP, TEG Working knowledge of general and specific competencies sections 2 & 3 of programme as described Experience of implementation of BCSH & UKHCDO guidelines Satisfactory performance in interactive problem solving reflecting curriculum (level 3) Level 3 COMPETENCY ASSESSMENT SATISFACTORY Version 1.3 February 2010 17 Level 4 Higher level of competence reflecting special interest in haemostasis and thrombosis recommended for SpRs with special interest in haemostasis & thrombosis, i.e. beyond FRCPath Competency Date achieved Consultant signature Confirmation of level 3 competencies and further development reflecting experience and reflective thinking Able to perform advanced assays, e.g. thrombin generation, thromboelastography Attended specialty meeting, e.g. BSHT, ISTH Understanding of research methodology and critical manuscript review Satisfactory performance in interactive problem solving reflecting curriculum (level 4) Level 4 COMPETENCY ASSESSMENT SATISFACTORY Version 1.3 February 2010