Early Adopters - Communities of Practice
advertisement

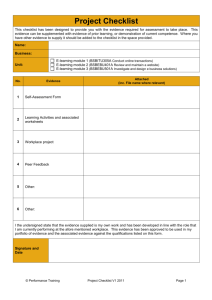
LESSONS FROM EARLY ADOPTERS Craig Bosenberg and Susan Maknack, Regina Qu’Appelle Health Region www.safesurgerysaveslives.ca Craig Bosenberg, Anesthetist, Regina Good Morning. I am Craig Bosenberg, an anesthetist from Regina and I am here together with Susan Maknack, a QI consultant from our region, as members of the team leading the implementation of the WHO checklist in RQHR. We are honored to be asked to relate our experiences to this group and hope that some of our story may be of use to yourselves as you embark on the same project. There are a few themes I would like to emphasize in our story which was mentioned in Bryce’s talk, but I think bear repeating: The WHO checklist is not just another bureaucratic checklist aimed at making the lives of physicians and nurses in the Operating Room busier than it already is. It obviously a tool aimed at reducing error from human factors, but more than that it is a tool for changing the culture of the OR from one of many separate groups working in their own world who meet over a patient to one where all team members form part of a team engaged in the same process of doing an excellent and error free operation. It is a tool for taking the implicit communication that happens every day in our ORs and making it explicit. It is critical in our opinion that any exercise aimed at implementing this checklist understands this, as this gives one an insight into the magnitude of the project at hand and the “change” management involved. In our institution if this succeeds, it will mean that we will have changed the lifelong practices of almost every surgeon and anesthetist. In our institution, it has therefore been absolutely critical to our success to not only engage our fellow clinicians in the process but also to INVOLVE them. This has been one of our greatest challenges to date and also one of our greatest successes. Our story began about 3 years ago when we realized that we had a problem in our ORs after a rash of critical incidents which resulted in patient harm. In the space of a year we had a morbidly obese patient fall off the operating room table and sustain a laceration to her head requiring several stitches, we did a total hip replacement proceed, only to find out that the prosthesis for the patient was not in the province. We also had 2 wrong site surgeries. We had known for a while that our practice of “time outs” or “surgical pauses” had not been well implemented and had been seen by most as another bureaucratic “tick and flick sheet”. As if to emphasize this point, all of the incidents mentioned above had happened in Operating Rooms where the surgeons involved were amongst the more enthusiastic adopters of the surgical pause. We realized that the problem was not the checklist, but that all the members of the team were not engaged in it and didn’t really “buy in to it”. We therefore started looking for ways to improve this engagement. We talked about “surgical huddles” but really didn’t think we had a hope of implementing that in our culture as it was too amorphous and lacked any evidence for it. We then came across the WHO checklist after some of us heard Atul Gawande speak at IHI a couple of years ago. We wanted to see if we could implement it in Regina. Building a safer health system LESSONS FROM EARLY ADOPTERS Craig Bosenberg and Susan Maknack, Regina Qu’Appelle Health Region www.safesurgerysaveslives.ca As the head of anesthesia, I approached and got the mandate from the surgical program to set about implementing this. We therefore established a working group of surgeons, anesthetists and nurses to achieve this. Our team has always emphasized that this should be a “grass roots” exercise if we were to have any chance of success and that if it was seen to be something forced on the operating rooms, our chances of success would be fairly limited. To this end, we have sought the advice of our peers every step of the way and have also concentrated on engaging the “informal” and formal leaders of the Operating Rooms in the process. As an anesthetist, having a surgeon as a captive audience for a day at a time can be very useful in this task. We have also positioned ourselves to be able to be fairly agile in terms of jumping on opportunities as they arise: One example - you will remember that one of our motivators was the wrong site surgeries we had had - one of those occurred in the room of our chief of surgery who up till then had been a supporter, if not that enthusiastically, of this project. On the day he had his wrong site surgery, he demonstrated extraordinary courage and leadership when he stood up in front of the surgery business meeting and told his peers about his mistake and then advocated for an improvement in our checklist procedure. Overnight, surgeons - who had up till then been fairly tepid in their acceptance of the surgical pause - started to ask about it. In my room the next day, one surgeon who had always poo poo’s the paused stopped before starting his case and told everyone in the room that while he realized he was often a bit grumpy he wanted them to stop him if they thought he was going to make a mistake, no matter how trivial. All we needed to do after that was to amplify this “buzz” and positively reinforce these sorts of actions. We therefore worked to increase awareness and grow our team. After IHI this year we found ourselves in the extraordinary position of having to “slow things down”. We had initially planned to have Bryce come and talk to us about his experience as an introduction to the pilot project which we were launching. Because of Don Berwick and Atul Gawande’s message at IHI a number of high level leaders came back and told us they wanted this implemented and soon. We even got a letter from the ministry suggesting the same. We had to impress upon them that we were already well under way and that if this was seen to be coming from the ministry or even the SMO’s we might put the whole project in jeopardy. Our pilot project therefore began a week before Bryce arrived to talk to us and his talk had exactly the impact we had hoped. We were in a position to capitalize on the enthusiasm created by this event and we currently have the WHO checklist being done in most of our Operating Rooms in the form of a PDSA. We chose to use this format because we had to capture the enthusiasm of our colleagues, but realized that we would not be able to standardize the process if it was happening in so many rooms being done by so many different people. By incorporating this in a PDSA, we have invited anyone interested, to do the checklist and to give us feedback on what works and what doesn’t. This engages and involves people in the project and also gives us the data to modify the checklist into something we can standardize across all the operating rooms in the future. Building a safer health system LESSONS FROM EARLY ADOPTERS Craig Bosenberg and Susan Maknack, Regina Qu’Appelle Health Region www.safesurgerysaveslives.ca As a final word and to underscore our approach, I would like to relate the story of how a skilled “influencer” in our team turned a colleague from a person who would have undermined the checklist into a powerful champion: One of our strongest team members is the head of gynecology. She is a young physician who has a passion for improving the care of her patients on a systemic level and was the first physician to pilot the checklist in our region. Knowing that she needed an ally in her department other than the chief of OBGYN, as we moved this forward, she decided to approach one of the most influential but stubborn members of her department for help. She knew that he viewed himself as a “trendsetter” and took great pride in the fact that he is one of the best laparoscopic surgeons in the country. He sees himself as “one of the boys”. She therefore approached him by suggesting to him that by being involved in this, he would be “cutting edge” and a leader in Canada. In other words she appealed to the thing that she knew would have the most influence on him. This piqued his interest and while not an enthusiastic supporter, he seemed to be happy to “go along with it”. The next day he did come to Bryce’s talk and was impressed. He therefore decided to “give it a try” himself in the women’s clinic the next day. On the very first case he did, he picked up that the patient had not had her antibiotics. And he said “BINGO”. Another champion! SUSAN MAKNAK, QUALITY IMPROVEMENT CONSULTANT, REGINA Good afternoon, I would like to start by thanking Craig and Dr. Stan Vuksic, another anesthetist who is here with us today. They were the ones with the “captive audience” for 8 hours and having the water cooler discussions to promote our hard work. Thanks to both of you. Before Bryce’s visit, Operating Room nursing staff at both sites had been educated on the checklist by Marg Farley. She is always on the “cutting edge” of what is new and willing to share it with us. After Bryce came, we found there were many unofficial attempts to sue the checklist with no way for us to capture any learnings. Everyone went forth and “checklisted”. We did not want to dampen the enthusiasm for the checklist but feedback was only anecdotal. In order to learn from these attempts, all interested surgeons, anesthetists, and nursing staff were invited to participate in a “PDSA”, Our Message was: We need your input for what the checklist should look like in RQHR This is your opportunity to tell us what you think about it Give it a try, see how it works Building a safer health system LESSONS FROM EARLY ADOPTERS Craig Bosenberg and Susan Maknack, Regina Qu’Appelle Health Region www.safesurgerysaveslives.ca This will need to be standardized, so we value your input Any person, any procedure, any time This is step #2 of what Bryce was talking about. We were talking it up and enlisting our champions. PDSA#1 Paper copies of the checklist were placed in all theatres at both sites. The checklist was on the front, on the back of the sheet we asked for the surgeon, anesthetist, and procedure. We felt this was important if we needed to learn more about what was working and wasn’t and if it was related to a specific procedure or physician. Number of minute’s checklist took What worked, didn’t and a place for comments. We also encouraged people to write any comments on the checklist side so we would know what needed to be explained more. We started this last Friday at 0800 and Sunday at 1400, Marg picked up 35 charts that we were happy to say included dental surgery and eye surgery. Messages from PDSAs Bryce, this is feedback from people who are accountable “Suggest follow up surgery of patients who had checklist performed while awake” “Everyone stopped and listened, worked best when led by surgeon” “I think once we get used to it, it will be better accepted and performed” “More surgeon and nursing education needed” Average time 3-4 minutes. We know we can improve on this, just as Rob indicated in his talk, that once people get used to it, we will decrease this time. So, we are hoping we can apply what we have learned from these and apply them to our Pilot will be OBS/Gyne. This is the service that has the champion that Craig mentioned. Now, to refer to what Marlis was talking about, our region is doing the Surgical Site Infection Prevention project, the Saferhealthcare now! Initiaitve, at 2 sites with 3 services. Obs/Gyne is not one of them. We will now begin an education blitz that will include education for the checklist, SSIPP, and the model for improvement – PDSAs. We think this is important for any changes we may need to try before next Tuesday, that people understand what “small tests of change” are and why they are important. We will start with “superusers” and that will be the specialty co-ordinators in surgical suites. We hope to have a “getting started kit”. Building a safer health system LESSONS FROM EARLY ADOPTERS Craig Bosenberg and Susan Maknack, Regina Qu’Appelle Health Region www.safesurgerysaveslives.ca Then we will move to all OR nursing staff and inpatient nursing staff. We will co-ordinate this with Education days. We want to strengthen nursing’s confidence to “stop the line” if needed We will also educate anesthesia and surgeons. The chief of OBs/gyne is presenting to her whole department this morning. Our aim is to have a strong member in each theatre. Existing white boards in theatres have staff names on them now. We are purchasing bulletin boards for outside theaters with important information on. Such as the PDSA of the week, how are we doing? We will then have to decide with our multidisciplinary OR Safety working group to standardize the checklist and decide what is negotiable and non-negotiable and develop a roll out plan. I would also like to share a story with you. One of our SSI groups in Neurosurgery. The neurosurgeons have been a great group to work with and have changed their booking forms to include antibiotic ordering. We have some outlieers who do not have the antibiotic ordered how we would like. WE have worked with Day surgery to place a red dot on our SSIPP data collection form to alert OR staff that an order is needed. There has been grumblings from this staff, this is silly, why do we have to babysit, the OR, why can’t they just do it. After Bryce’s visit this staff’s attitude has changed. They were very pleased to be invited to this “OR” talk and to be included in something this important. The next working group meeting they came saying “Now we get it, now we understand our role and why the red dot is important”. So I agree, it is not about the checklist but a tool to engage people in discussions about what is best for the patient, just as Phil indicated. So in conclusion, we are not sure what this will look like for RQHR, but what we are hoping for is a “memorable home run”.. Building a safer health system

![Assumptions Checklist [Word File]](http://s3.studylib.net/store/data/005860099_1-a66c5f4eb05ac40681dda51762a69619-300x300.png)