inspiring stories (from Esther)
advertisement

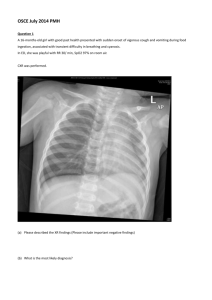
From Esther (A UK Palliative Care Nurse Specialist working with the team in 2007/2008) Victoria is a 32-year-old woman who we first met in Hospital. She was weak, emaciated and visibly short of breath. She complained of chest and abdominal pains. She had been admitted and investigated for long standing health problems and was found to be suffering from AIDS. The hospital referred Victoria to The Shepherd’s Hospice and she agreed that once she was sent home we could visit her. The day after she was discharged the team set off to find her. She lived in a remote area in the hills. We drove as close as we could in a land-rover and then had to proceed on foot. We found Victoria sitting on a mat on her veranda. She was happy to be home but still short of breath and in pain. Since coming home she had not been able to sleep due to coughing at night, she complained of chest and neck pains and was eating very little as she had oral thrush. Unfortunately, she had left hospital without her ARV drugs needed to treat her HIV infection. We promised to liaise with the Sister at the hospital to obtain her ARV drugs. She was too weak to attempt the return journey. Meanwhile we gave some medication for the pain and treatment for the thrush. Two days later the Community Health Officer returned to reassess Victoria. She was visibly stronger, eating a little food now that her mouth was healing. She now felt strong enough to make the return journey back to the hospital to get her ARV drugs. One week later, we found Victoria sitting over a pot cooking for her children. She was much stronger and her shortness of breath had also eased. She was now taking her ARV drugs. She still needed to take paracetamol for the chest pains. In view of her on-going respiratory symptoms the Doctor had requested she have a chest x-ray to rule out TB infection. She could not afford the L30,000 (£5) fee. TSH patient support fund was able to assist her and she was given L35,000 to cover the costs including a taxi fare. We await the results and continue to monitor her progress and support her as she takes her ARV drugs. ```````````````````````````````````````````````````````` Isatu is 5 years old. Her mother had brought her into the clinic at TSH. She was lying on the bed, feverish, weak and lethargic. She lived with her mother at Grafton Camp, formally a camp for displaced people during the war. Her mother was divorced, sadly Isatu’s father was not interested in his child. For over a year Isatu had been suffering from chronic health problems. Her mother had taken her to many of the local clinics, paying for tests and treatment, none of which had seemed to help. She had even paid for prayers at the local church, now her money had run out. Fortunately, another Shepherd’s Hospice patient had told her to come for help. Isatu was malnourished, she had a swollen infected eye and pus drained out of one ear. She wouldn’t speak and complained of pain in her throat on eating. The lymph nodes in her neck were enlarged, as was her liver. On examination she had reduced air intake into her lungs. Both of her feet were odematus. It was clear that she was acutely unwell and needed to be examined by a paediatrician. We were concerned that her chronic health problems maybe due to an underlying HIV infection, although her mother appeared well. We took Isatu and her mother to the local children’s hospital. On examination the Doctor decided to admit her but was concerned as to who would pay the bill? The patient support fund (PSF) was able to cover the consultation fee (£5) and laboratory fees (£2). Two days later we returned to find Isatu much improved, sitting up and able to reply to our greeting ‘Kushe’. She was smiling broadly. The laboratory tests had shown that she was anaemic but her HIV test was negative. The Doctor was concerned that she might have an underlying cardiac problem, could he order a chest x-ray? Once again the PSF was able to cover the (£5) fee. The chest x-ray revealed that she was suffering from pulmonary TB. She was commenced on treatment (free) and moved into the nutritional unit attached to the hospital. She would remain there for one month whilst she received intensive nutritional therapy and took her TB drugs. We left knowing that she would be well cared for. Five weeks later we visit Isatu in the camp. She is running around with her friends, giggling with delight. The transformation in her is amazing. Her mother thanks us, Isatu has started to talk again. She will need to continue on her TB drugs but she should make a full recovery. `````````````````````````````````````````````````````````````` John is 30 years old he has recently successfully completed treatment for TB. He knows that he is HIV positive, his first wife died of AIDS. He is keen to commence ARV treatment. He came to TSH for assistance. We pick him up from the side of the road as arranged and take him to hospital where he is commenced on Anti-retroviral treatment. His new wife does not know of his status, only his mother. A few days later, the Community Health Officer tries to visit John. He is not at home, he has been feeling ill and has gone to church for prayers. The next day we visit again. On arrival, we find John lying semi-conscious on the floor of a back bedroom. He complains of having a headache last night and today has not moved. He is unable to speak and is weak down one side of his body. His teeth are clenched together in his mouth and he moans quietly. If disturbed he stares but doesn’t appear to see. His neck is stiff. A family friend who works in another clinic has set up an intravenous drip. In the UK we would dial 999 and call for an ambulance. There is no ambulance and he is too large and unconscious to attempt to move him by car. We know that even if moved to the main hospital in Freetown, he may not receive the treatment needed to save his life. The journey would involve sitting in heavy traffic for perhaps hours in stiflingly hot conditions. His family are all too aware that they do not have the money to pay expensive hospital bills. We fear that John has meningitis, a complication of his HIV infection. We help the family understand what may be happening to John and the possible options. It is clear that they would like him to stay at home with them; they are afraid to move him. We reassure them that we will do our best to make him comfortable. We provid a Home-based Care Kit and attend to his personal hygiene needs, changing his clothes and bed sheet and laying him on incontinent sheets. We cool his body with tepid sponging and encourage his family to talk to him and keep him cool with a fan. It is impossible to give him any medication by mouth and so we administer an injection of Tramadol, the strongest pain killer that we have available in Sierra Leone. (However since October 2010 oral morphine is now available to Patients of TSH). We leave him and his family and promise to return the following day. His family seem relieved to have some support and tell us that he is now in God’s hands.