Rheumatoid Arthritis Case Study: Questions & Answers
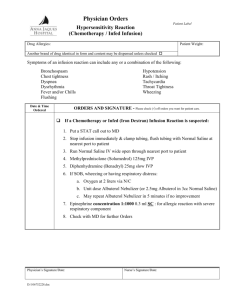
advertisement

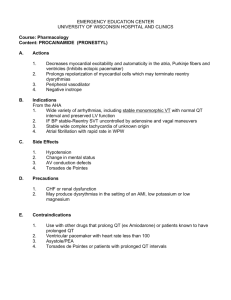
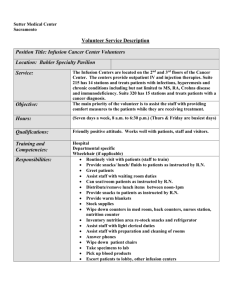
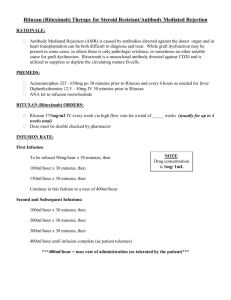
Rheumatoid Arthritis Case Study Questions & Answers Slide 5: What is significant about this report that leads you to RA? Pain in hands bilaterally, stiffness, tenderness in the morning, poor appetite and easily fatigued RA affects women > men and is most common 40-60 yrs old What additional nursing assessment data would be significant? Joints spongy feeling, warm/hot, swollen, not easily moved, fever, weight loss, Raynaud’s phenomenon (cold & stress induced vasospasms that cause white/cyanotic coloring Slide 7: Patient has mild OA and is now being diagnosed with RA, explain the differences to her. RA is typically symmetrical OA is not RA targets smaller joints first and OA tends to affect larger joints first RA is synovitis of the joints (inflammation of the synovial lining), OA is “wear & tear” breakdown of cartilage OA is more common RA is more debilitating & crippling RA is autoimmune, systemic RA is remissions & exacerbations Morning stiffness is < 30 mins in OA and > 1 hour in RA Slide 10: How will these laboratory values be affected or how will they assist in the diagnosis of RA? RBC & HcT are decreased – chronic inflammation CRP – elevated indicates active inflammation (Normal is less than 1 mg/dL) ESR – elevated indicates inflammatory process (Normal is 0-15 Men, 0-25 Women) RF – Positive in 80% of RA patients , not a specific indicator of RA ACPA – Positive can indicate RA, not a specific indicator of RA Synovial Fluid – cloudy with increased leukocytes present Xray – narrowed joint spaces, not typically seen in the first 3-6 months, also done to determine progression Slide 12: According to the American College of Rheumatology what are the 4 sets of data to classify RA? Joint involvement - number & small or large joint Serology - RF & ACPA Acute phase reactants - CRP & ESR Duration of symptoms - less than or greater than 6 weeks Explain what these 2 classes of medications are & how they work? NSAID (Nonsteroidal Antiinflammatory Drug) – reduce inflammation to decrease pain, swelling, improve function. Do not affect the disease process. GI side effects – dyspepsia, ulcers, cardiovascular risks. See results quicker DMARD (Disease Modifying Antirheumatic Drug) – have potential to decrease joint damage, slow progression of disease, preserve joint function, should be started with 3 months of diagnosis. Cause immunosuppression. Slower onset on action. Why is PT/OT involved so early on when there isn’t a current mobility problem? To help preserve joint function; teach the patient ways to decrease stress on joints; ROM; muscle strengthening; teach appropriate exercises What additional teaching should be completed at this time?? This is a chronic progressive disease that can affect other organs and it can impact all areas of life; how to deal with pain, fatigue, and depression that can occur; importance of treatment compliance and follow-up; this disease cannot be cured – but treatment can be very effective; What are examples of NSAIDS & DMARDS that could be used at this time? NSAIDS – naproxen (Naprosyn), ibuprofen (Motrin), celecoxib (Celebrex), meloxicam (Mobic), Diclofenac (Voltaren) DMARDS – hydoxychloroquine (Plaquenil), leflunomide (Arava), methotrexate (Rheumatrex), sulfasalazine (Azulfidine), abatacept (Orencia), rituximab (Rituxan), etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira) Slide 14: Prior to starting this treatment plan what should be evaluated? Cardiovascular risk factors, liver enzymes, CBC, creatinine, pregnancy status, history of GI bleeding, presence of infection What patient teaching is indicated for these medications? Have student’s role play patient teaching Labs – Liver enzymes, Immunizations should be administered prior to DMARD therapy, watch for signs of GI bleeding, watch for signs of infection, compliance with follow-up labs is essential, Methotrexate needs to be taken exactly as presecribed (weekly in this case), take on empty stomach Celebrex – take with food When would these medications be contraindicated? Pregnancy, significant cardiac risk factors or hepatic or renal impairment Slide 15: Appropriate nursing diagnoses include: Acute or chronic pain Fatigue Imbalanced nutrition: less than body requirements Sleep deprivation Activity intolerance Impaired physical mobility Self-care deficit Disturbed body image Ineffective coping Fear Anxiety Powerlessness Risk for infection related to treatment methods Knowledge deficit: disease process or treatment Slide 18: What new patient teaching should be included? Humira: Avoid live vaccines while taking it Prior to giving it TB screening should be completed Serious infections can occur Teach self administration – it is a subcutaneous injection (abdomen, rotate sites, needle care/disposal) It should be kept refrigerated Slide 20: What information should be taught to Mrs. About the use/administration of Remicade? It is given via IV infusion over at least a 2 hour period, then repeat in 2 weeks, then at 6 weeks, then every 8 weeks If she is going to continue to get Remicade regularly a central line (port-a-cath) could be beneficial for her Monitor for infusion related reaction during and for 2 hours after infusion (reactions are more common after 1st or 2nd infusion) Monitor for symptoms of systemic infections/fungal infections TB skin test prior to beginning therapy Monitor for reactions Monitor liver function Monitor CBC (leukopenia, neutropenia, thrombocytopenia, pancytopenia) Slide 22: What should the nurse monitor for during the initial infusion in regards to a reaction? Fever Chills Itching Rash Dyspnea Hypotension/Hypertension Chest pain Both during and for 2 hours following the infusion If she were to have a reaction what should the nurse do? Stop the infusion Call the MD Prepare to administer antihistamines, corticosteroids, acetaminophen, and/or epinephrine Slide 24: What are some common signs of disease progression? And extra articular signs of RA? To view photos of these deformities please visit http://images.rheumatology.org Swan neck deformities Rheumatoid nodules Boutonniere’s deformity Ulnar deformity Hallux toes Raynaud’s phenomenon – cold or stress induced vasospasm causing white/blue coloring of fingers Sjogren’s syndrome – dry eyes & mucous membranes Increased risk for cardiac disease (vasculitis, pericarditis)