BURNS - Tripod.com
advertisement

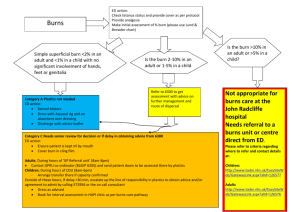
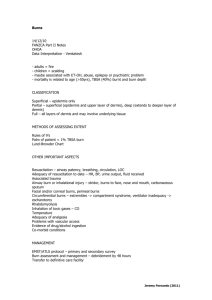
BURNS INTRODUCTION Burns are caused by application of heat to the body May be thermal -(flame, flash , contact, scald), chemical, electrical or radiation Usually accidental but may be predisposed by disease as in epilepsy 10% of admissions to Paediatric Surgery at MNH due to burns, mostly domestic accidents Injury is proportional to intensity and duration of exposure and tissue conductivity PATHOPHYSIOLOGICAL CHANGES Burn injury causes loss of epithelium and mediates systemic inflammatory response Results in generalized increase in microvascular permeability in burns >15% Maximal at16-24 hours Results in loss of protein rich exudate and oedema in unburned tissue Impaired cell membrane function with increase in ICF (>Na, <K) Initial hypodynamic state , decreased cardiac output, and increase in peripheral resistance At 2-3 days, hyperdynamic state with increased CO and low PVR Hypermetabolism beginning at 48 hours with x2 increased caloric needs Increased O2 consumption, heat production, hypoprotenaemia Due to catabolism, exudate, gluconeogenesis Loss of natural skin barrier and altered immunological function Associated with depressed cell mediated and humoral immunity Higher risk of infection and multiple organ dysfunction CLASSIFICATION OF BURNS Size of Burn: Lund and Broder chart or Wallaces ‘Rule of 9s’ Depth: 1st degree is involvement of epidermis and the burn is very painful, hyperaemic 2nd degree is partial injury of dermis, and is painful, pink and with possible blisters 3rd degree is full thickness, including dermal appendages, insensitive, red, white or black 4th degree is involvement of fascia, muscle or bone The estimate of the size of the burn (TBSA) is a total of burns beyond 2nd degree CRITERIA FOR ADMISSION All burns >15% BSA in adults Full thickness burns over 10% of BSA in adults Children with 5% or more of body involvement Burns to hands, face, feet, perineum and inner joint surfaces All respiratory burns. Electrical or chemical burns Circumferential burns ASSESSMENT A MAJOR burn is more than 15% BSA in adults and 10% in children. LUND-BROWDER chart must be used to assess the extent of the burn. Wallace’s Rule of 9s is a simpler alternative in adults Evaluate the patency of the AIRWAY: Inhalation injury usually appears within 2~48 hours post burn 1 Secondary to inhalation of combustion products. Symptoms: rales, rhonchi, stridor, cough and laboured or rapid breathing. Use high flow humidified oxygen to prevent drying of mucosa and hypoxia Airway Assessment for inhalation injury includes: Respiratory distress or upper airway obstruction Burns around face or neck Oedema of face or lips Oropharyngeal carbon or carbonaceous sputum Singed nasal hairs, eyebrows, eyelashes Inflammation or oedema of oropharynx Impaired consciousness These signs, especially 1, 2, 3 and 4 indicate the need to intubate Burn patients are among the most difficult intubations It is better to intubate early, than wait for respiratory distress. INITIAL TREATMENT 1. Stop the Burning Process and Relieve Pain Remove clothing, rings and other jewellery. Immerse or cover the affected area in cool water Provide pain relief: Diluted Pethidine, slow IV and titrate to response. 2. Fluid Resuscitation Principles Insert intravenous cannula (16G or 14G) through unburned skin. Budget FLUID resuscitation: Ringer Lactate- 2-4ml/kg/%BSAin the 1st 24 hours All formulas are budgets and need adjustment on physiological response Popular formulas: Modified Brooke (2ml) and Parkland (4ml)/kg/%BSA) Maintenance fluid is required in addition to above for children Indicators of response: Urine output (1ml in a child , 0.5 ml/hr in adult) Normal mentation, perfused extremities Mixed venous O2 >70%, normal arterial pH and lactate Colloid (Albumin, Dextran 70) in the 2nd 24 hours (0.3-0.5ml/kg/BSA) Add 5% Dextrose as necessary in the 2nd 24 hours to maintain urinary output (Hypertonic saline improves circulation, cardiac function faster and reduces load) Cardiac rhythm should be continually monitored for arrhythmia. Monitor vital signs and urine output hourly Acidosis, hypovolemia and hypothermia contribute to decreased cardiac output. Electrolyte disturbances are thought to be secondary to a defective sodium pump. Potassium is usually elevated 24-36 hours following the burn due to lysis of cells. After 72, hypokalaemia may develop as cell membranes regain their integrity. 3. Escharotomy and Fasciotomy 4. Tetanus Prophylaxis Previous Immunization <5 years: Nil Previous Immunization > 5 years: Booster No immunization or >10 years; 250=500 units of Human Antittetanus Globulin 2 3 The MODIFIED BROOKE FORMULA is only a guide 1st. 24 hours post burn Ringer’s Lactate : 2 mls x % of BSA x body weight (kg) (Half to be administered in first 8 hours post burn) Replacement should be reassessed on an hourly basis Insert a Foley’s catheter to assess urine output. Urine output should be no less than 0.7ml/kg/hr. If urine output is inadequate, increase infusion by 200ml next hour nd 2 . 24 hours Colloid 0.3-0.5ml/kg/BSA Dextrose to maintain urinary output 4. Treat Cardiovascular Instability: Cardiac rhythm should be continually monitored for arrhythmia. Monitor serial vital signs: P, BP, T, RR Foley catheter for accurate urine output for all patients with burn >20% Acidosis, hypovolemia and hypothermia contribute to decreased cardiac output. Electrolyte disturbances are thought to be secondary to a defective sodium pump. Potassium is usually elevated 24-36 hours following the burn due to lysis of cells. After 72 - 96 hours, hypokalaemia may develop as cell membranes regain their integrity. 5. Assess for Concomitant Injuries and Complications Burns 20% or greater carry a high incidence of paralytic ileus and Curling’s ulcer. A nasogastric tube should be inserted and Ranitidine 50 mg administered IV q8h Elevate limbs to decrease oedema. Flame burns to the neck and chest may contribute to respiratory difficulties The inelastic eschar of the anterior and post chest inhibits respiratory efforts. Escharotomies may be necessary Do not administer antibiotics. for prophylaxis since they predispose to resistant organisms INVESTIGATIONS Arterial blood gases Arterial carboxyhaemoglobin levels Full blood count Group and hold Electrolytes Blood glucose Blood culture Chest X Ray SPECIFIC TREATMENT 1. BURN WOUND Burns may be covered with cool water (not icy) if this brings relief. Analgesics, usually parenteral and titrated to patient need. (eg. IV Pethidine 100mg diluted in 10ml given slowly) Unburned areas should be covered to avoid hypothermia, especially in a child. 4 The aim is to cover the wound, reduce infection and allow healing and epithelialiization 2nd and 3rd degree burns that do not heal at 3 weeks require skin grafting Management includes: local care, topical agents, early excision and grafting Local Care: Wash with soap and antiseptic (eg. clorhexidine soap), remove debris, unroof blisters Open or exposure method with a bed net and cradle. Topical Agents: Silver sulphadiazine-0.5% (Silvadene or Silverex)- broad spectrum, fair penetration, painless. Mafenide acetate: (Sulphamylon) - broad spectrum, good penetration, painful, may cause acidosis Silver nitrate-0.5% -poor penetration, discoloration, causes Na/K depletion and methaemglobnaemia Early Excision and Grafting Eschar is excised at 2-7 days .and grafted immediately Grafting reduces evaporation, pain and protects underlying tissue Types of graft include-autograft, allograft, xenograft Skin substitutes include- cultured keratinocytes, dermal substitutes (Collagen, Vicryl mesh) Grafts usually split thickness and applied as sheets or mesh Cover with antimicrobials, Ca-alginate or occlusive dressing and pressure bandage Nutrition Metabolic needs proportional to BSA up to 50% Caloric needs calculated by the Harris Benedict equation and may be enteral/parenteral Physical and occupational therapy 3. COMPLICATIONS Infection and Septic Complications Invasive burn wound sepsis: Surface cultures are not helpful in diagnosis Diagnosis based on examination and histopathology Clinical features: Progressive depth, discoloration and haemorrhage, erythema Histopathology: Biopsy 500mg of lenticular tissue- half for histology; half for culture Stage I- Colonization: (a) superficial, (b) penetrating and (c) proliferating Stage II- Invasion: (a) microinvasion, (b) deep invasion and (c) microvascular Organisms: S Aureus-35%, Pseudomonas 9%, E Coli 5%, Proteus 4% Rx; Debridement, drainage and topical agents IV antibiotics- Empirical: Nafcillin, Piperacillin, Amikacin. Specific- based on C/S Pneumonia Most common infection is bronchpnemonia (S .Aureus, or Gm-ve organisms) First evidence may be on X-rays as ill defined infiltrate Rx is antibiotics adjusted on basis of C/S Suppuratve thrombophlebitis Can occur at any time and risk increases with duration(3 days) of catheter/cannula Local signs may be absent Haematogenous pneumonia or septicaemia should prompt exploration and excision of vein Acute endocarditis Risk proportional to durration of IV infusion and thrombophlebitis S Aureus is the most common organism and systemic antibiotic Rx for 3 weeks Bacterimia and Septicaemia Systemic antibiotics used prophylactically induce resistance Blood cultures should be obtained on scheduled basis 5 Administer antibiotics on the basis of laboratory diagnosis of infection Empirical Rx on basis of known surveillance data, Gm stain of infected secretions Critically ill patients may grow multiple organism and antibiotis Rx should cover all Gastrointestinal Complications Curling’s Ulcers: Mostly in stomach, duodenum ?hypoperfusion. Rx PPI. H2R. Antacids Adynamic ileus and acute dialatation of the stomach and colon: Rx IVF, NGT Acalculous cholecystitis : diagnosis on USS or HIDA scan. Rx Antibiotics Cutaneous Contarctures and burn scar; cosmetic and functional problems Hypertrophic scars, keloids and hyperpigmentation Carcinoma (Marjolin’s ulcer): Rare but latent period from 1-75 years Eyes: Corneal abrasions and cataracts Involve Ophthalmologist early in facial burns MUHIMBILI NATIONAL HOSPITAL (Department of Surgery) PROTOCOL FOR MANAGEMENT OF BURNS: Initial Management Name: Age: Sex: Occupation: Residence: Date: Time of admission. Date & Time of burn. Open/Closed space Burn agent: Scald Flame Flash Electric Chemical Other Primary Survey & Resuscitation Airway: Clear Compromised- Confined space/Evidence of Inhalation: Yes No Face/Neck burn: Yes No Hoarseness, stridor, wheeze: Yes No Head injury/unconscious: Yes No Breathing: Circumferential chest burn: Yes No Evidence of hypoxia: Yes No Respiratory Rate: /min Breath Sounds: Air entry (<) (N) Vesicular. Rhonchi Crepitations Rx: Oxygen. ETT, Assisted Ventilation, (Monitor-SaO.) Circulation: Pulse: b/min. BP: mm.Hg Capillary return: Good Poor Start IV Line (R/L or N/S) Cannula (Adult- Size 12-14 x 1-2 lines) Take blood for base-line studies Rx: FLUID BUDGET: Crystalloid 2-4ml/kg.BSA/ for the 1st 24hours (Modified Brooke Formula) 1st 8 hrs Next 16 hrs R/L or N/S 1ml/kg/% 1ml/kg/% Colloid 5% Dextrose - Next 24 hrs 0/3-0.5ml/kg/% To maintain urine output (0.5ml/kg/hr) * In CHILDREN : (1) 3 ml/kg/%BSA of R/L + Maintenance fluid is recommended for the Ist 24 hours (2) Aim at urine output of 1ml.kg/hr in CHILDREN Disability: (AVPU) Alert Response to Verbal stimulus Response to pain Unresponsive Exposure: (Avoid hypothermia) Head - Toe examination for burn and associated injury 6 Secondary Survey 1. History (AMPLE) Allergy: Medications: Past Illness: Last meal at: Events leading to burn: 2. Burn Injury: Site: Extent (%) : (Use Wallace’s Rule of 9s or Lund-Browder Chart) Depth : (Indicate as 1st, 2nd or 3rd degree on basis of appearance and sensation to pin-prick) 3. Associated Injuries: ( Specify) 4. Weight: Kg. Height: Metres Surface Area: m.sq 5. Investigations: Hb gm/dl . WBC Platelets (Serial) Electrolytes: Na K Cl Creatinine Glucose Blood group: Urinalysis: CxR: Medications/Monitor : 1. Analgesia: Pethidine 100mg diluted in 10 ml (1mg /kg) slow IV & titrate.: 2. Tetanus Toxoid 0.5ml for patients with no boosster in the last 5 years 3. Penicillin for Streptococcus prophylaxix (no broad spectrum prophylaxis) 4. Foley’s catheter (chart hourly output) and Ryle’s (NG) tube (>25% burn) . 5. Wound Care: Clean and apply Silver sulphadiazine cream 6. Ulcer prophylaxix: Ranitidine 50mg IV q8h/ Antacid 30ml q4h 7. Other: Escharotomy for deep/constricting circumferential burn Knowledge Module Burns Lesson 1 – Pathophysiology of Burns Lesson 2 – Types of Burns Lesson 3 – Treatment of Burns 7 BURNS Lesson 1: Pathophysiology of Burns Purpose (Terminal Objective): The purpose of this lesson is to: A. Explain the pathophysiological changes that occur with burns 1. The student will understand the direct effect of burns 2. The student will understand the secondary/systemic effects of burns Method/Media: Self Taught or Lecture. Training Aids: Chalk/whiteboard (optional). Evaluation: Written examination. See end of Lesson 3. Test every three years. References: Emergency War Surgery (NATO Handbook). Textbook of Military Medicine – Conventional Warfare: Ballistic, Blast and Burn Injuries. ABLS (Advanced Burn Life Support) Manual. HM 1 & C, HM 2 & 3. Content Information: A. Pathophysiologic changes in burns 8 1. Direct Effects: a) Burn severity is proportional to the extent of the cutaneous injury. At temperatures of >50 degrees C, protein denatures. Differences and similarities exist between thermal, chemical, and electrical burns. These differences are due to the duration of time skin is exposed to the agent, specific heat of reaction, protein avidity of the chemical agent and characteristics associated with different types of electrical burns, and the nature of the current in the electrical circuit. b) With burns, the skin is destroyed to a level corresponding to the insult. This may include superficial or complete partial thickness loss, which leaves skin appendages such as hair follicles and sweat glands intact or full thickness loss, which destroys all skin and skin appendages. Direct effect of chemical burns may include a “poisoned” zone wider than the obvious burn where cells have received enough of the chemical to become damaged. In electrical burns, all structures along the path from entry to exit may be injured, creating a zone of injury larger by far than the obvious burn. c) Loss of skin will lead to loss of the barrier to invasion by bacteria, decrease in the body’s ability to thermoregulate as sweat glands are destroyed, and loss of fluids to the environment through evaporation which is uncontrolled absent a skin barrier (this will also cause thermoregulation problems). The extent of these changes depends on the depth and the extent of the burn. d) Burns are classified by their depth and extent: (1) (2) e) B. CLASSIFICATION BY DEPTH: (a) FIRST DEGREE : superficial partial thickness. (b) SECOND DEGREE : partial thickness. (c) THIRD DEGREE : full thickness (d) FOURTH DEGREE: Includes deep tissue charring Classification by extent – the Total Body Surface Area (TBSA) of 2nd, 3rd and 4th degree burn. Pulmonary burns will not be covered in detail. However the main direct effects of burns to the respiratory system are edema and sloughing of the epithelial lining. This may cause acute laryngeal edema blocking the airway, or filling of alveoli with debris & edema causing impairment of air exchange. Indirect effects: 1. Indirect effects refer to the systemic effects that burns cause, even systems that are untouched by the burn. These include both immediate (I) and delayed (D) effects. 9 2. Fluid shifts/shock (I): The loss of significant skin and the localized effect of the burn on surrounding tissue results in massive fluid shifts out of the vascular spaces and into interstitial spaces. The burn patient has tremendous edema everywhere, and reduction of circulating fluid volume leads to severe shock. 3. Metabolic acidosis (I): This is due to hypoperfusion. 4. Compartment syndrome (I/D): Secondary to eschar formation, vascular injury, and hypoperfusion. 5. Anemia (D): Due to RBC destruction. 6. Renal failure (D): Due to hypoperfusion, renal tubular acidosis, or myoglobinuria. 7. Cardiac dysrhythmias (I/D): Due to hypoxemia, hyperkalemia, and metabolic acidosis. Immediate dysrhythmias are mostly seen in electrical burns. 8. Mortality in burns is primarily related to TBSA (total body surface area) burned. Concomitant inhalational injury also increases burn mortality. Co-morbid factors such as age (very young or elderly), systemic disease (diabetes, cardiac disease, etc), and others will increase mortality for a given TBSA. A rough estimate of mortality is: MORTALITY = AGE + TBSA BURNS Lesson 2: Types of Burns Purpose (Terminal Objective): The purpose of this lesson is to: A. Explain the different types of burns. 1. B. The student will be able to identify the different types of burns. Explain the clinical presentation of different types of burns. 1. The student will be able to understand and identify clinical features of different burns. Method/Media: Self Taught or Lecture. Training Aids: Chalk/whiteboard (optional). 10 Evaluation: Written examination. See end of Lesson 3. Test every three years. References: Emergency War Surgery (NATO Handbook). Textbook of Military Medicine – Conventional Warfare: Ballistic, Blast and Burn Injuries. ABLS (Advanced Burn Life Support) Manual. HM 1 & C, HM 2 & 3. Content Information: A. B. Types of burns: 1. Thermal burns: These represent the largest category of burns, and are the result of direct flame action, or the application of dry heat (as in sunburn). 2. Chemical burns: Acids and alkalis are the most common causes. Petroleum products, especially gasoline can also cause severe burns. These chemicals can be either wet or dry and cause injury by direct skin contact/mucous membranes or inhalation. 3. Electrical burns: Significant electrical burns are caused by higher voltage (up to very high voltage) current. For a given voltage, increasing amperage increases the danger of the shock. 4. Scalds: Scalds are burns caused by hot liquids (e.g.: boiling water). In adults they tend to be of limited danger due to the relatively small TBSA, but can be a significant problem in children 5. Inhalation burns: These are burns to the airway, caused either by thermal injury or chemical injury. 6. White Phosphorus (Willie Peter): This is a special burn of military significance. WP will continue to burn as long as it is exposed to air. If cut off from air WP will recombust if re-exposed. Clinical features of burns 11 1. Common features: Whatever the cause, most burns present with certain common features based on the depth of the burn. a) First degree: These burns are like a severe sunburn. The skin is reddened and painful but no blisters are formed. b) Second degree: These burns are extremely painful, may show some white patches, and have rapid onset of blister formation. Blisters are the hallmark of 2nd degree burns. c) Third degree: With full thickness burns the skin appears mottled or white. It is leathery, there are no blisters, and areas of 3rd degree burn are initially relatively painless, as the nerve endings have been destroyed. d) Fourth degree: Here you see severe charring, like a piece of meat burned on the grill. Much deeper tissues may be affected. 2. Chemical burns may be especially painful as the chemical continues to destroy tissue until it is diluted either by spread or medical intervention. 3. Electrical burns will present with an entry point for the current and an exit where it went to ground. Absence of pulses due to an acute compartment syndrome is common, as are cardiac dysrhythmias. The zone of injury is much wider than it appears at first glance, and progressive muscle necrosis is common. Renal failure due to myoglobinuria may occur early. 4. Lightning Injury is a special type of electrical burn, which may present with cardiopulmonary arrest. These casualties have an excellent chance of recovery if CPR is started promptly. 5. Pulmonary Inhalation burns: Always check for a patient coughing soot, facial burns, burns in the nares. Stridor and dysphonia (voice change) are also tip-offs that the respiratory tree has been burned. 6. WP burns: In white phosphorus burns, you will see the wounds smoking and smell a garlic-like odor as the WP continues to burn. BURNS Lesson 3: Treatment of Burns Purpose (Terminal Objective): The purpose of this lesson is to: A. B. Identify clinical parameters for burn treatment. 1. The student will be able to identify burn severity (TBSA). 2. The student will identify criteria for levels of treatment and evacuation. Identify treatment protocols and actions for burns. 1. The student will be able to identify general treatment protocols. 12 2. The student will be able to identify treatment protocols for different types of burns. Method/Media: Self Taught or Lecture. Training Aids: Chalk/whiteboard (optional). Evaluation: Written examination. See end of Lesson 3. Test every three years. References: Emergency War Surgery (NATO Handbook). Textbook of Military Medicine – Conventional Warfare: Ballistic, Blast and Burn Injuries. ABLS (Advanced Burn Life Support) Manual. HM 1 & C, HM 2 & 3. Content Information: A. Clinical indicators for burn treatment. 1. The key piece of information to know in treating burns is the %TBSA (total body surface area) burned. This is 2nd and 3rd degree burn (and 4th if present), 1st degree burn area is not included in the calculation. In calculating TBSA in adults use the “Rule of Nines” listed below: 2. Estimation of the extent of the burn site is by using the ‘Rule of Nines’. Region head/neck % TBSA 9 13 posterior thorax (back) 18 anterior thorax (chest) 18 upper extremity (each) 9 lower extremity (each) 18 Perineum B. 3. Rule of the patient’s palm -The patient’s palm size approximately equals 1% of the patient’s TBSA. Estimating the number of palms that would cover the burned area equals the percent of the body surface area involved. 4. Estimating burn wound size in children is similar, but the head is relatively larger and the legs are relatively smaller. Thus the “Rule of Nines” is not accurate, however the Rule of the Patient’s palm will work. Evacuation of burns: The policy for burn evacuation in a combat environment will be set by higher authority, but in general persons with limited burns not involving hands/feet/face/perineum may be kept on the line. 1. 2. C. 1 The following guidelines are those of the American Burn Association and are recommendations for transport of patients to burn units: a) second & third degree burns > 10% Total Body Surface Area (TBSA) when < 10 yrs or > 50 yrs; > 20% TBSA for all other ages. b) full thickness burns > 5% TBSA. c) burns to the face, hands, feet, perineum, eyes / ears. d) high voltage injuries - includes lightning. e) airway burns. f) significant chemical burns. g) burns associated with pre-existent disease e.g. diabetes, cardiovascular disease. It should be remembered that all burns need treatment, even if minimal. Burn treatment protocols 1. General interventions for burns a) Stop the burning process (extinguish flames/remove clothes if necessary), remove from toxic environment, remove from electrical current. Ensure appropriate ATLS/transport principles are followed. b) Check ABCs, especially airway. c) Estimate Burn Depth and extent (TBSA) 14 d) Major Burns – see ABA criteria above (may be modified by the Unit Surgeon). (1) If inhalation burn present perform endotracheal intubation. (2) Place 2 large bore IVs (3) Fluid replacement IAW Brooke Formula: 2-4ml/kg x %TBSA Burn: give ½ in first 8 hours after burn and remainder in the next 16 hours. e) D. (4) Cover burn with dry sterile or Water Gel burn dressing. (5) Pain Control (6) Prevent hypothermia (7) Prepare casualty for evacuation (8) Foley catheter, supplemental O2 and NG tube may be initiated at medical facility Minor Burns (1) Clean burn with soap and water (2) Cover with dry sterile or Water Gel burn dressing (3) Consider pain control (4) Refer to BAS for Medical Officer evaluation. Specific burn treatments 1. 2. Chemical burns a) Remove chemical, brush off dry matter then flush with water/saline. b) Neutralizing solutions are only used in very specific instances. c) Cover with dry sterile or Water Gel burn dressing d) Consider pain control e) Refer to BAS for Medical Officer evaluation. Electrical burns a) Don’t become a casualty – ensure patient no longer ‘hot” before you touch him. b) May require CPR or ACLS if cardiac dysrhythmias or arrest. c) Treat as for Major burn, as above. 15 d) Monitor urine carefully, may require IV bicarbonate to alkalinize urine to prevent tubular plugging secondary to myoglobinuria. e) At higher medical levels, be aware that multiple debridements or progressively higher amputations may be necessary as muscle necrosis becomes clear. 3. WP burns – cover with occlusive dressing such as petroleum gauze, the Water Gel burn dressing or a field expedient such as mud. 16