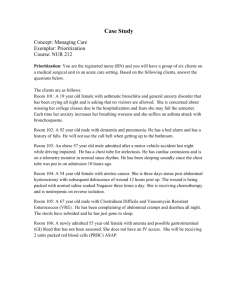
Oxygen Needs
advertisement

Oxygen Needs Altered function of any system affects oxygen needs. Oxygen needs are affected by: • • • • • • • • • • • • • • Respiratory system status Circulatory system function Red blood cell count Nervous system function Aging Exercise Fever Pain Drugs Smoking Allergies Pollutant exposure Nutrition Alcohol Patients at Risk for Poor Oxygenation Hypoxemia Insufficient oxygen in the blood Patients at risk Immobile Cardiac or pulmonary disease Risk Factors for Poor Oxygenation Postoperative Sleep apnea Morbidly obese Neuromuscular disease Decreased consciousness Kyphoscoliosis ALTERED RESPIRATORY FUNCTION Respiratory function involves three processes. • Air moves into and out of the lungs. • O2 and CO2 are exchanged at the alveoli. • The blood carries O2 to the cells and removes CO2 from them. Hypoxia means that cells do not have enough oxygen. • Anything that affects respiratory function can cause hypoxia. • The brain is very sensitive to inadequate O2. • Hypoxia is life-threatening. Adults normally have 12 to 20 respirations per minute. • They are quiet, effortless, and regular. • Both sides of the chest rise and fall equally. Tachypnea is rapid breathing. • Respirations are 24 or more per minute. Bradypnea is slow breathing. • Respirations are fewer than 12 per minute. Apnea is the lack or absence of breathing. Hypoventilation means respirations are slow, shallow, and sometimes irregular. Hyperventilation means respirations are rapid and deeper than normal. Dyspnea is difficult, labored, or painful breathing. With Cheyne-Stokes respirations: • Respirations gradually increase in rate and depth. • Then they become shallow and slow. • Breathing may stop (apnea) for 10 to 20 seconds. Orthopnea means breathing deeply and comfortably only when sitting. Biot’s respirations are rapid and deep respirations followed by 10 to 30 seconds of apnea. Kussmaul respirations are very deep and rapid respirations. ASSISTING WITH ASSESSMENT AND DIAGNOSTIC TESTS Altered respiratory function may be an acute or chronic problem. The doctor orders tests to find the cause of the problem. • • • • • • Chest x-ray (CXR) Lung scan Bronchoscopy Thoracentesis Pulmonary function tests Arterial blood gases (ABGs) Pulse oximetry measures the oxygen concentration in arterial blood. • The normal range is 95% to 100%. • A sensor attaches to a finger, toe, earlobe, nose, or forehead. • An alarm sounds if: • O2 concentration is low • The pulse is too fast or slow • Other problems occur • A good sensor site is needed. • Use SpO2 when recording the oxygen concentration value: • S = saturation • p = pulse • O2 = oxygen Pulse Oximeter Measures oxygen saturation of hemoglobin 95% to 100% - normal Below 90% - complications Below 85% - probable hypoxemia 70% or below - life-threatening emergency Pulse Oximeter Monitor the patient! Many variables interfere with accurate values! PROMOTING OXYGENATION To get enough oxygen, air must move deep into the lungs. • Air must reach the alveoli, where O2 and CO2 are exchanged. Measures to meet oxygen needs are found in care plans. Positioning • Breathing is usually easier in semi-Fowler’s and Fowler’s positions. • Persons with difficulty breathing often prefer the orthopneic position. • Frequent position changes are needed. Deep breathing and coughing • Deep breathing moves air into most parts of the lungs. • Coughing removes mucus. • Deep-breathing and coughing exercises: • Help persons with respiratory problems • Are done after surgery and during bedrest • Help prevent pneumonia and atelectasis The goal of incentive spirometry is to improve lung function. • Atelectasis is prevented or treated. Capillary Refill Indication of the peripheral circulation Cyanosis (problem with oxygen delivery) Skin Nailbeds Mucous membranes Lips Capillary Refill Capillary refill varies with age, but will return to normal within 2 to 3 seconds. Check capillary refill on all four extremities Oxygen Therapy Pressure gauge shows the amount of oxygen in the cylinder Never modify a gauge or part to make it fit! Humidification is not necessary in liter flows below 5 Chain tank to a carrier or base Oxygen Therapy Avoid sparks, post oxygen signs Remove smoking materials Follow all safety precautions ASSISTING WITH OXYGEN THERAPY Oxygen is treated as a drug. The doctor orders: • The amount of oxygen to give • The device to use • When to give it The person may need: • Oxygen constantly • Oxygen for symptom relief You do not give oxygen. • You assist the nurse in providing safe care. Oxygen is supplied as follows: • Wall outlet • Oxygen tank • Oxygen concentrator • Liquid oxygen system These oxygen devices are common: • Nasal cannula • Simple face mask • Partial-rebreather mask • Non-rebreather mask • Venturi mask Talking and eating are hard to do with a mask. Moisture can build up under the mask. • Keep the face clean and dry. • Masks are removed for eating. The oxygen flow rate • The flow rate is the amount of oxygen given. • It is measured in liters per minute (L/min). • The nurse or respiratory therapist sets the flow rate. • When giving care and checking the person: • Always check the flow rate. • Tell the nurse at once if it is too high or too low. • Know your center’s policy about nursing assistants adjusting oxygen flow rates. Oxygen administration set-up • If not humidified, oxygen dries the airway’s mucous membranes. • Distilled water is added to the humidifier. • Bubbling in the humidifier means that water vapor is being produced. You assist the nurse with oxygen therapy. • You do not give oxygen. • You do not adjust the flow rate unless allowed by your state and center. Suction Patient cannot breathe during suctioning Do not exceed 10 seconds for suctioning, insertion, and removal A Yankauer (tonsil tip) is used for mouth and throat Flexible catheter is used for the nose, mouth, and throat Persons who cannot cough or whose cough is too weak to remove secretions need suctioning. These routes are used to suction the airway: • Oropharyngeal • Nasopharyngeal • Lower airway If not done correctly, suctioning can cause serious harm. • Hypoxia and life-threatening problems can occur. • Cardiac arrest can occur. • Infection and airway injury are possible. Small Volume Nebulizer A nebulizer converts liquid medicine into a mist Loosens and lubricates secretions It may be large, small, ultrasonic, or placed inside ventilator tubing Continuous Positive Airway Pressure CPAP maintains positive pressure during the respiratory cycle Pressure opens partially or fully closed alveoli Provides more surface area for gas exchange Improves oxygenation and prevents premature airway closure Bilevel Positive Airway Pressure BiPAP is similar to CPAP Maintains positive airway pressure during inspiration and expiration Higher pressure during inhalation Reduces pressure during exhalation BiPAP reduces effort of breathing Postural Drainage Drains secretions from lungs For patients with cystic fibrosis or certain types of pneumonia Can be used to treat other conditions PCT assists with positioning patient Advanced Respiratory Procedures ASSISTING WITH RESPIRATORY THERAPY Some persons need artificial airways, suctioning, mechanical ventilation, and chest tubes. The goals for respiratory rehabilitation are to help the person: • Reach his or her highest level of function • Live as independently as possible • Return home Artificial airways keep the airway patent (open). • Intubation means inserting an artificial airway. These airways are common: • Oropharyngeal airway • Endotracheal (ET) tube • Tracheostomy tube Care for persons with artificial airways involves: • Vital signs are checked often. • Observe for hypoxia and other signs and symptoms. • If an airway comes out or is dislodged, tell the nurse at once. • Frequent oral hygiene is needed. • Follow the care plan. Persons with ET tubes cannot speak. (Some tracheostomy tubes allow speech.) • Follow the care plan. • Always keep the signal light within reach. Caring for an Intubated Patient Elevate head Turn head to one side Suction oral secretions Provide oral and nasal care Reposition at least every 2 hours Monitor for and prevent pressure ulcers Caring for an Intubated Patient Monitor vital signs and capillary refill Monitor insertion site for redness, irritation, or breakdown Monitor for signs of respiratory distress Reassure the patient and family Develop a method for communicating with the patient Tracheostomies are temporary or permanent. • A tracheostomy has three parts (the obturator, the inner cannula, and the outer cannula). • The cuffed tracheostomy tube is used for mechanical ventilation. • The tube must not come out (extubation). • The tube must remain patent (open). • Call for the nurse if: • You note signs and symptoms of hypoxia or respiratory distress • The outer cannula comes out • Nothing must enter the stoma. • Follow Standard Precautions and the Bloodborne Pathogen Standard when assisting with tracheostomy care. The care of a tracheostomy involves: • Cleaning the inner cannula to remove mucus and keep the airway patent • Cleaning the stoma to prevent infection and skin breakdown • Applying clean ties or a Velcro collar to prevent infection When secretions collect in the upper airway, they can: • Obstruct airflow into and out of the airway • Provide an environment for microbes • Interfere with O2 and CO2 exchange Usually, coughing removes secretions. Caring for a Tracheostomy Patient Some patients breathe room air Others use a ventilator or a bag valve mask Tracheostomy care is a sterile procedure Keep the stoma and cannula clean Caring for a Tracheostomy Patient Secure the outer cannula Prevent water and objects from entering the lungs Prevent infection Caring for a Laryngectomy Patient Deep breathing and coughing every 2 hours Monitor the patient’s skin color Watch for: Cyanosis Color changes in nailbeds or mucous membranes Respiratory distress Caring for a Laryngectomy Patient Watch for: Restlessness Dyspnea Anxiety Increased heart rate Lethargy Disorientation Chest Tubes The doctor inserts chest tubes to remove air, blood, or fluid from the pleural space. • Pneumothorax is air in the pleural space. • Hemothorax is blood in the pleural space. • Pleural effusion is the escape and collection of fluid in the pleural space. • Chest tubes attach to a drainage system. • Water-seal drainage keeps the system airtight. Caring for a Chest Tube Patient Keep bottle lower than heart Make sure that nothing pulls on tube Keep tube taped to chest Keep junction of chest and drainage tube taped together Position drainage system upright Reposition patient every 2 hours Caring for a Chest Tube Patient Keep the tube patent Coil tubing on the bed Don’t disconnect a drain connected to a vacuum regulator Keep patient mobile Keep oxygen and suction at bedside Keep emergency equipment in room Caring for a Chest Tube Patient Inform RN of abnormal signs or symptoms If chest tube comes out, cover site with 4 x 4 gauze or petroleum gauze If a drainage bottle breaks, clamp proximal tube with a rubber-tipped clamp Mechanical Ventilation Mechanical ventilation may be needed for a variety of health care problems. • Mechanical ventilation is started in the hospital. • Alarms sound when something is wrong. • When any alarm sounds on a mechanical ventilator: • First check to see if the person’s tube is attached to the ventilator. If not, attach it to the ventilator • Then tell the nurse at once about the alarm. • Do not reset alarms. • Persons needing mechanical ventilation are very ill. Caring for a Mechanically Ventilated Patient Make sure the alarm is on at all times Respond immediately Provide oral and nasal care Monitor mucous membranes for pressure, irritation, and breakdown Caring for a Mechanically Ventilated Patient Observe for changes Respiratory rate and depth Shortness of breath Use of accessory muscles Caring for a Mechanically Ventilated Patient Count spontaneous respirations and ventilator‑ delivered breaths Check for tube displacement Make sure the tube is taped securely Visually inspect the chest Should appear symmetrical Caring for a Mechanically Ventilated Patient Monitor patient for pain Elevate head 60 to 90 Elevation of head of the bed increases risk of skin breakdown on the torso Elevate heels off surface of bed Suction, if permitted