Hepatorenal Syndrome
advertisement
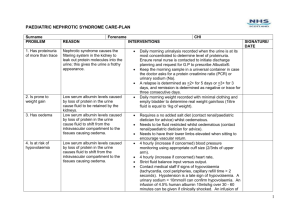
Hepatorenal Syndrome 14/8/10 PY Mindmaps E-medicine SP Notes = profound oliguria and Na+ retention in the setting of severe liver dysfunction (cirrhosis or fulminant liver failure) - usually fatal unless liver transplant performed. - RRT can prevent advancement of condition Pathophysiology -? - local production of intrarenal vasoconstrictors -> intrarenal vasoconstriction despite systemic vasodilation - increased Q with reduced SVR and MAP - hypovolaemia and raised intra-abdominal pressure may also be factors Types I – rapidly progressive 1. 2. 3. 4. 5. acute deterioration (doubling of creatinine or halving of CrCl over 2 weeks) absent renal parenchymal disease absent proteinuria no shock no history of nephrotoxic drugs II – slower onset and progression - renal failure in the context of end-stage liver disease that does not meet the criteria of type I Risk Factors - Na+ and H2O retention (urinary Na+ < 5mEq/L and dilutional hyponatraemia) - low MAP - poor nutrition - reduced GFR - high plasma renin activity - oesophageal varices - associated with infection, acute alcohol hepatitis, large volume paracentesis without albumin replacement Jeremy Fernando (2011) Investigations - concentrated urine with low Na+ (<10mol/L) few granular casts (doesn’t improve with fluid replacement) no proteinuria normal kidneys on U/S DIAGNOTIC CRITERIA - no other cause for renal failure - Na+ and H2O retention Major - chronic or acute liver disease with advanced hepatic failure + portal hypertension low GFR (Cr > 130mmol/L or CrCl < 40ml/min) absence of shock, bacterial infection and recent treatment with nephrotoxic agents no sustained improvement in renal function post 1.5 of isotonic saline proteinuria < 0.5g/day no renal tract disease on U/S Additional - urine volume < 500mL/day urine Na+ < 10mmol/L urine osmolality > plasma osmolality urine red blood count < 50 per high power field serum Na+ < 130mmol/L Management - diagnostic paracentesis (exclude SBP) - albumin - RRT - transjugular intrahepatic portosystemic shunt (TIPS) – reduces blood pressure in portal vein - liver dialysis (dialysis circuit with an albumin bound membrane to bind and remove toxins normally cleared by the liver) - IV clonidine (improves GFR) - terlipressin/octreotide – decrease portal vein pressure - liver transplant Jeremy Fernando (2011)