14 - Ynet
advertisement

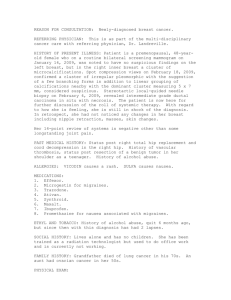
14.3 Licensed to Darya Levy ®UpToDate 2006© New Search Contents My UpToDate CME 96.8 Help A newer version of UpToDate is now available, and the information in this version may no longer be current. Official reprint from UpToDate® www.uptodate.com Drug-induced thrombosis and vascular disease in patients with malignancy Kenneth A Bauer, MD UpToDate performs a continuous review of over 350 journals and other resources. Updates are added as important new information is published. The literature review for version 14.3 is current through August 2006; this topic was last changed on August 16, 2006. The next version of UpToDate (15.1) will be released in February .2007 INTRODUCTION — Cancer is often associated with a state of hypercoagulability which can have a variety of clinical manifestations including migratory superficial thrombophlebitis, "unprovoked" deep vein and other venous thrombosis, nonbacterial thrombotic endocarditis, and disseminated intravascular coagulation. Deep vein thrombosis is the most common vascular toxicity of antineoplastic therapy. Intracranial dural sinus vein thrombosis and thrombotic microangiopathies can also be .)"seen. (See "Hypercoagulable disorders associated with malignancy This review will discuss vascular complications caused by the various .chemotherapeutic agents used in the treatment of patients with malignant disease MECHANISMS AND RISK FACTORS — The proposed mechanisms for the increased incidence of vascular complications in patients with malignancy include release or expression of procoagulants by tumor cells (eg, cancer procoagulant and tissue factor) and expression of procoagulant activity by normal host cells such as monocytes, platelets, and endothelial cells. (See "Pathogenesis of the hypercoagulable .)"state associated with malignancy In addition, the usual treatments for cancer also significantly increase the risk of thrombotic events. Surgery is a major precipitating factor, with the risk of postoperative thrombosis being several-fold higher than in patients without cancer. (See "Prevention of venous thromboembolic disease", section on Surgery in cancer patients). High dose chemotherapy and bone marrow transplantation for hematologic malignancies are associated with an enhanced risk of thrombosis, particularly hepatic veno-occlusive disease. (See "Pathogenesis and clinical features of hepatic venoocclusive disease following hematopoietic cell transplantation"). A number of chemotherapeutic regimens have been associated with an increased rate of thromboembolism [1]. Two of the regimens most commonly complicated by thrombosis are L-asparaginase, often given for acute lymphoblastic leukemia, and the administration of tamoxifen and other agents in the treatment of breast cancer (see below). The presence of an indwelling central venous catheter is a known risk factor for the development of upper extremity venous thrombosis in both adult and pediatric cancer patients. (See "Catheter-induced upper extremity venous thrombosis" and see "Pathogenesis and clinical manifestations of venous thromboembolism in infants and .)"children Disease- and patient-specific risk factors may also contribute to the risk of chemotherapy-associated venous thromboembolic disease. In a study of 3003 patients receiving at least one cycle of chemotherapy, symptomatic VTE occurred in 1.9 percent over a median follow-up of 2.4 months, or a rate of 0.8 percent/month [2]. The highest rates were seen in patients with upper gastrointestinal cancers, lung .cancer, and lymphoma, with rates of 2.3, 1.2, and 1.1 percent/month, respectively On multivariate analysis, the following factors were significantly associated with development of symptomatic VTE [2]: Upper gastrointestinal malignancy (odds ratio [OR] 3.9, 95% CI 1.4-10) Pre-chemotherapy platelet count 350,000/microL (OR 2.8, 95% CI 1.6-4.9) Use of white blood cell growth factors (eg, G-CSF, OR 2.1, 95% CI )1.2-3.6) Hemoglobin <10.0 g/dL or use of erythropoietin (OR 1.8, 95% CI 1.1-3.1 L-ASPARAGINASE — Thrombotic events have been reported with induction chemotherapy regimens for acute lymphoblastic leukemia (ALL) that include Lasparaginase. (See "Treatment of acute lymphoblastic leukemia in adults"). Intracranial dural sinus thrombosis with hemorrhage is observed most frequently, but deep venous thrombosis and pulmonary embolism can also occur [3-5]. In one large series of children receiving L-asparaginase as part of induction chemotherapy for ALL, the incidence of thrombotic complications was 1.2 percent [4]. Generalized .bleeding episodes have rarely been observed Asparaginase depletes plasma asparagine, thereby inhibiting protein synthesis in leukemic cells and the synthesis of many plasma proteins. The latter effect causes deficiencies of albumin, thyroxine-binding globulin, and various coagulation proteins, including prothrombin, factors V, VII, VIII, IX, X, XI, fibrinogen, antithrombin, protein C, protein S, and plasminogen [6-8]. This results in prolongation of the prothrombin time, activated partial thromboplastin time (aPTT), and thrombin time, and in hypofibrinogenemia with levels often less than 100 mg/dL. These coagulation .abnormalities resolve within one to two weeks after cessation of the drug It is difficult to assess the role of the substantial reductions in the levels of natural anticoagulant proteins such as antithrombin, protein C, and protein S in the pathogenesis of the thrombotic events. Both procoagulant and anticoagulant protein synthesis in the liver are decreased by L-asparaginase, leading to uncertainty as to whether there is an alteration in the balance of the opposing forces of the hemostatic .mechanism. Two mechanisms have been considered Antithrombin — There are data suggesting that antithrombin supplementation given concurrently with L-asparaginase may suppress the prothrombotic state [9-11]. However, a drug-induced decrease in antithrombin is not predictive of subsequent thrombosis. In one study of children with ALL receiving L-asparaginase, prednisone, and vincristine, no correlation was found between protein C, protein S, or .]antithrombin levels and the presence or absence of thrombosis [12 von Willebrand factor — Qualitatively abnormal von Willebrand factor (vWf) has been found in several patients at the time of L-asparaginase-induced thrombosis [13]. L-asparaginase may lead to a transient increase in unusually large plasma vWf .]multimers that have enhanced platelet agglutinating properties [13 Erwinia-asparaginase is an alternate preparation which may have fewer effects on the coagulation system than Escherichia coli L-asparaginase. In a series of 11 adults with ALL, there was significant lowering of antithrombin but the levels of the vitamin-K .]dependent procoagulant factors II, VII, and X, remained within normal ranges [14 TREATMENT OF BREAST CANCER — A number of large studies have found an increased incidence of thromboembolic events in women with breast cancer treated with chemotherapy, tamoxifen, or both. Additional risk factors may include postmenopausal status, prior mastectomy, increased body weight, presence of an .]indwelling central venous catheter, and evidence of coagulation activation [15 Chemotherapy — Studies of adjuvant chemotherapy for stage II breast cancer or primary chemotherapy for advanced, metastatic disease have shown a high incidence of thrombosis, both arterial and venous, during but not after chemotherapy. The risk is higher in patients with metastatic disease, which is probably due to the increased tumor burden and the increased incidence of other predisposing factors such as .immobilization Incidence — The incidence of thromboembolic disease following chemotherapy for breast cancer has varied widely in different reports, and appears to be related to the stage of the disease, the chemotherapeutic regimen given (eg, CAF versus CMF), and whether tamoxifen is given concurrently or following completion of chemotherapy (see "Tamoxifen and raloxifene" below). In a randomized study of early breast cancer, patients assigned to perioperative chemotherapy with fluorouracil, doxorubicin and cyclophosphamide had a higher incidence of thromboembolic events within six weeks after surgery than a control group treated with observation alone (2.1 versus 0.6 percent) [16]. In a Cancer and Leukemia Group B (CALGB) study, 433 patients were randomly assigned to receive one of three regimens based upon cyclophosphamide, methotrexate and 5-fluorouracil (CMF) as adjuvant therapy [17]. Thromboembolic disease occurred in 5 to 7 percent. There was no difference between the three groups. .No patient developed thrombosis after chemotherapy was completed A similar incidence (7 percent) was noted in a prospective study evaluated of 205 women with stage II breast cancer who were treated with one of two chemotherapy regimens: CMFVP (cyclophosphamide, methotrexate, fluorouracil, vincristine, and prednisone) or CMFVP plus doxorubicin and tamoxifen [18]. Once again, no thrombotic episodes occurred during 2413 patient months of follow-up without therapy. There was no relationship between the development of thrombosis and estrogen or progesterone receptor status, age, number of involved lymph nodes, or subsequent tumor recurrence. A higher risk of thrombosis (18 percent) was noted in a series of 159 patients treated with CMFVP for advanced, stage IV disease [19]. There were no differences in the presence of risk factors for thrombosis between the patients .who had a thromboembolic event and those who did not Although most patients develop venous thrombosis, there is also an association between arterial thrombosis and cancer therapy among women with breast cancer [20,21]. A CALGB study, for example, found a 1.3 percent incidence of arterial thrombosis, either peripheral or cerebrovascular, in 1014 patients during treatment for stage II or III breast cancer on two separate chemotherapy protocols [20]. All but one .of the thrombotic events occurred while patients were receiving chemotherapy Mechanism — The mechanism of the thrombogenic effects of chemotherapy in patients with breast cancer is not well understood. One report noted statistically significant decreases in protein C and protein S levels during CMF chemotherapy which, in some patients, fell below the range of values seen in hereditary thrombotic disorders [22]. Reductions in procoagulants factor VII and fibrinogen were also present and none of the patients in this small series had clinically evident thrombosis. In another report, there were significant declines in protein C concentration during CMF chemotherapy, which returned to baseline values after the completion of therapy .][23 Possible explanations for these chemotherapy-induced abnormalities include impairment of vitamin K metabolism and inhibition of DNA/RNA synthesis, leading to a reduction in protein synthesis by the liver. In addition, endothelial cell injury can lead to qualitative or quantitative abnormalities in vWf which may enhance the thrombotic potential. Other possible mechanisms include direct platelet activation, reduced fibrinolytic activity, and the release of procoagulant from tumor cells dying .as a result of antineoplastic therapy Attempts to identify patients at risk by monitoring with coagulation tests have not been successful. In a study of 50 patients treated with adjuvant epirubicin and cyclophosphamide chemotherapy, the incidence of deep vein thrombosis was 10 percent [24]. Preoperative levels of D-dimer, fibrinogen, and plasminogen activator inhibitor activity were significantly higher in the patients with breast cancer than in healthy women; however, monitoring during chemotherapy did not identify patients at .higher risk for deep vein thrombosis Tamoxifen and raloxifene — A number of studies, including the Early Breast Cancer Trialists' Collaborative Group (EBCTCG) overview analysis and the large Breast Cancer Prevention Trials, have demonstrated that tamoxifen use is associated with an increased rate of venous thromboembolic events and that there is a significant additional procoagulant effect when tamoxifen is added to chemotherapy [21,25-32]. In at least one randomized trial the incidence of VTE was lower when raloxifene was used in place of tamoxifen [33]. (See "Selective estrogen receptor modulators for the prevention of breast cancer" and see "Use of selective estrogen receptor modulators in postmenopausal women", section on Adverse effects and see "Adjuvant systemic therapy for hormone receptor positive early stage breast cancer in postmenopausal women"). In the NSABP P-1 Breast Cancer Prevention Study, which involved 13,388 women followed for an average of 3.6 years, the rates of pulmonary embolism and deep vein thrombosis were increased in older women receiving tamoxifen (risk ratio 3.0 [CI 1.1 to 11.2], and 1.6 [CI 0.9 to 2.9], respectively) [30]. In a subsequent pooled analysis of 13 NSABP Breast Cancer Prevention trials, which involved 20,878 women, the risk of pulmonary embolism, deep venous thrombosis, and superficial phlebitis was increased two- to threefold in those treated with tamoxifen and was increased 11- to 15-fold in those treated with tamoxifen plus chemotherapy [31]. Risk factors included increased age and body mass index; there were no differences in the rates of thrombosis between African Americans and white women in this study. In the five-year, randomized, double-blind, placebo-controlled International Breast Cancer Intervention Study (IBIS-1), involving 7,139 patients, use of tamoxifen was associated with an increased risk of developing a major venous thromboembolic event (odds ratio 2.1, 95% CI: 1.1-4.1) [34]. This risk was further increased in those patients who had surgery, immobilization, or fracture in the month prior to the event (odds ratio 4.7, 95% CI: 2.2-10.1). Factor V Leiden and prothrombin mutations were not associated with thrombosis in this population or in subjects participating in the National Surgical Adjuvant Breast and Bowel Project's Breast Cancer Prevention .]Project (BCPT) [35 The possibility that tamoxifen may be associated with an increased incidence of stroke was raised in two NSABP randomized trials: P-1 and NSABP B-24, a trial of tamoxifen for intraductal breast cancer. However, the available data are conflicting: In the EBCTCG overview analysis of approximately 15,000 women randomized to five years of tamoxifen or control, there was a trend toward increased stroke-related mortality that did not reach the level of statistical significance (54 versus 29 deaths, p = 0.07) [32]. Tamoxifen use was not associated with higher stroke risk in a retrospective nested case control study of 11,045 women enrolled in a large HMO in the Los Angeles area who were diagnosed with breast cancer between 1980 and 2000 [36]. When 179 who met the criteria for stroke were compared to 358 age and year of diagnosis-matched controls who had breast cancer but not stroke, there was no association between tamoxifen and stroke risk. In a systematic review of randomized controlled trials of tamoxifen use for breast cancer management and prevention published since 1980, the frequency of ischemic stroke during a mean follow-up period of 4.9 years was 0.71 percent with tamoxifen versus 0.39 percent for controls [37]. It was concluded that, although the absolute risk of stroke was small, women with breast cancer who were treated with tamoxifen had an increased risk for ischemic stroke (odds ratio 1.82, 95% CI 1.4-2.4) or any stroke (odds ratio 1.40, 95% .)CI 1.1-1.7 On the other hand, the increased risks of pulmonary embolus and stroke may be partially offset by a decreased risk of ischemic heart disease. In a case control study of women being treated with tamoxifen for breast cancer, there was a significant decrease in the incidence of first myocardial infarction or developing angina pectoris compared with cancer patients not being treated with tamoxifen (odds ratio 0.4, 95% CI 0.2-0.7) [38]. This beneficial effect may be due to the favorable effect of .tamoxifen on lipid profiles Mechanism — The potential mechanisms for the tamoxifen procoagulant effect have not been identified. Tamoxifen is an antiestrogen that has weak estrogenic effects which may contribute to its prothrombotic activity. A number of studies have evaluated measurements of hemostasis in patients taking tamoxifen. The results have been conflicting and no major changes have been identified [39-42]. Some reports have found modest reductions in antithrombin and protein C [39,40], while a prospective double-blind study was unable to find consistent tamoxifen-induced .]changes in protein S or protein C activity [42 Other agents — Aromatase inhibitors are being used as adjuvant hormonal treatment as an alternative to tamoxifen. The incidence of thromboembolic complications with anastrozole was significantly lower than with tamoxifen in the ATAC trial comparing these two agents. (See "Adjuvant systemic therapy for hormone receptor positive early stage breast cancer in postmenopausal women" section on AIs versus .)"tamoxifen Second-line hormonal therapy for patients with advanced breast cancer who fail tamoxifen includes the aromatase inhibitor formestane and the progestational agent megestrol. In a phase III prospective randomized crossover trial, the two drugs showed similar antineoplastic activity but the incidence of deep vein thrombosis was significantly higher with megestrol than formestane (five in 81 patients versus 0 in 90 .]patients) [43 Prophylactic anticoagulation — Long-term anticoagulant therapy with low-intensity warfarin may be a safe and effective method for prevention of thromboembolism in patients with metastatic breast cancer who are receiving chemotherapy. In a prospective, double blind study, for example, 311 patients with stage IV breast cancer received either placebo or warfarin (1 mg PO daily for six weeks which was then adjusted to maintain an INR of 1.3 to 1.9) [44]. Treatment was continued until one week after the end of chemotherapy which lasted approximately six months. There were seven thromboembolic events in the placebo group and one in the warfarin group (4.4 versus 0.7 percent), a relative risk reduction of 85 percent. Major bleeding .occurred in three patients, two of whom received placebo The benefit was achieved without an increase in health care costs [45]. The cost of providing low-intensity warfarin was calculated at $219 (Canadian dollars) per patient but therapy led to a reduction in costs of $243 per patient, producing a small cost .saving In a separate study, the effect of low-intensity warfarin on markers of hypercoagulation was evaluated in a randomized trial of 32 patients with metastatic breast cancer who were undergoing chemotherapy [46]. Before therapy, markers of clotting activation were increased in both groups, consistent with the presence of a hypercoagulable state. After starting chemotherapy, markers were progressively lower in the group receiving warfarin prophylaxis. These differences became statistically significant after the fourth course of chemotherapy. Deep vein thrombosis occurred in two of the 16 patients receiving placebo and in none of the 16 patients receiving very.low-dose warfarin TREATMENT OF TESTICULAR CANCER — Major cardiovascular issues that have been studied in connection with treatment for testicular cancer include hypertension, dyslipidemia, early atherosclerosis and coronary artery disease, Raynaud phenomenon, and thromboembolic events. These are discussed in detail separately. (See "Chemotherapy-related toxicity in men with testicular germ cell .)tumors", section on Cardiovascular and see "Miscellaneous" below THROMBOTIC MICROANGIOPATHY — Thrombotic microangiopathies have been associated with a number of cancer chemotherapeutic agents. This primarily occurs with one of four regimens: mitomycin C; cisplatin with or without bleomycin; gemcitabine; and the use of radiation and high dose chemotherapy prior to hematopoietic cell transplantation (HCT). (See "Causes of thrombotic thrombocytopenic purpura-hemolytic uremic syndrome in adults", section on Cancer, .)cancer chemotherapy, and HCT The syndrome more closely resembles the hemolytic-uremic syndrome (HUS) than thrombotic thrombocytopenic purpura (TTP) and usually develops within weeks to months after exposure to the drug. Detection may be delayed because chemotherapy can produce thrombocytopenia due to bone marrow depression and renal disease, thereby masking the presence of HUS. Affected patients typically present with slowly progressive renal failure, new or exacerbated hypertension, and a relatively bland .urine sediment, often occurring in the absence of clinically apparent tumor Drug-related endothelial injury is presumed to be the initiating event. It has been proposed that vWf multimers derived from damaged or stimulated endothelial cells may be involved in the pathogenesis of intravascular platelet clumping. However, there are conflicting data on the role of vWf multimers in patients with drug-induced thrombotic microangiopathies. In one study, vWf multimeric patterns were normal during episodes of mitomycin C-induced microangiopathy [47]. However, another report using a superior technique for detection of multimers found abnormalities in vWf in five of six patients [48]. The sixth patient had a three fold elevation in the .levels of vWf antigen MISCELLANEOUS — A variety of other drugs that can be used in patients with malignancy can be associated with thromboembolic events: High doses of estrogens increase the plasma concentrations of clotting factors and the risk of thrombotic disease [49]. Estrogenic prothrombotic effects are believed to be responsible for the dose-related cardiovascular complications of the estrogen analogue diethylstilbestrol (DES) in the treatment of prostate cancer [50]. In comparison, the lower doses used for hormone replacement therapy or oral contraception are associated with only a small increase in thrombotic risk. (See "Postmenopausal hormone therapy and cardiovascular risk", section on Venous thromboembolism). Dacarbazine, alone or in combination with other drugs has been associated with the Budd-Chiari syndrome [51]. In addition, veno-occlusive disease of the liver has been reported in patients with acute myelocytic leukemia who were treated with thioguanine and daunomycin with or without cytarabine [52,53]. Arterial ischemia or thrombosis in major coronary or cerebral vessels and in the small vessels of the extremities can be induced by chemotherapy. Various combinations of bleomycin, cisplatin and vinblastine are associated with myocardial infarction and stroke [51,54,55]. In one study, for example, cisplatin-based multiagent chemotherapy for urothelial transitional cell carcinoma was associated with a 13 percent risk of vascular events (venous thromboembolism, arterial thromboses, and cerebrovascular events), most of which occurred during the first two cycles of chemotherapy [55]. In another prospective series of 108 patients treated with cisplatin and gemcitabine for non-small cell lung cancer, 19 had significant vascular events, including seven with lower extremity arterial thrombosis [56]. (See "Neurologic complications of cancer chemotherapy"). An increased incidence of arterial thrombosis has been associated with the monoclonal antibody, bevacizumab, in patients with colorectal cancer, who are being treated concurrently with systemic chemotherapy. (See "Systemic chemotherapy for .)metastatic colorectal cancer" section on Bevacizumab Cardiac toxicity occurs in 1.6 to 2.3 percent of patients treated with 5-fluorouracil [57], and myocardial ischemia and stroke occur in up to 10 percent of patients who receive continuous infusions of the drug [58]. Induction of coronary spasm is the presumed mechanism [57]. (See "Cardiotoxicity of nonanthracycline cancer chemotherapy agents"). The use of cisplatin-bleomycin regimens for testicular cancer has been associated with Raynaud's phenomenon in up to 40 percent of patients [5961]. Vasospasm presenting as painful digits and paresthesias typically occurs 10 months after starting therapy and lasts indefinitely. The cumulative dose of bleomycin appears to be the major risk factor [61]. Raynaud's phenomenon associated with bleomycin and vinca alkaloids also occurs in patients with AIDS-related Kaposi's sarcoma [62,63]. (See "Chemotherapy-related toxicity in men with testicular germ cell tumors", section on Cardiovascular). Thrombosis has been noted in a significant percentage of patients with multiple myeloma treated with thalidomide and lenalidomide, most often in combination with other agents (eg, dexamethasone, doxorubicin). This subject is discussed separately. (See "Thrombotic complications .)"following treatment with thalidomide and its analogues Use of UpToDate is subject to the Subscription and License Agreement. REFERENCES 1. Otten, HM, Mathijssen, J, ten Cate, H, et al. Symptomatic venous thromboembolism in cancer patients treated with chemotherapy: an underestimated .phenomenon. Arch Intern Med 2004; 164:190 Khorana, AA, Francis, CW, Culakova, E, Lyman, GH. Risk factors for .2 chemotherapy-associated venous thromboembolism in a prospective observational .study. Cancer 2005; 104:2822 Priest, JR, Ramsay, NKC, Latchaw, RE, et al. Thrombotic and hemorrhagic strokes .3 complicating early therapy for childhood acute lymphoblastic leukemia. Cancer 1980; .46:1548 Priest, JR, Ramsay, NKC, Steinherz, PG, et al. A syndrome of thrombosis and .4 hemorrhage complicating L-asparaginase therapy for childhood acute lymphoblastic .leukemia. J Pediatr 1982; 100:984 Steinherz, PG, Miller, LP, Ghavimi, F, et al. Dural sinus thrombosis in children .5 .with acute lymphoblastic leukemia. JAMA 1981; 246:2837 Bezeaud, A, Drouet, L, Leverger, G, et al. Effect of L-asparaginase therapy for .6 acute lymphoblastic leukemia on plasma vitamin K-dependent coagulation factors and .inhibitors. J Pediatr 1986; 108:698 Buchanan, GR, Holtkamp, CA. Reduced antithrombin III levels during L- .7 .asparaginase therapy. Med Pediatr Oncol 1980; 8:7 Conard, J, Horellou, MH, Van Dreden, P, et al. Decrease in protein C in L- .8 .asparaginase-treated patients. Br J Haematol 1985; 59:725 Gugliotta, L, D'Angelo, A, Mattioli Belmonte, M, et al. Hypercoagulability during .9 L-asparaginase treatment: the effect of antithrombin III supplementation in vivo. Br J .Haematol 1990; 74:465 Mazzucconi, MG, Gugliotta, L, Leone, G, et al. Antithrombin III infusion .10 suppresses the hypercoagulable state in adult acute lymphoblastic leukemia patients treated with a low dose of Escherichia coli L-asparaginase. A GIMEMA study. Blood .Coagul Fibrinolysis 1994; 5:23 Mitchell, L, et al. Trend to efficacy and safety using antithrombin concentrate in .11 prevention of thrombosis in children receiving l-asparaginase for acute lymphoblastic .leukemia. Results of the PAARKA study. Thromb Haemost 2003; 90:235 Pui, CH, Chesney, CM, Bergum, PW, et al. Lack of pathogenic role of protein C .12 and S in thrombosis associated with asparaginase-prednisone-vincristine therapy for .leukemia. Br J Haematol 1986; 64:283 Pui, CH, Jackson, CW, Chesney, CM, et al. Involvement of von Willebrand factor .13 in thrombosis following asparaginase-prednisone-vincristine therapy for acute .leukemia. Am J Hematol 1987; 25:291 Carlsson, H, Stockelberg, D, Tengborn, L, et al. Effects of Erwinia-asparaginase .14 .on the coagulation system. Eur J Haematol 1995; 55:289 Caine, GJ, Stonelake, PS, Rea, D, Lip, GY. Coagulopathic complications in breast .15 .cancer. Cancer 2003; 98:1578 Clahsen, PC, van de Velde, CJ, Julien, JP, et al. Thromboembolic complications .16 after perioperative chemotherapy in women with early breast cancer: A European Organization for Research and Treatment of Cancer Breast Cancer Cooperative Group .study. J Clin Oncol 1994; 12:1266 Weiss, RB, Tormey, DC, Holland, JF, et al. Venous thrombosis during .17 .multimodal treatment of primary breast carcinoma. Cancer Treat Rep 1981; 65:677 Levine, MN, Gent, M, Hirsh, J, et al. The thrombogenic effect of anticancer drug .18 .therapy in women with stage II breast cancer. N Engl J Med 1988; 318:404 Goodnough, LT, Saito, H, Manni, A, et al. Increased incidence of .19 thromboembolism in stage IV breast cancer treated with a five-drug chemotherapy .regimen. A study of 159 patients. Cancer 1984; 54:1264 Wall, G, Weiss, RB, Norton, L, et al. Arterial thrombosis associated with adjuvant .20 chemotherapy for breast carcinoma: a Cancer and Leukemia Group B study. Am J .Med 1989; 87:501 Saphner, T, Tormey, DC, Gray, R. Venous and arterial thrombosis in patients who .21 .received adjuvant therapy for breast cancer. J Clin Oncol 1991; 9:286 Rogers, JS II, Murgo, AJ, Fontana, JA, et al. Chemotherapy for breast cancer .22 .decreases plasma protein C and protein S. J Clin Oncol 1988; 6:276 Feffer, SE, Carmosino, LS, Fox, RL. Acquired protein C deficiency in patients .23 with breast cancer receiving cyclophosphamide, methotrexate, and 5-fluorouracil. .Cancer 1989; 63:1303 von Tempelhoff, GF, Dietrich, M, Hommel, G, et al. Blood coagulation during .24 adjuvant epirubicin/cyclophosphamide chemotherapy in patients with primary .operable breast cancer. J Clin Oncol 1996; 14:2560 Rutqvist, LE, Mattson, A. Cardiac and thromboembolic morbidity among .25 postmenopausal women with early stage breast cancer in a randomized trial of .adjuvant tamoxifen. J Natl Cancer Inst 1993; 85:1398 McDonald, CC, Alexander, FE, Whyte, BW, et al. Cardiac and vascular morbidity .26 in women receiving adjuvant tamoxifen for breast cancer in a randomised trial. The .Scottish Cancer Trials Breast Group. BMJ 1995; 311:977 Pritchard, KI, Paterson, AH, Pauol, NA, et al. Increased thromboembolic .27 complications with concurrent tamoxifen and chemotherapy in a randomized trial of adjuvant therapy for women with breast cancer. National Cancer Institute of Canada .Clinical Trials Group Breast Cancer Site Group. J Clin Oncol 1996; 14:2731 Meier, CR, Jick, H. Tamoxifen and risk of idiopathic venous thromboembolism. .28 .Br J Clin Pharmacol 1998; 45:608 Fogarty, PF, Rick, ME, Swain, SM. Tamoxifen and thrombosis: Current clinical .29 observations and guidelines. Principles and Practice of Oncology Updates 2002; .16(2):1 Fisher, B, Constantino, JP, Wickerham, DL, et al. Tamoxifen for prevention of .30 breast cancer with tamoxifen: Report of the National Surgical Adjuvant Breast and .Bowel Project P-1 Study. J Natl Cancer Inst 1998; 90:1371 McCaskill-Stevens, W, Wilson, J, Bryant, J, et al. Contralateral breast cancer and .31 thromboembolic events in African American women treated with tamoxifen. J Natl .Cancer Inst 2004; 96:1762 Effects of chemotherapy and hormonal therapy for early breast cancer on .32 recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005; .365:1687 Vogel, VG, Constantino, JP, Wickerham, DL, et al. Effects of tamoxifen vs .33 raloxifene on the risk of developing invasive breast cancer and other disease .outcomes. JAMA 2006; 295:2727 Duggan, C, Marriott, K, Edwards, R, Cuzick, J. Inherited and acquired risk factors .34 for venous thromboembolic disease among women taking tamoxifen to prevent breast .cancer. J Clin Oncol 2003; 21:3588 Abramson, N, Costantino, JP, Garber, JE, et al. Effect of Factor V Leiden and .35 prothrombin G20210-->A mutations on thromboembolic risk in the national surgical adjuvant breast and bowel project breast cancer prevention trial. J Natl Cancer Inst .2006; 98:904 Geiger, AM, Fischberg, GM, Chen, W, Bernstein, L. Stroke risk and tamoxifen .36 .therapy for breast cancer. J Natl Cancer Inst 2004; 96:1528 Bushnell, CD, Goldstein, LB. Risk of ischemic stroke with tamoxifen treatment .37 .for breast cancer: a meta-analysis. Neurology 2004; 63:1230 Bradbury, BD, Lash, TL, Kaye, JA, Jick, SS. Tamoxifen-treated breast carcinoma .38 patients and the risk of acute myocardial infarction and newly-diagnosed angina. .Cancer 2005; 103:1114 Mannucci, PM, Bettega, D, Chantarangkul, V, et al. Effect of tamoxifen on .39 .measurements of hemostasis in healthy women. Arch Intern Med 1996; 156:1806 Pemberton, KD, Melissari, E, Kakkar, VV. The influence of tamoxifen in vivo on .40 the main natural anticoagulants and fibrinolysis. Blood Coagul Fibrinolysis 1993; .4:935 Jordan, VC, Fritz, NF, Tormey, DC. Long-term adjuvant therapy with tamoxifen. .41 Effects on sex hormone binding globulin and antithrombin III. Cancer Res 1987; .47:4517 Mamby, CC, Love, RR, Feyzi, JM. Protein S and protein C level changes with .42 adjuvant tamoxifen therapy in postmenopausal women. Breast Cancer Res Treat .1994; 30:311 Thurlimann, B, Castiglione, M, Hsu-Schmitz, SF, et al. Formestane versus .43 megestrol acetate in postmenopausal breast cancer patients after failure of tamoxifen: A phase III prospective randomised cross over trial of second-line hormonal treatment (SAKK 20/90). Swiss Group for Clinical Cancer Research. Eur J Cancer 1997; .33:1017 Levine, M, Hirsh, J, Gent, M, et al. Double-blind randomised trial of a very-low .44 dose warfarin for prevention of thromboembolism in stage IV breast cancer. Lancet .1994; 343:886 Rajan, R, Gafni, A, Levine, M, et al. Very low-dose warfarin prophylaxis to .45 prevent thromboembolism in women with metastatic breast cancer receiving .chemotherapy: An economic evaluation. J Clin Oncol 1995; 13:42 Falanga, A, Levine, MN, Consonni, R, et al. The effects of very-low-dose .46 warfarin on markers of hypercoagulation in metastatic breast cancer: Results from a .randomized trial. Thromb Haemost 1998; 79:23 Monteagudo, J, Pereira, A, Roig, S, et al. Investigation of plasma von Willebrand .47 factor and circulating platelet aggregating activity in mitomycin C-related hemolytic.uremic syndrome. Am J Hematol 1990; 33:46 Charba, D, Moake, JL, Harris, MA, Hester, JP. Abnormalities of von Willebrand .48 factor multimers in drug associated thrombotic microangiopathies. Am J Hematol .1993; 42:268 .Baird, DT, Glasier, AF. Hormonal contraception. N Engl J Med 1993; 328:1543 .49 Blackard, CE. The Veterans Administration Cooperative Urologic Research .50 Group studies of carcinoma of the prostate. A review. Cancer Chemother Rep 1975; .59:225 Luzzatto, G, Schafer, AI. The prethrombotic state in cancer. Semin Oncol 1990; .51 .17:147 D'Cruz, CA, Wimmer, RS, Harcke, HT, et al. Veno-occlusive disease of the liver .52 in children following chemotherapy for acute myelocytic leukemia. Cancer 1983; .52:1803 Gill, RA, Onstad, GR, Cardamone, JM, et al. Hepatic veno-occlusive disease .53 .caused by 6-thioguanine. Ann Intern Med 1982; 96:58 Doll, DC, List, AF, Greco, FA, et al. Acute arterial ischemic events following .54 cisplatin-based combination chemotherapy for germ cell tumors of the testis. Ann .Intern Med 1986; 105:48 Czaykowski, PM, Moore, MJ, Tannock, IF. High risk of vascular events in .55 patients with urothelial transitional cell carcinoma treated with cisplatin based .chemotherapy. J Urol 1998; 160:2021 Numico, G, Garrone, O, Dongiovanni, V, et al. Prospective evaluation of major .56 vascular events in patients with nonsmall cell lung carcinoma treated with cisplatin .and gemcitabine. Cancer 2005; 103:994 .Anand, AJ. Fluorouracil cardiotoxicity. Ann Pharmacother 1994; 28:374 .57 Robben, NC, Pippas, AW, Moore, JO. The syndrome of 5-fluorouracil .58 .cardiotoxicity: An elusive cardiopathy. Cancer 1993; 71:493 Vogelzang, NJ, Torkelson, JL, Kennedy, BJ. Hypomagnesemia, renal dysfunction .59 and Raynaud's phenomenon in patients treated with cisplatin, vinblastine and .bleomycin. Cancer 1985; 56:2765 Hansen, SW, Olsen, N, Rossing, N, Rorth, M. Vascular toxicity and the .60 mechanism underlying Raynaud's phenomenon in patients treated with cisplatin, .vinblastine and bleomycin. Ann Oncol 1990; 1:289 Berger, CC, Bokemeyer, C, Schneider, M, et al. Secondary Raynaud's .61 phenomenon and other late vascular complications following chemotherapy for .testicular cancer. Eur J Cancer 1995; 31A:2229 Reiser, M, Bruns, C, Hartmann, P, et al. Raynaud's phenomenon and acral .62 necrosis after chemotherapy for AIDS-related Kaposi's sarcoma. Eur J Clin Microbiol .Infect Dis 1998; 17:58 Hladunewich, M, Sawka, C, Fam, A, et al. Raynaud's phenomenon and digital .63 gangrene as a consequence of treatment for Kaposi's sarcoma. J Rheumatol 1997; .24:2371 New Search Contents My UpToDate CME 96.8 Help UpToDate® • www.uptodate.com • Contact Us 2006©