ch_20_Case Study_Answer_Key
advertisement
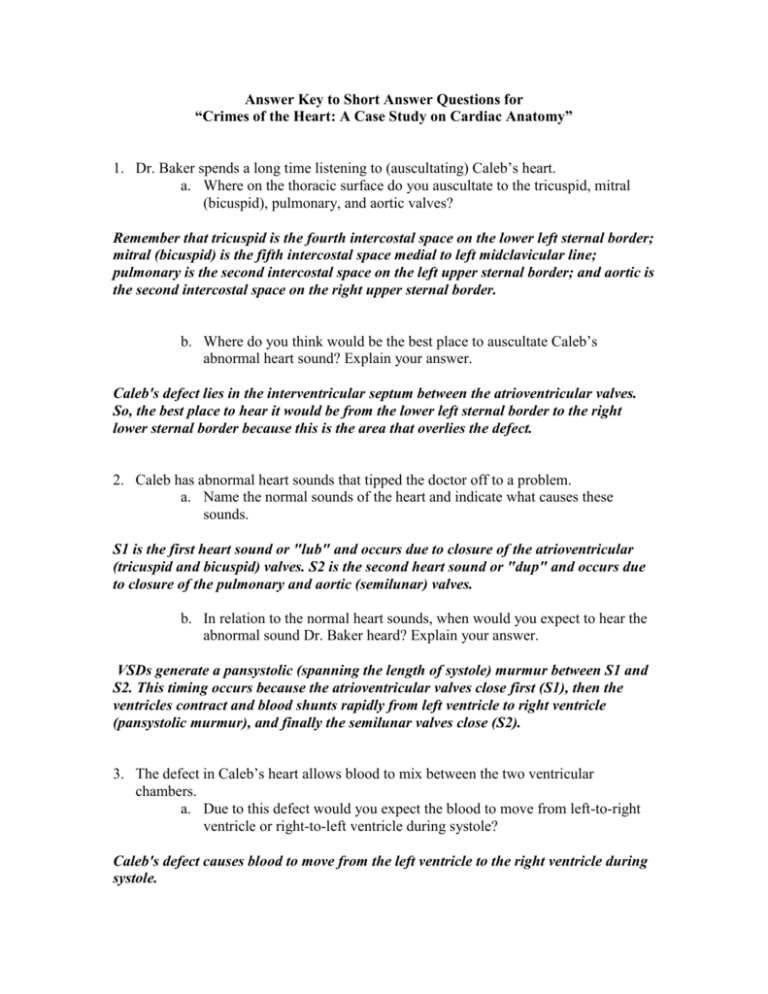
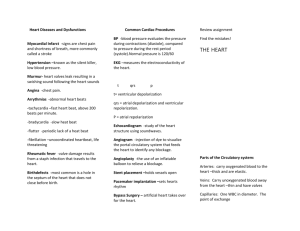
Answer Key to Short Answer Questions for “Crimes of the Heart: A Case Study on Cardiac Anatomy” 1. Dr. Baker spends a long time listening to (auscultating) Caleb’s heart. a. Where on the thoracic surface do you auscultate to the tricuspid, mitral (bicuspid), pulmonary, and aortic valves? Remember that tricuspid is the fourth intercostal space on the lower left sternal border; mitral (bicuspid) is the fifth intercostal space medial to left midclavicular line; pulmonary is the second intercostal space on the left upper sternal border; and aortic is the second intercostal space on the right upper sternal border. b. Where do you think would be the best place to auscultate Caleb’s abnormal heart sound? Explain your answer. Caleb's defect lies in the interventricular septum between the atrioventricular valves. So, the best place to hear it would be from the lower left sternal border to the right lower sternal border because this is the area that overlies the defect. 2. Caleb has abnormal heart sounds that tipped the doctor off to a problem. a. Name the normal sounds of the heart and indicate what causes these sounds. S1 is the first heart sound or "lub" and occurs due to closure of the atrioventricular (tricuspid and bicuspid) valves. S2 is the second heart sound or "dup" and occurs due to closure of the pulmonary and aortic (semilunar) valves. b. In relation to the normal heart sounds, when would you expect to hear the abnormal sound Dr. Baker heard? Explain your answer. VSDs generate a pansystolic (spanning the length of systole) murmur between S1 and S2. This timing occurs because the atrioventricular valves close first (S1), then the ventricles contract and blood shunts rapidly from left ventricle to right ventricle (pansystolic murmur), and finally the semilunar valves close (S2). 3. The defect in Caleb’s heart allows blood to mix between the two ventricular chambers. a. Due to this defect would you expect the blood to move from left-to-right ventricle or right-to-left ventricle during systole? Caleb's defect causes blood to move from the left ventricle to the right ventricle during systole. b. Based on your understanding of blood pressure and resistance in the heart and great vessels, explain your answer to question 3a. Blood moves into an open space where there is the least amount of resistance (pressure) or down its resistance (pressure) gradient. The blood pressure in the right ventricle is lower than the pressure in the left ventricle. This phenomenon occurs because the afterload in the right ventricle is lower than the afterload of the right ventricle. The difference between these afterloads is due to the pulmonary blood vessels generating less resistance when compared to the systemic blood vessels. 4. When an echocardiogram is performed, the technician color-codes oxygenated blood (red) and deoxygenated blood (blue). a. In a healthy baby, what color would the blood be within the right and left ventricles, respectively? The right ventricle has deoxygenated blood (blue). The left ventricle has oxygenated blood (red). b. In Caleb’s heart, what color would the blood be within the right and left ventricles, respectively? The right ventricle has both deoxygenated and oxygenated blood (both blue and red). (Note: In a real echocardiogram, this shows up as yellow/white.) The left ventricle has oxygenated blood (red). 5. Caleb’s heart allows oxygenated and deoxygenated blood to mix. Based on your knowledge of the heart and the great vessels, describe other anatomical abnormalities that cause the mixing of oxygenated and deoxygenated blood. Patent ductus arteriosus: Normally the ductus arteriosus, which connects the fetal pulmonary trunk to the aorta, closes very soon after birth. However, if it fails to close then it remains open, or patent. A patent ductus arteriosus allows a portion of the oxygenated blood from the aorta to flow back to the pulmonary trunk, where it mixes with deoxygenated blood that is sent to the lungs. Because of this, there is a significant increase in the volume of blood that goes to the lungs. Atrial Septal Defect (ASD): A hole in the wall between the two upper chambers is called an atrial septal defect, or ASD. Normally, systemic deoxygenated blood is carried by the superior and inferior vena cavae to the right atrium, and the left atrium receives oxygen-rich blood from the pulmonary veins. When a defect is present between the atria, some oxygen-rich blood leaks back to the right side of the heart. It then goes back to the lungs even though it is already rich in oxygen. Because of this, there is a significant increase in the volume of blood that goes to the lungs. 6. What happens to Caleb’s systemic cardiac output as a result of his ventricular septal defect (VSD)? Explain your answer. Due to a left-to-right blood shunt, the left ventricular volume falls during systole prior to the opening of the aortic valve. This shunt decreases stroke volume and cardiac output from the left ventricle into the aorta. 7. One of the problems that worried Tiffaney was that Caleb seemed to be breathing too hard all the time. Let’s consider how this symptom is related to his heart defect. a. Describe what would happen to the blood volume and pressure entering the pulmonary circuit as a result of his VSD. There is an increase in the total amount of blood pumped to the pulmonary trunk during each systole. Thus, the total pressure in these vessels also increases. (Note: This excessive volume/pressure, or pulmonary hypertension, causes pulmonary edema indicated by Caleb's increased work of breathing.) b. Describe what would happen to the myocardium of Caleb’s right ventricle as a result of his VSD. Due to the left-to-right shunt, the blood volume within the right ventricle increases. Due the volume overload, the right ventricle cannot effectively pump out blood, causing an increase in end systolic volume and stretching of the myocardium. The end result is an overall enlargement of the wall of the right ventricle called hypertrophy. 8. Based on the location of Caleb’s defect, what part of the conduction system might be at risk for abnormalities? The bundle of His (atrioventricular bundle) and the bundle branches are along the interventricular septum. So, if the defect included a large portion of the septum, all of these areas could be at risk for abnormalities. This would show up as a bundle branch block on an ECG rhythm strip. (Note: One way VSDs are classified is if they include the contractile myocardium, the conduction system, or both.)