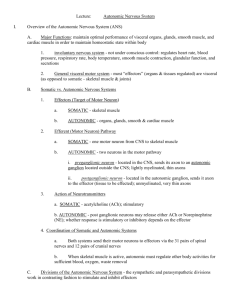
Central autonomic nervous system handout
advertisement

BMS Endocrinology John Morris HYPOTHALAMIC/CENTRAL CONTROL OF AUTONOMIC NERVOUS SYSTEM The hypothalamus acts as integrative centre for regulation of the autonomic nervous system by the cerebrum, by feedback, and from its own intrinsic sensitivity. It is involved in homeostasis; stress responses; anticipatory responses; part of integrated somatic/endocrine/autonomic responses. Sympathetic and parasympathetic are essentially output systems; there are also visceral afferents which are important in both physiological regulation of and pain from the viscera; and the enteric nervous system which integrates control along the gut. Functionally: Sympathetic: response to injury or potential injury; ‘fight or flight’ Parasympathetic: active when well-fed, warm, with 'good friend'; ‘rest and digest’ Both systems can be activated by: extrinsic (e.g. pain) and intrinsic (e.g. BP) stimuli, analysed via 'limbic system'; by psychic activity (e.g. anxiety - tachycardia; shyness - blushing; favourite food - salivation; erotic material - vascular changes in genitalia; anxiety - block of milk ejection, menstrual cycle). PERIPHERAL AUTONOMIC SYSTEM (brief revision of the main points of the systems) A. Autonomic efferent systems 1. Sympathetic system preganglionic neurons: spinal cord T1-L2,3 sympathetic ganglia: chain from base of skull to end of sacrum inputs: preganglionic axons from thoraco-lumbar cord outputs: from all levels of the sympathetic chain distribution: postganglionic fibres to head, trunk, limbs; preganglionic fibres via midline ganglia to viscera neurotransmitters: preganglionic: ACh (nicotinic) postganglionic: NA, ACh, peptides receptors: α & β types and subtypes - effects of drugs 2. Parasympathetic system preganglionic neurons: Cranial nns III, VII, IX, X; sacral cord S2-4 ganglia in or near targets; short postganglionic axons distribution: to head via ganglia: - ciliary (III) - globe of eye: pupillary sphincter, ciliary muscle - sphenopalatine (VII) - hard palate, nose, lacrimal gland - submandibular (VII) - submandibular and sublingual salivary - otic (IX) - parotid; NB Cranial parasympathetic ganglia also act as distribution centres for sensory (V) and postganglionic sympathetic nerves distribution: to viscera via vagus (X); pelvic parasympathetics - X supplies forgut and midgut derivatives; kidneys - pelvic parasympathetic (S2,3,4) supplies hindgut, pelvic organs. neurotransmitters: muscarinic ACh, peptides - effects of drugs 3. Enteric system neurons and plexuses in alimentary tract wall; intrinsic reflexes of gut inputs from sympathetic and parasympathetic axons modulate activity neurotransmitters: ACh, amines, peptides, ATP B. Visceral afferents: receptors in gut, lung, cardiovascular sensitivities - distension, pain routes of axon projection to the CNS - physiological via IX, X, S2-4 - pain via sympathetic pathways projection to nucleus of tractus solitarius Further reading: Donadio V et al (2009) J Neurol Neurosurg Psychiatry on line.Autonomic innervations in multiple system atrophy and pure autonomic failure. Kaufmann H et al (2010) Neurology 74:536 Pure autonomic failure: a restricted Lewy body synucleinopathy or early Parkinson disease? CNS CENTRES CONTROLLING THE ANS Hierarchical organisation of parts: spinal cord, medulla, pons, hypothalamus, cerebral cortex. SPINAL CORD: spinal shock: causes absent reflexes, low BP; reflexes start to return and BP rises, but reflexes are segmental; if cord then lesioned BP falls again and does not recover. Very difficult to demonstrate coordination in absence of higher centres. sacral centres control bladder, rectum, genitalia (erection, emission; ejaculation (requires somatic (pudendal) nerve)); role oxytocin automatic bladder/rectum - after spinal cord injury the bladder/rectum fills to a certain volume, then discharges. mass reflex: a minor sensory stimulus can cause limb withdrawal, sweating, defaecation., micturition. Probable cause: lack of inhibition from higher centres, sprouting of dorsal roots, denervation hypersensitivity. Cilio-spinal centre C8,T1- this determines the sympathetic (dilator) action on the pupil. MEDULLA: centres which control autonomic output for cardiac (pressor and depressor), respiratory (inspiratory, expiratory, pneumotaxic), salivation (superior (VII), inferior (IX)); vomiting (swallowing); control of blood sugar. If cord and medulla are intact, TONIC control is OK, but responses to challenge are very deficient, and there is no anticipation or coordination with somatic responses. PONS: micturition centre (starts to function only well after birth). CEREBELLUM: motion sickness - autonomic effects salivation, sweating Experimental stimuli in cerebellum cause changes in BP, heart rate Injury to the cerebellum often affects frequency of micturition. HYPOTHALAMUS: Sherrington's "head ganglion" of the autonomic NS; but without cerebral cortex, control is incomplete. ‘Centres’: heat/cold; homeostatic responses; resistance to stress; organises visceromotor; rage reaction. (NB functional areas do not necessarily correspond to nuclei. In general stimulation of anterior hypothalamus gives parasympathetic effects; posterior gives sympathetic effects. AMYGDALA: stimuli cause changes in sympathetic and parasympathetic (BP); removal causes placidity (deficits in social ranking; submissivity). CEREBRAL CORTEX: Lesions can affect micturition control; poor temperature regulation. Stimuli all over (esp frontal) affect BP control; shunting of blood, anticipatory and response. Anticipatory vasodilation of arterioles in muscles about to be active. Cerebral localisation of autonomic activity reflects somatic in motor and premotor; visceral afferents reach sensorimotor primary and sensory cortex via NTS and VPM; interconnections to posterior orbito-frontal cortex, mediodorsal (MD) thalamus and limbic structures Complete control of ANS requires all parts of the CNS ---------------------------- ORGAN CONTROL BY SYMPATHETIC & PARASYMPATHETIC SYSTEMS Pelvic --------------------------RECEPTORS Cholinergic (N1 nicotinic N2 nicotinic M1, 3, 5 muscarinic M2, 4 muscarinic ion channel ion channel Gαq; PLC; IP3 & DAG Gαi, o; AdCycl; cAMP somatic NS) symp., parasymp.ganglia; adrenal medulla Adrenergic α1 (NA>A) α2 (NA>A) β1 (A>NA) β2 (A>NA) β3 (A>NA) Gαq; PLC; IP3 & DAG Gαi; AdCycl; cAMP Gαs; AdCycl; cAMP Gαs; AdCycl; cAMP Gαs; AdCycl; cAMP predominate on blood vessels predominate on presynaptic terminals e.g. heart on SAN, muscle; JGA, e.g. bronchial, coron art smooth muscle, liver e.g. fat cells, vasodilate salivary gland e.g. heart bradycardia; presyn muscle vasodil. 5-HT ATP P2 purinoceptors Ca channel NO e.g. use of TNG in angina, sildenafil (Viagra) in erectile dysfunction; in pulmonary oedema. Peptides: VIP, opioid peptides, somatostatin; substance P, CGRP in visceral afferents SUMMARY OF AUTONOMIC CONTROL OF END ORGANS (Symp = sympathetic; PS = parasymp) EYE Pupil size (Symp α1 dilates, PS (M) (III) constricts), (opiates constrict) Accommodation: ciliary muscle (PS (III) accommodates), pupil changes; Lacrimation (VII): via int. acoustic meatus and sphenopalatine ganglion Afferent stimuli: light, accommodation. Consensual pupillary reflex. Pupil constriction on stimulation of visual area 19 (the visual area giving the most corticofugal fibres; role in fixation), and of frontal eye fields (area 8; connected to limbic structures, hypothalamus, PAG) Sympathetic cilio-spinal centre (C8,T1) > SCG > NA symp fibres to eye; Horner's syndrome (symp denervation of head) - usually caused by lesion at the neck of the first rib as sympathetic chain leaves the chest. Parasympathetic from Edinger-Westphal III, via III > ciliary ganglion > ciliary nerves (ACh) Maximum pupillary dilation probably needs both an increase in sympathetic and a decrease in parasympathetic tone Think about drugs applied to eye to dilate pupil in ophthalmology Lacrimation - VII (long complex pathway: facial nerve parasympathetic (N & M) via internal acoustic meatus, petrosal nerves, spheno-palatine ganglion, to gland). Basal, reflex and psychic tears. CARDIOVASCULAR Control of heart rate & force Control vessel tone (esp. arterioles); Control blood volume Afferents: baroreceptors, chemoreceptors, via IX, X to nucleus of solitary tract; all somatosensory especially pain Hypothalamus posterior: stimulation gives pressor BP+, rate+, vasoconstrictor Hypothalamus anterior: stimulation gives depressor, vasodilator; (osmoreceptor neurons for control of body water) Some hypothalamic effects are indirect via brain stem centres; some are direct Cerebellum: stimulation anywhere leads to cardiovascular changes Cerebral cortex: anticipatory vascular changes before movement; Stimulation motor areas 4, 6: vasomotor changes even in paralysed limbs Sympathetic (β1): increased speed SA node, speed AV conduction, positive inotropic; vasoconstricts/dilates vascular beds depending on receptors. Parasympathetic (M2): decreased speed SA node and conduction, (minor negative inotropic); splanchnic dilation THERMOREGULATION Control of vascular system Control of sweating (cholinergic sympathetic), Control of metabolism: via ANS; control thyroid Spinal/ bulbospinal animals are poikilothermic; need HT for homeothermic regulation Hypothalamus anterior: heat loss: thermosensitive neurons;: local heating or electrical stimulation leads to panting, heat loss Hypothalamus posterior: heat conservation: stimulation gives shivering, vasoconstriction, piloarrection (no thermoreceptor neurons). Bilateral lesions post hypothalamus impair capacity to adapt to low temperature. Symp stimulates brown fat metabolism (neonate) Pyrogen responses: affect thermostats of anterior HT (via PGs - aspirin); responses depend on integrity of posterior HT If injected into anterior hypothalamus : pyrogens, 5HT raise body temp; A, DA, NA lower body temperature. Postoperative hyperthermia common after operations on/ HT, suprasellar pituitary tumours Piloarrection is produced by stimuli in many areas (but NB temp, rage) Shivering produced by a graded increase in tone (10-20/sec contractions); suppressed in cortical voluntary movement Associated somatic behaviour: stamping feet when cold; “its too hot to move”; clothes DIGESTIVE SYSTEM and FEEDING ANS influences all aspects; stimulated by parasympathetic activity. Motility and migrating myoelectric complex starting in duodenum. Secretion: control submandiular gland via VII, parotid gland via IX; Gut: oesophagus to splenic flexure colon via X; hindgut pelvic PS. (ACh M). Hypothalamus anterior: stimulation increases secretion/peristalsis (parasympathetic); senses nutrients (glucose, FFA), body fat (leptin), GI & pancreatic hormones Hypothalamus posterior: stimulation inhibits secretion and peristalsis (sympathetic) Lesions in hypothalamus can result in gastric ulcers, haemorrhage; gastric bleeding is common after intracranial operations. Higher centres: gastric erosions appear rapidly in very nervous animals. Relationship human peptic ulcers and “stress” GI tract & enteric NS: (Hirschprung's disease - defect in submucosal (Auerbach's) plexus; Crohn’s disease VIP increased Enteric NS: 107-8 neurons; control peristalsis & secretion so gut is relatively independent of CNS; trophic effects Feeding and drinking - see separate lecture URINARY TRACT Kidney Control (reduce) renal blood flow (sympathetic; α1) Control (increase) renin secretion via JGA (sympathetic; β1 ) Bladder: Afferents signal distension to sacral cord via pelvic plexus Efferents - pelvic parasympathetics (ACh; M2)) stimulates micturition sympathetic?; int sphincter? – poorly understood. (NB somatic to external sphincter) Bladder centre in sacral cord - automatic bladder in spinal animals. After spinal injury humans can learn a somatic reflex to empty bladder. Pontine inhibitory centre: develops postnatally with bladder control. GENITAL TRACT Erection - parasympathetic vasodilation; role ACh M3; NO cGMP, Viagra; VIP Emission - sympathetic - slow contraction vas, seminal vesicle smooth muscle; Ejaculation - somatic (pudendal nerve. - rapid contraction of bulbospongiosus) SLEEP There are probably are no specific sleep centres in the HT but: Hypothalamus: posterior lesions cause hypersomnia by preventing arousal; anterior lesions cause insomnia. Role of orexins in arousal; narcolepsy. Low frequency stimulation anteriorly can induce sleep; high frequency stimulation causesawakening; Lateral preoptic area lesions cause hyperactivity man & rats Dorsal hypothalamic area stimulation causes sleep and motor preparation for sleep Raphé: destruction causes insomnia; 5-HT from raphé promotes sleep. EMOTIONAL & BEHAVIOURAL RESPONSES Emotion is a feeling; other people can only observe the physical results The appearance of emotional reactions can be elicited in decorticate animals. "Sham rage" can be induced when only the hypothalamus is connected to the brain stem. Any stimulus then causes sympathetic arousal which ceases immediately the stimulus ends (cf real rage). Sham rage is abolished by a lesion of the posterior hypothalamus. The autonomic system is central to the control of many systems. Hence it appears in various places in the syllabus 8.3.3 Autonomic innervations of bronchi; 8.7.2 Asthma and its pharmacology; 8.8.2 Short-term reflex control of ABP; 8.8.6.3 Sympathetic control; 8.8.8 cardiovascular regulation in critical illness; 8.9.3 Physiological changes during exercise; 16.5.2 Orbit and eyeinternal muscles of eye; 21.7 Pupillary reflexes; 22 Cranial nerves; 23.2 Hypothalamus; 24.2 Sleep; 51.1 Functions of hypothalamus; 51.2 Physiological response to stress; 52.1 body temperature regulation; 53.2 Effects of general anaesthetics; 24.2 sleep ... and many others