Nephrology - Dr. Robert Bell 2013
advertisement

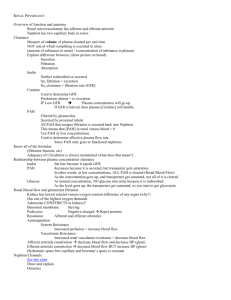
Back to Basics Nephrology 2013 Major issues in Nephrology, Electrolytes, Acid-base disturbances CKD K/DOQI Classification of Chronic Kidney Disease Stage GFR (≥3mo) Description (ml/min/1.73m2) 1 2 3 4 5 90 60-90 30-59 15-29 <15 Damage with normal GFR Mild GFR Moderate GFR Severely GFR Kidney Failure In this K/DOQI staging, “kidney damage” means: • Persistent proteinuria • Persistent glomerular hematuria • Structural abnormality: – such as PCKD, reflux nephropathy CHRONIC KIDNEY DISEASE • Diagnosis: • Acute vs. chronic: –Small kidneys on U/S or unenhanced imaging mean CKD –Diabetic CKD may still have normal sized kidneys CHRONIC KIDNEY DISEASE • Common causes of CKD: • Diabetic nephropathy • Vascular disease • GN • PKD CHRONIC KIDNEY DISEASE • Causes of CKD: • Best to divide as proteinuric or non-proteinuric CKD • Proteinuric is much more likely to have deterioration in GFR and higher cardiovascular morbidity and mortality CHRONIC KIDNEY DISEASE • Treatment • Delay progression: • Treat underlying disease i.e. good glucose control for DM • BP control to 140/90, (the current target); 130/80 for diabetics • ACEI or ARB has extra benefit for proteinuric CKD • Lower protein diet…maybe CHRONIC KIDNEY DISEASE • Treatment of the consequences of decreased GFR: – PO4: • decrease dietary intake • PO4 binders such as CaCO3 – Hypocalcemia: • CaCO3, 1,25 OH D3 CHRONIC KIDNEY DISEASE • Treatment of the consequences of decreased GFR: – Anemia: • Erythropoetin current target Hb 95105 CHRONIC KIDNEY DISEASE • Uremic Complications: Major: – Pericarditis – Encephalopathy – Platelet dysfunction ARF Click here in slide show mode Question 1 Urine values compatible with pre-renal failure: A) B) C) D) Osm < 300 mosm/L RBC casts Na+ < 20 mmol/L Fex Na+ > 2% ARF • Pre renal and ATN most common causes (quoted at 70% of cases of ARF) • DDx: – Pre Renal – Intra Renal – Post Renal Urine: Pre-Renal vs. Renal Assessment of Function U Na • Pre-Renal < 20 > 40 • ATN U Osm > 500 < 350 Fe Na < 1% > 2% U/P Na Fe Na = X 100 U/P Cr • Pigmented granular casts found in up to 70% of cases of ATN Urine: Pre-Renal vs. Renal Assessment of Function Fe Urea • Pre-Renal < 35 Fe Urea = U/P Ur X 100 U/P Cr > 55 • ATN • FeUrea might be useful to Dx pre renal ARF in those who received diuretics…but not all studies support its use. ARF • Investigations: – Pre Renal: Urine tests as noted and responds to volume – Intra-Renal: look for GN, interstitial nephritis as well as ATN – Post Renal: Imaging showing bilateral hydronephrosis is highly specific for obstruction causing ARF Dialysis: Who Needs It? • If cannot control these by other means: Hyperkalemia Pulmonary edema Acidosis Uremia • (GFR < 10-15% for CRF) Dialysis: Who Needs It? • Hemodialysis is also used for intoxications with: – – – – ASA Li Alcohols: i.e. methanol, ethylene glycol Sometimes theophylline + Na Hyponatremia • Pseudo: – If total osmolality is high: hyperglycemia/ mannitol – If total osmolality is normal, could be due to very high serum lipoprotein or protein Hyponatremia • Volume status: – Hypovolemic: high ADH despite low plasma osmolality – High total volume: CHF/ cirrhosis have decreased effective circulating volume and high ADH despite low plasma osmolality Hyponatremia • Volume status: – If volume status appears normal: • If urine osmolality is low: normal response to too much water intake…”psychogenic polydipsia” • If urine osmolality is high: inappropriate ADH Hyponatremia • Treatment: – Hypovolemic: • Replace volume – Decreased effective volume: • Improve cardiac output if possible • Water restrict – SIADH: • Water restrict Hyponatremia • Treatment: – Rate of correction of Na: • Not more than 10 mmol in first 24 h and not more than 18 mmol over first 48 h of treatment • Or Central Pontine Myelinosis may occur Potassium Hyperkalemia • Real or Not: – Hemolysis of sample – Very high WBC, PLT – Prolonged tourniquet time Hyperkalemia • Shift of K from cells: – Insulin lack – High plasma osmolality – Acidosis – Beta blockers in massive doses Hyperkalemia • Increased total body K: – Decreased GFR plus: • • • • High diet K KCl supplements ACEI/ARB K sparing diuretics – Decreased Tubular K secretion TTKG? • Requirements: – Urine osmolality > 300 – Urine Na+ > 25 – Reasonable GFR • TTKG = U/P K+/U/P Osm [urine K+ (urine osmol/serum osmol)] serum K+ <7, esp < 5 = hypoaldosteronism Hyperkalemia • Treatment – IV Ca – Temporarily shift K into cells: • Insulin and glucose • Beta 2 agonists (not as reliable as insulin) • HCO3 if acidosis present – Remove K GFR ASSESSMENT OF GFR: 1000 Creat 800 600 400 200 0 30 60 90 GFR 120 ASSESSMENT OF GFR: Creatinine clearance formula: • Cockroft-Gault estimated Creatinine clearance UCr x V PCr (140-age) x Kg x1.2 Creat (x .85 for women) Need a Steady State for these to be valid MDRD eGFR • Labs now calculate this for anyone who has a serum creatinine checked • Use serum creatinine, age, sex MDRD eGFR GFR, in mL/min per 1.73 m2 = (170 x (PCr [mg/dL])exp[-0.999]) x (Age exp[-0.176]) x ((Surea [mg/dL])exp[-0.170]) x ((Albumin [g/dL])exp[+0.318]) where SUrea is the serum urea nitrogen concentration; and exp is the exponential. The value obtained must be multiplied by 0.762 if the patient is female or by 1.180 if the patient is black. Simplified: GFR, in mL/min per 1.73 m2 = 186.3 x ((serum creatinine) exp[-1.154]) x (Age exp[-0.203]) x (0.742 if female) x (1.21 if African American) Do NOT memorize this formula Limitations of GFR estimates: Not reliable for: • extremes of weight or different body composition such as post amputation, paraplegia • acute changes in GFR • use in pregnancy • eGFR greater than 60ml/min/1.73m2 Proteinuria Proteinuria • Albumin vs. other protein – Dipstick tests albumin PROTEINURIA • Quantitative: – 24 hour collection – ACR: random albumin to creatinine ratio – PCR: random protein to creatinine ratio PROTEINURIA • Microalbuminuria: less than dipstick albumin • Can use albumin to creatinine ratio on random urine sample… best done with morning urine sample Normal Random Urine ACR (g/mol) 24h Urine Albumin (mg/24h) Random 24h Urine Urine PCR Protein (g/mol) (mg/24h) M <2.0 F <2.8 <30 <20 MicroM 2.0-30 albuminuria F 2.8-30 30-300 Macroalbuminuria >300 >30 <200 Question 2 The definition of nephrotic syndrome includes: : A)Hypolipidemia B)Lipiduria C)24 hr protein ≥2g D)hypertension Nephrotic Syndrome • Definition: – > 3 g proteinuria per day – Edema – Hypoalbuminemia – Hyperlipidemia and lipiduria are also usually present Nephrotic Syndrome • Causes: – Secondary: DM, lupus – Primary: • Minimal change disease • FSGS • Membranous nephropathy Nephrotic Syndrome • Complications: – Edema – Hyperlipidemia – Thrombosis…with membranous GN and very low serum albumin Nephrotic Syndrome • Treatment: – Treat cause if possible – Treat edema, lipids – Try to decrease proteinuria Hematuria Hematuria • Significance: ≥3 RBC's per hpf • DDx: Is it glomerular or not? • Glomerular: – RBC casts – Dysmorphic RBCs in urine – Coinciding albuminuria may indicate glomerular disease Hematuria • Other investigation: – Imaging of kidneys – Serum creatinine – Age over 40-50 rule out urologic bleeding, i.e. urine cytology and referral for cystoscopy Hematuria • For glomerular hematuria without proteinuria DDx includes: – IgA nephropathy – Thin GBM disease – Hereditary nephritis Ca++, PO4, Mg++ Ca++ and PO4- Decreased GFR and increased PO4 Decreased Ca 1 OH of 25-OHD3 Increased PTH Renal osteodystrophy Magnesium • Hypomagnesemia: – GI loss/lack of dietary Mg – Renal loss: • Diuretics • Toxins esp cisplatin Hypophosphatemia • Shift • Decreased total body PO4 – GI loss/decreased intake – Renal loss • Fanconi Syndrome? – Very rare renal tubular loss of: • PO4, amino acids, glucose, HCO3- Question 3 Most likely cause of Na 140 Cl 110 HCO3 10 : A) B) C) D) RTA serum albumin 20 resp alkalosis ketoacidosis Acid-Base • Approach to: – Resp or metabolic – Compensated or not – If metabolic: anion gap or not – Anion gap = Na - (Cl + HCO3) Acid-Base Increased anion Gap acidosis: • “MUDPILES”: – Methanol – Uremia – Diabetic/alcoholic ketosis – Paraldehyde – Isopropyl alcohol – Lactic acid – Ethylene glycol – Salicylate Acid-Base Metabolic acidosis with normal serum anion gap can be due to: 1) GI losses of HCO3 2) Renal tubular acidosis Renal Tubular Acidosis Hopefully will not need this. Normal renal response to acidosis is to increase ammoniagenesis and more NH4 will be found in the urine For those with close to normal GFR, the “urine anion gap” is a way to estimate urinary NH4 Urine anion gap = urine (Na+ + K+ – Cl-) If it is positive there is decreased NH4+ production and likely a renal component to the acidosis AKI