Chapter 9
advertisement
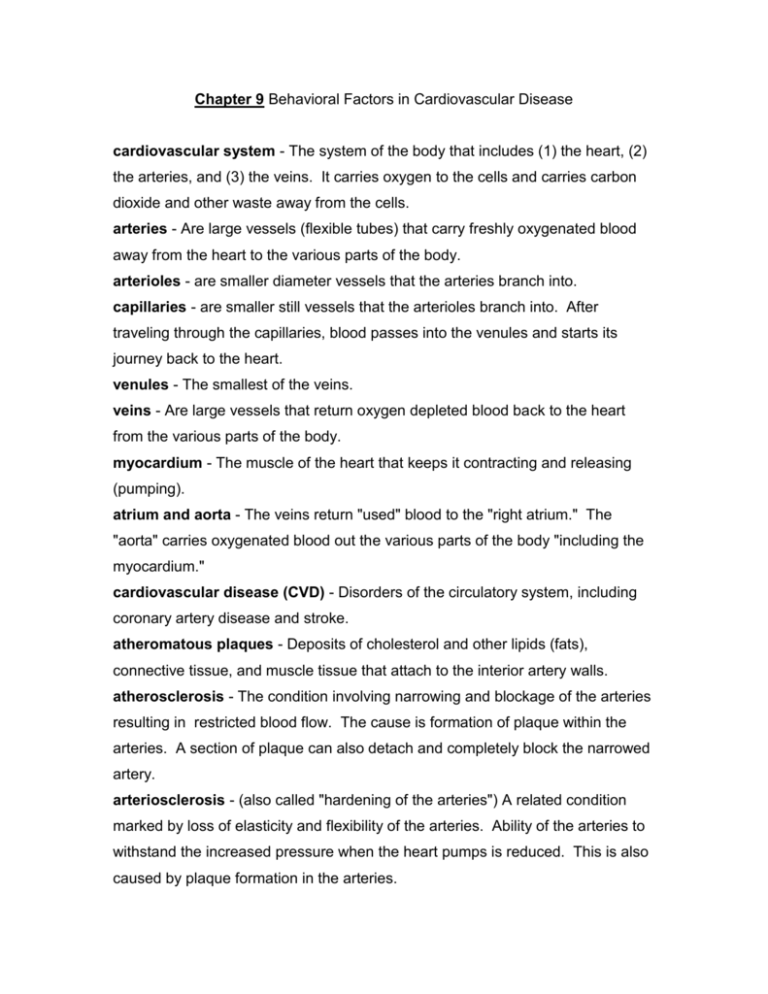
Chapter 9 Behavioral Factors in Cardiovascular Disease cardiovascular system - The system of the body that includes (1) the heart, (2) the arteries, and (3) the veins. It carries oxygen to the cells and carries carbon dioxide and other waste away from the cells. arteries - Are large vessels (flexible tubes) that carry freshly oxygenated blood away from the heart to the various parts of the body. arterioles - are smaller diameter vessels that the arteries branch into. capillaries - are smaller still vessels that the arterioles branch into. After traveling through the capillaries, blood passes into the venules and starts its journey back to the heart. venules - The smallest of the veins. veins - Are large vessels that return oxygen depleted blood back to the heart from the various parts of the body. myocardium - The muscle of the heart that keeps it contracting and releasing (pumping). atrium and aorta - The veins return "used" blood to the "right atrium." The "aorta" carries oxygenated blood out the various parts of the body "including the myocardium." cardiovascular disease (CVD) - Disorders of the circulatory system, including coronary artery disease and stroke. atheromatous plaques - Deposits of cholesterol and other lipids (fats), connective tissue, and muscle tissue that attach to the interior artery walls. atherosclerosis - The condition involving narrowing and blockage of the arteries resulting in restricted blood flow. The cause is formation of plaque within the arteries. A section of plaque can also detach and completely block the narrowed artery. arteriosclerosis - (also called "hardening of the arteries") A related condition marked by loss of elasticity and flexibility of the arteries. Ability of the arteries to withstand the increased pressure when the heart pumps is reduced. This is also caused by plaque formation in the arteries. coronary artery disease (CAD) - Atherosclerosis and/or arteriosclerosis in the coronary arteries resulting in reduced flow of blood to the heart (myocardium). Ischemia - is the technical term for artery blockage and restricted blood flow. coronary heart disease (CHD) - This conditions involves actual damage to the myocardium due to insufficient blood supply. myocardial infarction - is the technical term for a "heart attack." The cause is death of myocardial tissue due to loss of blood supply. Reduced vigor and stamina may require lifestyle adjustments (assuming one survives). cardiac rehabilitation - A group of approaches (often involving psychologists) designed to help heart patients (1) adjust lifestyle, (2) reduce risk factors, and (3) avoid future attacks. angina pectoris - A less severe condition involving restricted blood supply to the myocardium. The symptoms are "crushing" pain in chest and difficulty breathing which often (but not always) follow exertion or stress. stroke - is the name for damage to the brain resulting from lack of oxygen (death of brain cells will occur within "3 to 5 minutes" of oxygen loss). Stroke is typically the result of cardiovascular disease. common stroke - is caused by a clot (blockage), most often in a vessel that has been narrowed by atherosclerosis (plaque formation). hemorrhagic stroke - is caused by bleeding in the brain due to a rupture of a weakened vessel. Cells can die (1) because their blood supply is lost OR (2) from pressure due to the escaping blood. blood pressure - is the most common measurement of cardiovascular functioning, probably because of its ease and convenience. The degree to which the pressure raises a column of mercury in a glass tube indicates the pressure (just like a barometer with air pressure). systolic blood pressure - The "first" number, a measure of the blood pressure generated by the heart’s contraction. diastolic blood pressure - The "second" lower number, a measure of blood pressure between contractions of the heart. hypertension - Abnormally "high blood pressure" (resting). According to our text (numbers approximate), up to 120 systolic and 80 diastolic are "normal" blood pressure. Up to 140 / 90 would be Prehypertension, up to 160 / 100 Stage 1 Hypertension, and above that, Stage 2 Hypertension. Hypertension is the "single best predictor of both heart attack and stroke." The delicate blood vessels of the "retinas" are at risk from the increased pressure as are other body parts. essential (primary) hypertension - High blood pressure that has no easily discernable cause. Genetics and environment likely play important roles. secondary hypertension - High blood pressure that can be identified as the result of other diseases (e.g., kidney disease). It is much "less common" than essential hypertension. electrocardiogram (ECG) - is a measure of the electrical activity of the heart during "rest." An abnormal ECG indicates cardiac problems BUT cannot detect plaque buildup or hardening of the arteries (CAD). stress test - measures the electrical activity of the heart under increasing levels of exercise test to diagnose coronary artery disease. Inefficient oxygen supply due to artery blockage will produce a characteristic pattern. Thus, this is a more sensitive and useful test than is the ECG. angiography - The most definitive (but invasive) test for diagnosing CAD. A catheter is snaked through a blood vessel to the heart. A dye is then injected so that X-ray pictures can clearly show artery blockage. It is considered the "gold standard" of diagnosis. Unfortunately, it is uncomfortable or even painful, frightening, and carries a slight risk of death. angioplasty - A catheter with an inflatable balloon tip is passed into an obstructed artery. The tip is then inflated in order to flatten atherosclerotic deposits of plaque and, at least temporarily, open up blocked arteries. The procedure is now fairly routine. stent - a metal tube which can be inserted into the artery after angioplasty to keep the artery open. cardiovascular death rates - in the U. S. rose dramatically between 1920 and the 1960s. It then began a steady decline (when graphed, the pattern forms an "inverted U function" or bell curve). The decline is due to two factors: (1) improved emergency treatment, and (2) changes in lifestyle (better diet, more exercise, etc.). the Framingham Heart Study - identified a number of now well recognized risk factors back in the 1960s and, along with the 1964 Surgeon General's Report on Smoking, likely led to many of the post 1960s lifestyle changes that have helped reduce heart disease in the U. S. increasing rates of cardiovascular disease - In contrast to the U. S., rates are increasing in Russia and other Eastern European areas of the former Soviet Union. All factors are not understood but higher rates of smoking and increased alcohol use are two. inherent risk factors - are things that are not easily changed such as genetics and the presence of various physical conditions. advancing age - is the primary risk factor (inherent or otherwise) for cardiovascular disease. With each 10 years of age, risk of cardiovascular disease more than doubles. demographic factors - Risk of CVD for men is about twice that for women. Native, Asian, and Hispanic Americans are at less risk than European Americans who are, in turn, at less risk than African Americans. For African Americans, discrimination leads to hypertension which, in turn, leads to CVD. cholesterol - fatlike lipoproteins that comes from animal fats and other sources. They are necessary (in small quantities) to human life. low-density lipoprotein (LDL) - "Bad cholesterol" is a form of lipoprotein thought to cause coronary artery disease. high-density lipoprotein (HDL) - "Good cholesterol" is a form of lipoprotein that confers some protection against coronary artery disease. triglycerides - very low density (VLDL) lipoproteins. High levels are thought to cause coronary artery disease. total cholesterol to HDL Ratio - yields a number that provides a "snapshot" of one's cholesterol profile. A lower number is more favorable with a ratio of "4 or less" being desirable. behavioral factors - Cigarette smoking is the leading behavioral risk factor for cardiovascular death in the U. S. Other risks include obesity (esp. with a large amount of abdominal fat), a diet high in saturated (animal) fats, and sedentary lifestyle. psychosocial factors - Lower level of education is a risk factor via association with other risks such as smoking. Higher income, social support, and (one of my favorites) having a pet can have beneficial effects. personality - seems to be less of a factor than intuition would suggest. In the 1970s, cardiologists Friedman and Rosenman identified a CHD prone personality pattern which they called "Type A." Later research indicated that only hostility and anger were the relevant personality factors (and even these are NOT major factors). Neither violent expression of anger nor holding anger in (suppression) is an effective strategy. Experts suggest calm expression of anger. Anger, badly handled, can lead to cardiovascular reactivity (CVR). cardiovascular reactivity (CVR) - An increase in blood pressure and heart rate as a reaction to frustration or harassment. cardiologist - A medical doctor who specializes in the diagnosis and treatment of heart disease. Dean Ornish - Achieved some degree of fame when his super low fat (less than 10%) vegetarian diet actually resulted in a "decrease" in arterial plaques among his research patients. Unfortunately, such a program is extraordinarily difficult to stay with.