Regulatory Aspects of Developmental & Reproductive Toxicology
advertisement

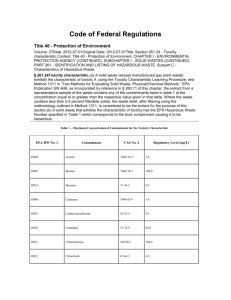
The University of North Carolina at Chapel Hill Toxicology 207: Advanced Toxicology Regulatory Aspects of Developmental and Reproductive Toxicology Rochelle W. Tyl, Ph.D., DABT Senior Fellow Developmental and Reproductive Toxicology (DART) Senior Director, DART Studies RTI International Research Triangle Park, NC (e-mail: rwt@rti.org) Monday, December 4, 2006 9:00 - 9:50 a.m. 2304 McGavran-Greenberg 1 Regulated Materials 1. U.S. FDA (Food and Drug Administration) a. Food additives (preservatives, dyes, etc.) b. Vitamins (not "natural products") c. Food substitutes i. Fat substitutes ii. Artificial sweeteners d. Pharmaceuticals e. Veterinary pharmaceuticals f. Food use pesticides g. Food use chemicals (chemical wrapping, artificial sausage skins, etc.) h. Medical devices NOTE: Attention to mechanism, disease state, clinical trials (IND, NDA) 2. U.S. EPA (Environmental Protection Agency) a. U.S. FIFRA (Federal Insecticide, Fungicide and Rodenticide Act) i. Pesticides ii. Food use pesticides iii. Biological pesticides (e.g., "BT" - Bacillus thuringensis) iv. Biochemical pesticides v. Engineered plants (transgenic plants make pesticides) NOTE: Attention to nontarget species, environmental migration (contamination) (registration, re-registration) b. U.S. TSCA (Toxic Substances Control Act) i. Commodity chemicals -- ii. paints, paint thinners, inks, plasticizers, plastics, medical supplies, PVC piping, solvents, carpets, car parts, etc. Options -- test rules -- negotiated test agreement -- voluntary submissions/programs (e.g., HPV [High Production Volume] initiative) NOTE: Minimal information required for PMN, SNUR; EPA has 90 days to respond 2 Drug Discovery and Development (NIDA TR&D Preclinical Workshop, 6/20/00) Typical Toxicity Studies and Costs Per Compound A. Basic Acute Studies for Initial Review 1. Acute iv range-find in rats $12,000 2. Acute oral (po) range-find in rats 12,000 3. Definitive oral (po) study 35,000 4. 14-day, range-find in rats 75,000 5. 16-day MTD and 14-day fixed dose study in dogs 80,000 6. Ames assay (mutagenicity/carcinogenicity) 3,000 TOTAL B. $217,000 Additional Studies for IND 1. 28-day study in rats with two-week recovery $80,000 2. 28-day study in dogs with two-week recovery 200,000 3. Battery of three mutagenicity studies 100,000 4. Cardiovascular study with cpd alone in dog 45,000 5. GI motility and renal tests in rats 25,000 6. Acute drug interactions between cpd and (e.g., cocaine, ethanol, morphine) in rodents 110,000 Cardiovascular interaction between cpd and (e.g., cocaine) in unrestrained dogs 350,000 7. TOTAL C. $945,000 Studies to Go to Phase IIa 1. Segment II in rats $90,000 2. Segment II in rabbits 110,300 TOTAL D. $200,000 Studies to Initiate NDA 1. 90-day study in rats $218,000 2. 90-day study in dogs 400,000 TOTAL E. $618,000 Studies to Complete NDA 1. Segment I and III reproduction in rats $348,000 2. One-year study in dogs 639,000 3. Two-year carcinogenicity study in rats 980,000 4. Two-year carcinogenicity study in mice 980,000 TOTAL $2,947,000 GRAND TOTAL $5,545,000 3 New Millenium Drug Discovery and Development (NIDA Div. Treatment, Research, and Development: Preclinical Workshop, 6/20/00) Off Patent Patent Target Hit Lead SAC Proj. Structure Activity Correlations HTS In Silico Combinational Safety and PK Testing Libraries "Computational Toxicology" Chem/Phys/PK Properties In Vitro SAC Tox and PK Carcinogenicity Predictions Testing "e - R&D" IND NDA Investigational New Drug Application New Drug To Market $$ Phase IV Preclinical Safety/PK Postmarketing Surveillance In Vivo Efficacy/Toxicity Pharmacoeconomics Safety Phase In Vitro I In Vivo Healthy Volunteers Pharmacology Earlier Failures and Improved SACs Microarrays Pharmacogenomics Proteomics Time: 8-13 years Cost: $350-600 M OTC II III Pilot Clinical Patients Trials $$ 4 5 Developmental Toxicity Testing Soon after the thalidomide disaster in the late 1950s and early 1960s, the U.S. FDA assumed regulatory responsibilities for requiring specific testing paradigms "for the appraisal of safety of new drugs for use during pregnancy and in women of childbearing potential.”1. A letter was sent from the Chief of the Drug Review Branch, U.S. FDA, to all corporate medical directors,1 establishing what became known as the Guidelines for Reproductive Studies for Safety Evaluation of Drugs for Human Use. These guidelines (Figure 1) encompassed three test intervals: Phase I (Segment I), with prebreeding and mating exposures, to provide information on possible effects on breeding, fertility, implantation, pre- and postimplantation development (Figure 1A); Phase II (Segment II), with exposures during major organogenesis, to provide information on possible effects on in utero survival and morphological growth and development, including teratogenesis (Figure 1B); and Phase III (Segment III), with exposures from the onset of the fetal period through weaning of the offspring, to provide information on parturition, lactation, late intrauterine (fetal) and postnatal growth and development, puberty, and reproductive function of F1 offspring (Figure 1C). The procedures for Segment II studies have essentially been followed by the U.S. EPA, 2,3,4 Japan,5 Canada,6 Great Britain,7 and the OECD.8 6 Figure 1. FDA Segment I, II, and III Studies A. SEGMENT I: FERTILITY STUDY G PBE - 28-70 days Q M - 14 days F0 Males gd 0 gd 7 gd 13-15 N F0 Females and F1 Litters PBE - 14 days Q F0 Females EC N F0 Males Information on: breeding, fertility, nidation, and pre- and postimplantation development B. SEGMENT II: DEVELOPMENTAL TOXICITY STUDY G gd 0 gd 6 gd 15 N gd 17-18 (mice) or 20-21 (rats) Q M rodent females gd 6-15 G gd 0 gd 6-7 gd 18-19 N gd 29-30 Q M rabbit females Information on: maternal toxicity, embryotoxicity, fetotoxicity, teratogenicity C. SEGMENT III: PERINATAL AND POSTNATAL STUDY G Q L W M F0 females G gd 0 gd or 6 gd 15 parturition (pnd 0) PWHP (F1) pnd 21 DL VP PPS L M EC F1 females gd 0 pnd 0 N F2 pups pnd 4 N F1 males and females N F0 females Information on: maternal toxicity, in utero growth and development, parturition, lactation, postnatal growth and development, puberty, reproductive functions of offspring Direct exposure to adults No exposure Q = Quarantine M = Mating G = Gestation gd = gestational day L = Lactation W = Wean N = Necropsy pnd = postnatal day PBE = Prebreed exposure period DL = Developmental landmarks VP = Acquisition of vaginal patency PPS = Acquisition of preputial separation EC = Estrous cyclicity (for F0 females in Segment I and F1 females in Segment III) PWHP = Postwean holding period (minimum 49 days; F1 offspring at least 70 days old at end of period) 7 Recently, attempts have been made to make testing guidelines for reproductive and developmental toxicity studies consistent among major nations. The International Conference on Harmonization (ICH), representing the U.S. (FDA), the European Community (EC), and Japan, has promulgated testing guidelines for registering pharmaceuticals within the three regions.9 They are similar to the original FDA guidelines and assess exposure during prebreeding, mating, and gestation, until implantation on gestational day 6 (Study 4.1.1), exposures from implantation to weaning (Study 4.1.2), exposures only during organogenesis (Study 4.1.3), and combined single and two-study designs. ICH Study 4.1.3 is, in fact, identical to the U.S. FDA Segment II study, and ICH Study 4.1.2 is similar to the U.S. FDA Segment III study, except that exposures start at the beginning of organogenesis instead of at the end. Draft guidelines 10 and final guidelines17 from the U.S. EPA, OPPTS (Office of Prevention, Pesticides and Toxic Substances) for developmental toxicity studies have also recently been promulgated, and the U.S. EPA TSCA Final Guidelines15. The U.S. FDA19 and OECD21 have also recently revised their guidelines. The Segment II study had traditionally been termed a “teratology study,” since the initial focus was on structural malformations (terata). It is currently more appropriately termed a “developmental toxicity study,” as it evaluates (and the term "developmental toxicity" encompasses) a spectrum of possible in utero outcomes for the conceptus, including death, malformations, deficits (usually functional), and developmental delays. It is important to note that a Segment II Study evaluates only structural growth and development of offspring and only during in utero development. The parameters assayed are fetal body weights and the appearance of external, visceral, and skeletal structures. For example, if the organs are the right size, shape, and color, and in the correct location, they are judged to be normal. There is no assessment for microscopic integrity or function and no way to assess functional effects that might have occurred (or become evident) during postnatal life if the fetuses had been born (these concerns are addressed by different testing paradigms). A comparison of the old and new testing guidelines for developmental toxicity assessment is as follows. 8 Differences Between Old and New Developmental Toxicity Test Guidelines MATERNAL ENDPOINTS Event/Parameter Previous Requirementsa Current Requirementsb Maternal Evaluations Assignment to dose group Not specified Assignment by a body weight dependent random procedure Definition of high dose level Should induce some overt maternal toxicity, but not more than 10% maternal deaths Should induce developmental and/or maternal toxicity, but not more than 10% maternal deaths Test substance administration: period of dosing During the major period of organogenesis: days 6-15 in rodents and 6-18 (or 7-19 FIFRA) in rabbits Dose from implantation through termination (days 6-20 or 21 in rats, 6-17 or 18 in mice, and 6-29 or 30 in rabbits): option to begin on GD 0; ICH retains original dosing period21 Test substance administration: dose adjustment Dosage based upon the body weight at the start of test substance administration or adjusted periodically by body weight Dosage adjusted periodically throughout the period of administration by body weight Number of pregnant animals at termination (presumed pregnant animals assigned to study) Rodents: 20 per group Rabbits: 12 per group Rodents and rabbits: 20 litters per group (females with implantation sites at termination) Maternal postmortem data: ovarian corpora lutea counts Data required for all species except mice (TSCA only) Data required for all species (including mice) Rodents: Assignment of fetuses for evaluation One-third to one-half of each litter assigned for skeletal evaluation, the remainder for visceral evaluation One-half of each litter assigned for skeletal evaluation, the remainder for visceral evaluation Rabbits: Coronal sectioning Not required Required (50% serial sections, 50% coronal sections) Ossified and cartilaginous skeletal evaluation Only ossified specified (alizarin red S stain) Both ossified and cartilaginous skeletal examination required (unspecified method of staining; usually alizarin red S for ossified bone and alcian blue for cartilaginous bone and other structures), all species Fetal Evaluations a Requirement under FIFRA, TSCA, and FDA b OPPTS (EPA TSCA and FIFRA) Draft Guidelines, Public Draft, February 1996, and Final Guidelines “Prenatal Developmental Toxicity Study OPPTS 870.3700”, TSCA Final Guidelines 799.9370 (August 15, 1997), FDA Guidelines 9 All previous governmental testing guidelines specified exposure beginning after implantation is complete and continuing until the completion of major organogenesis. This corresponds to gd 6 through 15 for rodents and gd 6 through 18 (FDA and TSCA) or gd 7 through 19 (FIFRA) for rabbits, if the day of impregnation is designated gd 0. In a departure from the previous guidelines, recently released draft10 and final17,19 developmental toxicity testing guidelines specify exposure during the entire gestational period, from gd 0 through scheduled sacrifice at term or from gd 6 to term. The rationale for starting exposures after implantation is complete is based on two possible confounding scenarios: 1. If the initial (parent) test material is teratogenic and the metabolite(s) is not, and if metabolism is induced by exposure to the parent compound, then exposure beginning earlier than implantation (with concomitant induction of enzymes and enhanced metabolism) will result in the conceptuses being exposed to less of the teratogenic moiety, and the study may be falsely negative. 2. If the test chemical and/or metabolites interferes with implantation, then exposure prior to implantation will result in few or no conceptuses available for examination11. However, there are situations when initiation of exposure should begin prior to completion of implantation. These include: 1. For exposure regimens that are anticipated to result in slow systemic absorption; e.g., cutaneous application, subcutaneous insertion, or dosing via feed or water, steady-state, maximal blood levels may not be attained until the very end (or beyond) of organogenesis if exposures begin on gd 6 or 7. 2. For materials which are known to have accumulative toxicity (due to build-up of chemical and/or insult) after repeated exposures, exposure should begin on gd 0 (or earlier) so that the conceptuses are developing in a fully affected dam. 3. For materials, which are known to deplete essential components, such as vitamins, minerals, cofactors, etc., exposures should begin early enough so that the dam is in a depleted state by the start of organogenesis (or by gd 0). 4. For materials, which are innocuous as the parent chemical but which are metabolized to teratogenic forms, exposures should begin early enough so that postimplantation conceptuses are exposed to maximal levels of the teratogenic metabolites. 5. For materials which are known not to interfere with pre-implantation growth and development or with implantation11. 10 The termination of exposures was specified as the end of major organogenesis. It is signaled by the closure of the secondary palate and the change in designation of the conceptus from embryo to fetus. The cessation of exposure allows for a postexposure recovery period for both the dam and the fetuses, and an assessment can be made regarding whether the observed maternal effects (body weights, clinical observations) are transient or permanent. However, fetal evaluations generally take place at term, and there is no commonly employed way to detect early adverse effects on the conceptus that resolve (are repaired or compensated for) earlier in gestation. What is observed at term is the net result of the original insult and any repair or compensation that occurred subsequently in the conceptus, and a detailed evaluation of the dam after a post-exposure period (i.e., no detailed information of the dam during the exposure period). In addition, exposure until term includes the period of male fetal reproductive system differentiation in utero which begins on gd 13-14 in rodents so possible endocrine disrupters may be detected. These considerations may be the basis for the requirement in the new U.S. EPA OPPTS draft10 and final,17 and the U.S. FDA19 and OECD21 final developmental toxicity testing guidelines (Figure 2) for exposure continuing until terminal sacrifice. 11 Interestingly, the recent ICH testing guidelines9 have retained the maternal exposures only during major organogenesis. 11 Figure 2. New U.S. EPA, OECD, and FDA Prenatal Developmental Toxicity (“Segment II”) Study Exposure Durations OPPTS 1996 Draft Guidelines; Final Guidelines, 1998 (870.3700); and TSCA Final Test Guidelines, 1997 (799.9370); U.S. FDA Guidelines (2000); OECD Guidelines G GD 0 Q GD 6 M N GD 17-18 (mice) GD 20-21 (rats) GD 29-30 (rabbits) N fetuses at term OR G GD 0 Q GD 6 M N GD 17-18 (mice) GD 20-21 (rats) GD 29-30 (rabbits) N fetuses at term Key: Q = Quarantine M = Mating G = Gestation N = Necropsy GD = gestational day Direct exposure of dams/does Possible indirect exposure of conceptuses via transplacental transfer of parent compound and/ or metabolites No exposure 12 Figure 3. ICH Study Designs A. Study of Fertility and Early Embryonic Development (4.1.1), Rodent (see Phase I) F0 males PBE Q 4 weeks F0 females G Q M GD 0 GD 6 GD 15 GD 20 3 weeks N F0 males OR N N F0 females F0 females Assess: Maturation of gametes, mating behavior, fertility, preimplantation, implantation B. Study for Effects on Prenatal and Postnatal Development, Including Maternal Function (4.1.2), Rodent (see Phase III) G Q M GD 0 L W selected F1 pups M G pnd 4 N L F1 females and F2 litters pnd 21 GD 6 parturition pnd 0 Assess: N F0 females N F1 males Toxicity relative to nonpregnant females, prenatal and postnatal development of offspring, growth and development of offspring, functional deficits (behavior, maturation, reproduction) C. Study for Effects on Embryo-Fetal Development (4.1.3), Rodent and Nonrodent (see Phase II) G GD 0 Q M N F0 females and F1 litters on GD 20 GD 6 GD 15 Assess: Toxicity relative to nonpregnant females, embryo/fetal death, altered growth of offspring, and structural changes of offspring in utero 13 FIGURE 3 (continued) D. Single Study Design (4.2), Rodents (combine 4.1.1 and 4.1.2) F0 males Q PBE M F0 females Q GD 0 G 3 weeks pnd 21 GD 20 N F0 males L W pnd 21 selected F1 pups M G N 1/2 F0 females and F1 litters N F1 females and F2 litters N F1 males N 1/2 F0 females and F1 litters E. Two-Study Design (4.3), Rodents 4.1.1 with 4.1.2: 1/2 F0 females and F1 litters necropsied on GD 20 1/2 F0 females and F1 litters necropsied on pnd 21 (retained selected F1 pups followed through mating and gestation of F2 litters) Q= PBE = M= G= L= W= N= GD = pnd = Quarantine Prebreed Exposure Period Mating Gestation Lactation Wean Necropsy Gestational Day Postnatal Day Direct exposure of adults 14 Reproductive Toxicity Testing The U.S. FDA Segment I and III studies have been essentially combined in the U.S. EPA-mandated reproductive toxicity testing guidelines for both TSCA12 and FIFRA13 since 1985 (graphically presented in Figure 4). The proposed U.S. EPA OPPTS draft17 and final18 guidelines (and the TSCA final testing guidelines16) (Figure 5), the U.S. FDA final guidelines (Figure 6), and the OECD 41622 final guidelines have the same overall design, but have included additions to improve the sensitivity of the study design, to assess reproductive endpoints (structural and functional) in a robust animal model (the rat), with special attention to detection of possible endocrine disrupters. All current study designs include a long prebreed exposure period for the initial animals (designed the F0 generation), beginning after weaning to encompass at least one complete spermatogenic cycle, mating, gestation, and lactation with exposures continuing, culling litters (designated F1) on pnd 4 to a fixed size, necropsy of parental animals, retention of selected F1 pups for a long prebreed with mating, gestation, and lactation of F2 litters as in the first generation, with termination of the study at the weaning of the F2 litters. The F1 generation is the one generation, which has the potential for exposure beginning as gametes (in the F0 parents) through their reproductive performance. (In contrast, F0 animals begin exposures at 5-9 weeks of age, and F2 animals are potentially exposed from gametes through lactation, all indirect through their parents, the F1 generation.) A comparison of the old and new testing guidelines for reproductive toxicity assessments is as follows. 15 Figure 4. Previous Two-Generation Study Design (EPA) Q PBE M G L F0 M G L W PBE M G L M G L W F1 F2 KEY: Q = Quarantine PBE =Prebreed exposure M = Mating G = Gestation L = Lactation W = Weaning Direct exposure Possible indirect exposure via placental and/or lactational transfer Direct and possibly indirect exposure if test material is in the diet or drinking water as pups begin to self-feed and self-drink by third week of lactation 16 Figure 5. New Two-Generation Study Design (EPA, FDA, and OECD and FDA)a PBE Q M G L F0 N F0 females ECE N F0 males M G L W PBE M G L F1 N F1 females NW S VP PPS N F1 males ECE M G LW F2 NW AGD S a EPA18 and FDA20 provide for a possible second litter per generation (i.e., F1a and F1b; F2a and F2b). KEY: Q = Quarantine PBE =Prebreed exposure M = Mating G = Gestation L = Lactation W = Weaning N = Necropsy ECE = Estrous cyclicity evaluations S = Standardize litters on pnd 4 to 8-10 VP = Acquisition of vaginal patency PPS = Acquisition of preputial separation AGD = Measurement of anogenital distance in F2 pups on pnd 0 if "triggered" NW = Necropsy F1 and F2 weanlings, up to three/sex/litter Direct dietary exposure Possible indirect exposure from transplacental and/or translactational exposure Both direct and possible indirect exposure if test material is in feed or drinking water (nursing pups begin self-feeding and self-drinking in last week of lactation) 17 Figure 6 FDA Two-Generation Reproduction and Teratology Study (FDA Redbook 2000, IV.C.9.a) Timeline (weeks) 0 F0 2 4 6 8 10 10-week PBE Q 12 14 16 18 P L M 20 22 24 26 28 30 32 34 36 38 40 H M 42 44 N F0 females N F0 males G P L W 10-week PBE M G P L G F1a gd 20 VP PPS S G Developmental Landmarks Optional: P L W F2a N S AGD -- Type I immunotoxicity in F0 dams and F1 male and female offspring -- Functional Type II immunotoxicity testing in retained F0 parents, or satellite F1 and/or F2 postweanlings -- Neurotoxicity screening in offspring (F1 and/or F2a) Q= N= necropsy PBE = prebreed exposure quarantine (1 wk) W= weaning (on pnd 21) M= mating (2 wks) S= standardize litters to ten pups (with equal sex ratio) on pnd 4 G= gestation (3 wks) H= holding period between breedings L= lactation (3 wks) P= parturition (delivery) gd = gestational day PPS = acquisition of preputial separation in F1a males AGD = measurement of anogenital distance on pnd 0 VP = acquisition of vaginal patency in F1a females N F1 males G F2b N F1a dams and F2b fetuses on gd 20 Use for optional teratology study 18 BUT, there are criticisms: 1. Current guidelines only follow one offspring/sex/litter to adulthood. Will we miss subtle lesions or effects at low incidence? Should more pups per litter be retained postwean? This will not improve statistical power since that is based on live numbers of litters/group, but it will improve the characterization of parameters for each litter. 2. Current guidelines trigger anogenital distance in F2 offspring if effects on reproductive development are detected in F1 offspring (e.g., delays in acquisition of puberty, alterations in estrous cyclicity, etc.). Since F2 offspring are terminated at weaning, effects on AGD in F2 newborn pups cannot be related to any postwean effects such as puberty, estrous cycling, adult reproductive system structures, or functions. Easy fix: Measure AGD in F1 animals, which are thoroughly evaluated through sexual maturity and reproduction. AGD is considered the most sensitive indicator of anti-androgenic activity and can be a good (but not perfect) predictor of effects in older animals and/or at higher doses. 3. Current test guidelines do not specify examination of preweanling males for retained nipples and/or areolae (indicator of anti-androgen activity) or preweanling females for decreased nipples or areolae (from androgenic activity). Easy fix: Examine F1 and F2 preweanlings (pnd 11-13) for number of nipples and/or areolae. 4. Current testing guidelines do not require use of a positive control group (or “reference chemical”). Use of positive control (successfully) indicates the animal model is sensitive to perturbation in endpoints of concern, and that the performing laboratory is competent to detect effects if they occurred. There is no prohibition of its use… 5. Current testing guidelines do not require assessment of hormone levels in the blood. Most mammalian hormones are released into circulation in a pulsatile pattern with additional diurnal and seasonal rhythms. A single blood sample taken at necropsy may not be informative. Multiple samples over time under basal and challenge conditions will be much more useful, but this would require cannulated animals or multiple tail sticks, etc., which could confound the assessment of treatment-related reproductive effects. In addition, hormonal changes are the basis for regulation of homeostatis. They are supposed to change in response to changes in the external or internal environment and are not adverse, per se. The consequences, if any, from altered hormone levels are the endpoints of concern. A separate study or a satellite group or groups is highly recommended for these assessments. 19 NEW RISK ASSESSMENT/RISK MANAGEMENT PARADIGM Science-Based Risk Assessment Scientific Research Laboratory and Field Observations/Measurements Risk Management Development of Regulatory Options Toxicity Assessment Extrapolation Methods Linked Databases RA Identifies Research Needs Risk Characterization Cell Signaling Pathway Research Gene-Environment Research Genomics/Proteomics Population Characterization Public Health, Social, Ethical, Economic, Political Implications New Research Informs RA Exposure Assessment Modified from: NRC, 2000; Scientific Frontiers in Developmental Toxicity and Risk Assessment Regulatory Decision(s) Implementation 20 COMPARISON OF HAZARD ASSESSMENT 1. Hazard: “Intrinsic capacity of the test chemical to do harm” 2. Basic research VERSUS RISK ASSESSMENT 1. Risk: The probability that exposure to the test chemical -- by relevant routes of administration -- small numbers/group -- at doses down to environmentally relevant levels -- typically high doses -- during susceptible periods of development (in utero, -- strange and wonderful routes 3. Identify (and validate) new endpoints perinatal, peripubertal, adult, senescent) will result in adverse outcome(s) -- cell signaling pathways 2. Science-based risk assessment -- gene-environment interactions -- robust study designs -- “-omics” (e.g., genomics, proteomics, metabolomics) -- large numbers/group 4. New research informs risk assessment -- range of doses 5. These studies are not used for risk assessment -- relevant routes, timing -- use of validated endpoints 3. Involves both toxicity and exposure assessments -- if hazard is high but no exposure, then no risk -- if hazard is low but ubiquitous in environment, then likely high risk 4. Risk assessment identifies new research needs 5. Risk characterization regulatory decisions (risk mgmt.) 20 REFERENCES 1 Goldenthal, E. I. (Chief, Drug Review Branch, Division of Toxicological Evaluation, Bureau of Scientific Standards and Evaluation), Guidelines for Reproduction Studies for Safety Evaluation of Drugs for Human Use, March 1, 1966. 2 U.S. Environmental Protection Agency (EPA), Toxic substances control act (TSCA) test guidelines: Final rule, Federal Register, 50, 39412, 1987. 3 U.S. Environmental Protection Agency (EPA), Pesticides assessment guidelines (FIFRA), subdivision F. Hazard Evaluation: Human and Domestic Animals, Section 83-3 (Final Rule). Available from NTIS (PB86-108958), Springfield, VA, 1984. 4 U.S. Environmental Protection Agency (EPA), Pesticide assessment guidelines, subdivision F hazard evaluation: humans and domestic animals, series 83-3, rat or rabbit developmental toxicity study, June, 1986 (NTIS PB86-248184), as amended in Federal Register 53(86), Section 158.340, May 4, 1988. 5 Japanese Guidelines of Toxicity Studies, Notification No. 118 of the Pharmaceutical Affairs Bureau, Ministry of Health and Welfare. 2. Studies of the Effects of Drugs on Reproduction, Yakagyo Jiho Co., Ltd., Tokyo, Japan, 1984. 6 Canada Ministry of Health and Welfare, Health Protection Branch, The testing of chemicals for carcinogenicity, mutagenicity and teratogenicity. The Ministry of Ottawa, 1973. 7 United Kingdom, Committee on Safety of Medicines: Notes for guidance on reproduction studies, Department of Health and Social Security, Great Britain, 1974. 8 Organization for Economic Cooperation and Development (OECD), Guideline for Testing of Chemicals: Teratogenicity, Director of Information, Paris, France, 1981. 9 Food and Drug Administration (FDA) (1994). International Conference on Harmonisation (ICH); Guideline for Detection of Toxicity to Reproduction for Medicinal Products; Availability; Notice. Section 4.1.3, Study for Effects on Embryo-Fetal Development. Federal Register 59(183), 48749, September 22, 1994. 10 U.S. EPA (1996). OPPTS (Office of Prevention, Pesticides and Toxic Substances) Health Effects Test Guidelines, OPPTS 870.3700, Prenatal Developmental Toxicity Study (Public Draft, February, 1996). 11 _ Tyl, R. W. and Marr, M. C. (1996). Chapter 7. Developmental Toxicity Testing Methodology, In: Handbook of Developmental Toxicology (R. D. Hood, Editor), CRC Press, Inc. (September, 1996). 12 U.S. EPA (1985). Toxic Substances Control Act, EPA (TSCA) Section 798.4700, Reproduction and Fertility Effects. Federal Register 50 (188), 39432-39433 (September 23, 1985). 13 U.S. EPA (1989). Federal Insecticide, Fungicide, and Rodenticide Act (FIFRA) EPA Guidelines for Pesticide Registration (Subdivision F, Hazard Evaluation: Human and Domestic Animals, Section 845), August 17, 1989. 14 U. S. EPA (1996). Office of Prevention, Pesticides and Toxic Substances (OPPTS), Health Effects Test Guidelines, OPPTS 870.3800, Reproduction and fertility effects (Public Draft February, 1996). 21 15 U.S. EPA (1997). Toxic Substances Control Act Test Guidelines; Final Rule 40 CFR Part 799.9370 “TSCA prenatal developmental toxicity.” Federal Register 62(158), 43832-43834 (August 15, 1997). 16 U.S. EPA (1997). Toxic Substances Control Act Test Guidelines, Final Rule 40 CFR Part 799.9380 “TSCA reproduction and fertility effects.” Federal Register 62(158), 43834-43838 (August 15, 1997). 17 U.S. EPA (1998). Office of Prevention, Pesticides and Toxic Substances (OPPTS). Health Effects Test Guidelines OPPTS 870.3700, Prenatal Developmental Toxicity Study; Final Guideline, August 1998. 18 U.S. EPA (1998). Office of Prevention, Pesticides and Toxic Substances (OPPTS). Health Effects Test Guidelines OPPTS 870.3800, Reproduction and Fertility Effects; Final Guideline, August 1998. 19 U.S. FDA (2000). Center for Food Safety and Applied Nutrition Redbook 2000. IV.C.9.b. Guidelines for Developmental Toxicity Studies. July 20, 2000. 20 U.S. FDA (2000). Center for Food Safety and Applied Nutrition Redbook 2000. IV.C.9.c. Guidelines for Reproductive Studies. July 20, 2000. 21 OECD (2001). OECD Guideline for the Testing of Chemicals; Proposal for Updating Guideline 414: “Prenatal Developmental Toxicity Study,” pp. 1-11, adopted January 22, 2001. 22 OECD (2001). OECD Guideline for the Testing of Chemicals; Proposal for Updating Guideline 416: “Two-Generation Reproduction Toxicity Study,” pp. 1-13, adopted January 22, 2001.