Duarte et al revised FRBM submission
advertisement

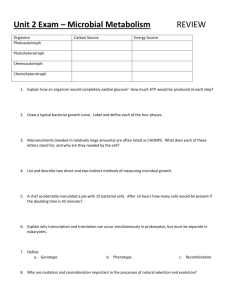
ORIGINAL CONTRIBUTION Gene expression profiling reveals new protective roles for vitamin C in human skin cells Tiago L. Duarte1,2*, Marcus S. Cooke1,3, George D. D. Jones1 1 Radiation & Oxidative Stress Group, Department of Cancer Studies & Molecular Medicine, University of Leicester, Leicester, LE1 7RH, U.K. 2 Iron Genes & Immune System Group, IBMC – Instituto de Biologia Molecular e Celular, Universidade do Porto, 4150-180 Porto, Portugal. 3 Department of Genetics, University of Leicester, Leicester, LE1 7RH, U.K. *To whom correspondence should be addressed. Iron Genes & Immune System Group, Instituto de Biologia Molecular e Celular, Rua do Campo Alegre 823, 4150-180 Porto, Portugal. Tel.: +351 226074956. Fax: +351 226098480. E-mail address: tduarte@ibmc.up.pt 1 Abstract: The skin is a protective barrier against external insults and any lesion must be rapidly and efficiently repaired. Dermal fibroblasts are the major source of extracellular connective tissue matrix and play an important role in wound healing. Vitamin C is an important water-soluble free radical scavenger and an essential co-factor for collagen synthesis by dermal fibroblasts, and consequently may contribute to the maintenance of a healthy skin. Using microarray analysis, we investigated the effects of long-term exposure to a stable vitamin C derivative, ascorbic acid 2-phosphate (AA2P), in contact-inhibited populations of primary human dermal fibroblasts. When comparing with ‘scorbutic’ cells, exposure to AA2P increased the expression of genes associated with DNA replication and repair, and with G2/M phase of the cell cycle. Consistent with the gene expression changes, AA2P increased the mitogenic stimulation of quiescent fibroblasts by serum factors and cell motility in the context of wound healing. Furthermore, AA2P-treated fibroblasts showed faster repair of oxidatively damaged DNA bases. We propose that vitamin C may protect the skin by promoting fibroblast proliferation, migration and replication-associated base excision repair of potentially mutagenic DNA lesions, and we discuss the putative involvement of hypoxia inducible transcription factor-1 (HIF-1) and collagen receptor-related signalling pathways. Keywords: Ascorbic acid; Fibroblast; Gene expression; DNA repair; 8-oxoguanine; Wound healing; Cell proliferation; Cell migration. 2 Introduction Human skin consists of two tissue layers, namely a keratinized stratified epidermis and an underlying thick layer of collagen-rich dermal connective tissue. The skin serves as a protective barrier against external insults and therefore any lesion must be rapidly and efficiently repaired. Wound healing is a complex process consisting of several consecutive and overlapping phases: inflammation, cell proliferation and migration, extracellular matrix deposition and wound contraction [1]. Dermal fibroblasts are the major source of extracellular connective tissue matrix and they play an important role in wound healing. They are recruited to the wound area by inflammatory cells, invade lesions and play an important role in promoting re-epithelialization and re-establishing tissue integrity. Consequently, cultured fibroblasts have been incorporated into various tissue-engineered products that are used in the clinics for skin regeneration [2]. Fibroblasts that are found at sites of lesions proliferate more and more actively secrete extracellular matrix components such as collagens and fibronectin [1]. Solar ultraviolet radiation is a genotoxic agent and considered to be the principal cause of skin carcinogenesis. UVB is directly absorbed by DNA bases, leading to damage, such as pyrimidine dimers, but has limited penetrance into the epidermis. In contrast, UVA radiation is known to reach the dermal layer, where damage is formed indirectly, either by energy transfer reactions, or the formation of reactive oxygen species (ROS) [3]. Singlet oxygen, formed by the excitation of cellular photosensitisers and transfer of energy to molecular oxygen, reacts with DNA molecule forming, almost exclusively, 7,8-dihydro-8-oxo-guanine (8-oxoGua) [4], which is mutagenic [5]. Vitamin C is an important free radical scavenger and 3 therefore it may protect the skin against ROS-mediated damage. It is also a co-factor for prolyl and lysyl hydroxylation, required for collagen maturation [6] and ceramide synthesis [7]. Whilst vitamin C can stimulate the differentiation of several mesenchymal cell types (reviewed by [8]), it seems to be associated with a higher proliferation rate in skin fibroblasts. Recently, it was shown that the addition of a stable vitamin C derivative, magnesium Lascorbic acid 2-phosphate (AA2P), to the cell culture medium led to an increase in dermal fibroblast number and a better organization of the basement membrane zone in an in vitro human reconstructed skin model [9]. We previously shown that vitamin C modulates intracellular iron metabolism and affects the expression of iron-related genes in fibroblasts from human skin [10]. In the present work, we aimed at elucidating additional role(s) of vitamin C in these cells by performing a genome-wide expression profiling analysis of vitamin C-replete versus ‘scorbutic’ cells (i.e. cells depleted of vitamin C by serial propagation in culture without the addition of the vitamin). Dermal fibroblasts do not exhibit a rapid proliferating activity in vivo, except when exposed to certain stimuli, e.g. during wounding. Therefore, a system where cells enter a nondividing state but still keep the ability to divide when exposed to several stimuli would represent a better model of these cells in vivo. In vitro, this can be achieved according to two well-established drug-independent methods: serum deprivation and cell contact inhibition [11]. We made primary human fibroblasts quiescent by growing them to a post-confluence density and incubated them with ascorbic acid (AA) or AA2P for up to 5 days, with daily repletion, to study the basal gene expression profiles associated with a long-term exposure to vitamin C. We have previously shown that, whilst AA is unstable and its auto-oxidation generates H2O2 in culture media, the amount of H2O2 produced by physiological 4 concentrations of AA ( 100 µM) is not toxic to confluent fibroblast monolayers. AA2P, on the other hand, does not generate H2O2 in cell culture media [12]. We hypothesised that with the above-mentioned approach we would gain new insights on the participation of vitamin C in important processes in human skin, such as wound healing or the repair of oxidative DNA lesions in skin cells. Materials and Methods Reagents Minimal Essential Medium with Earle’s salts and non-essential amino acids, foetal bovine serum (FBS) and Glutamax-I were purchased from Invitrogen (Paisley, UK). Magnesium salt of AA2P (C6H6O9P 3/2 Mg; Figure 1) was obtained from Wako Pure Chemical Industries (Neuss, Germany). All other chemicals and reagents were purchased from Sigma-Aldrich (Poole, UK) unless otherwise stated. Cell culture conditions GM5659 primary fibroblasts established from a skin biopsy of an apparently healthy donor were obtained from the NIGMS Human Genetic Cell Repository (Coriell Institute for Medical Research, New Jersey, USA). Cells were grown as a monolayer culture in Nunclon culture flasks at 37 °C in a humidified atmosphere containing 5 % CO2. Fibroblasts were grown in Minimal Essential Medium with 2 mM Glutamax-I and 10 % FBS. Cells were passaged when nearly confluent and all experiments were performed at passage numbers 14-17. Cells were grown to confluence prior to the experiments. 5 Millimolar solutions of AA and AA2P were freshly prepared and sterilised by passing through a 0.22 µm membrane immediately prior to the experiments. Solutions were then diluted in pre-warmed medium to obtain the desired concentrations. Post-confluent fibroblasts were supplemented with 100 µM AA or AA2P added fresh every day for a period of up to 5 days. Control cells received medium alone. Gene expression profiling Total-RNA was extracted using TRI Reagent, according to the manufacturer’s instructions. A second RNA cleanup was performed using the RNeasy Mini kit (QIAGEN, Crawley, UK). RNA concentration was determined by measuring the absorbance at 260 nm and integrity was investigated in the Agilent 2100 Bioanalyzer using the Eukaryote Total RNA Nano assay (Agilent Technologies, Palo Alto, California, USA). Total RNA (6 µg) was reverse transcribed into double stranded cDNA with an oligo-dT primer using the One-cycle cDNA Synthesis Kit (Affymetrix, Santa Clara, California, USA) and cleaned up using the Affymetrix Sample Cleanup Module. Synthesis of biotin labelled cRNA was performed by in vitro transcription using the Affymetrix IVT labelling kit, followed by cRNA cleanup with the Affymetrix Sample Cleanup Module. Size distribution of the labelled transcripts was investigated in the Agilent 2100 Bioanalyzer. Fragmented, biotin-labeled cRNAs (20 µg) were hybridised to GeneChip Affymetrix Human U133 Plus 2.0 arrays for 16 hr at 45 °C with rotation at 60 rpm. Probe array washing and staining were performed according to Affymetrix EukGE-WS2v5 Gene Chip protocol in the Fluidics Station 400. Probe arrays were scanned at 570 nm using an Affymetrix GeneChip scanner and the fluorescence intensity of the scanned image registered in CEL intensity files. DNA-Chip Analyser (dChip) software [13] was used 6 to automatically select probes, detect outliers/artefacts, normalise the fluorescence intensity over multiple arrays and calculate model-based expression values from the differences between perfect match and mismatch probes in the cell intensity files. The data have been deposited in NCBI’s Gene Expression Omnibus (GEO, http://www.ncbi.nlm.nih.gov/geo/) and are accessible through GEO Series accession number GSE11919. In addition, dChip software was used to filter a set of AA- and AA2P-responsive genes for which the expression levels were significantly altered in the triplicate experiments (t-test, P<0.01), with an average fold change ≥2 or ≤-2 when comparing with the control groups and a difference in average fluorescence intensity >50. Real-time RT-PCR Real-time reverse transcription-PCR (RT-PCR) was performed on the MX4000 spectrofluorometric thermal cycler (Stratagene, Amsterdam, Netherlands) as described previously [10]. The amplification protocol consisted of denaturation at 95 °C for 4 min and 40 cycles of 95 °C for 30 sec, annealing temperature for 1 minute and 72 °C for 30 sec. Amplification conditions and primer sequences are listed in Table 1. The quantity of each transcript was estimated against the respective standard curve and normalised against the quantity of the endogenous control gene, Hypoxanthine phosphoribosyltransferase 1 (HPRT1). The final gene expression value in each treated sample was subsequently determined as a ratio of the gene expression in the control sample. Cell cycle analysis 7 Cells were fixed in 70 % ethanol at approximately 1 × 106 cells/ml and kept at 4 °C for a minimum of 24 hr. Prior to analysis, cells were centrifuged at 600 × g for 10 min and resuspended in phosphate-buffered saline with 0.1 mg/ml RNase A and 5 µg/ml propidium iodide. Following incubation at room temperature for 30 min, 10,000 cells were acquired in a FACScan flow cytometer (Becton Dickinson, Oxford, UK). The proportion of cells in the different phases of the cell cycle was calculated from the histogram of number of cells per propidium iodide fluorescence intensity with ModFitLT v2.0 software (Verity Software House, Topsham, Maine, USA). Cell viability assay Cell viability was measured by analysis of propidium iodide uptake and cell size by flow cytometry, exactly as described previously [10]. Wound healing assay The migratory behaviour of control and AA2P-treated cells was assessed in an in vitro wound healing assay. Fibroblasts were grown to confluence and incubated with 100 µM AA2P added fresh every day for a period of 3 days. Control cells received medium alone. An artificial wound was created with a 200 µl micropipette tip. After washing each culture to remove debris, cells were further incubated with AA2P or growth medium for 24 hr. Fibroblast migration was assessed by measuring the distance between wound edges, by means of an inverted microscope. DNA repair assay 8 Cells were incubated with phosphate-buffered saline containing 0.4 µM Ro 19-8022 (Roche, Basel, Switzerland) and irradiated on ice at 35 cm distance from a 500 W halogen lamp to induce oxidative modification of DNA via 1O2. The repair of 8-oxoGua was subsequently monitored using the human 8-oxoguanine DNA glycosylase 1 (hOGG1) comet assay (hOGG1 comet) [14] with substantial modifications. After trypsinisation, cells were suspended in 0.6 % low melting point agarose. Eighty microliters of the agarose gel (containing approximately 2 × 104 cells) were dispensed onto glass microscope slides previously coated with 1 % normal melting point agarose. The agarose was allowed to set on ice under a coverslip and the slides left overnight in ice-cold lysis buffer (100 mM disodium EDTA, 2.5 M NaCl, 10 mM Tris-HCl, pH 10 containing 1 % triton X-100 added fresh). Slides were washed once with distilled water and immersed in two changes of enzyme digestion buffer [40 mM HEPES, 0.1 M KCl, 0.5 mM EDTA and 0.2 mg/mL bovine serum albumin (pH 8.0)], for 5 min each time, at room temperature. In preliminary experiments, hOGG1 (New England Biolabs, Hitchin, UK) was added to the gel (50 µL/gel) at different dilutions, to achieve optimal concentration. Gels were covered with a cover slip and incubated in a humidified chamber at 37 ºC for 45 min. The cover slips were removed and the slides were placed in a horizontal electrophoresis tank. From this step onwards, the assay was performed exactly as described [14]. DNA damage was expressed as the percentage of DNA in the comet tails. Statistical analysis Data are expressed as mean values ± standard deviation for at least 3 independent samples. Statistical evaluation was performed using Minitab software (Minitab Ltd, Coventry, UK). 9 Differences among multiple groups were compared by one-way analysis of variance with posthoc Tukey’s test. Unless otherwise stated, statistical significance was assumed at P < 0.05. Results Gene expression profiling Our previous work confirmed that primary dermal fibroblasts become depleted of vitamin C (i.e. ‘scorbutic’) following serial propagation in vitamin C-free medium. Incubating fibroblasts with the stable vitamin C derivative AA2P, however, leads to a dose- and timedependent intracellular accumulation of AA, with a concentration plateau being reached between 12 and 24 hr of incubation [10]. In the current work, we incubated confluent fibroblasts with either 100 µM AA2P or AA added fresh every day at 24-hour intervals for a period of up to 5 days, to maintain a constant level of intracellular AA repletion. Using this model, we did not see a reduction in cell viability when incubating cells with AA2P or AA at 20-500 µM (cell viability >96 %), which agrees with our previous findings [12]. Visual inspection of the cultures revealed that, whilst control cells remained a tightly packed, 2dimensional monolayer, with only minimal cell overlap after 5 days of incubation in growth medium, cells incubated with AA2P or AA exhibited post-confluent growth, as indicated by a much higher cell density and extensive cell overlap (data not shown). The ability of vitamin C to induce post-confluent growth of skin fibroblasts has been previously described [15-17]. To identify genes whose expression was altered by continued exposure to vitamin C, we grew GM5659 human dermal fibroblasts to confluence and subsequently incubated them with 100 M AA2P for 5 days with daily repletion, as mentioned above. Control cells were 10 given fresh medium without AA2P. Affymetrix high-density oligonucleotide DNA microarray analysis was employed to investigate the genome-wide expression profiles of treated and control (scorbutic) cells. The expression of 294 genes and expressed sequence tags was significantly modulated by AA2P with at least 2-fold induction or repression in 3 independent experiments (P<0.01). Genes were grouped according to the Gene Ontology functional categories (Table 2 and supplementary table 1). AA2P induced about 20 genes that promote the passage through the different phases of the cell cycle by regulating the transitions of G1 to S phase and G2 to M phase, including several cyclins and cyclin-dependent kinases. Also upregulated was a cluster of genes that are essential components of the cellular DNA replication machinery, such as primase, DNA polymerase alpha 1, DNA topoisomerase 2 alpha (TOP2A) and replication factors. Some of the genes in this group are also known to be involved in DNA repair, like RAD51 homolog, flap structure-specific endonuclease 1 (FEN1) or nei endonuclease VIII-like 3 (NEIL3). Furthermore, AA2P increased the expression of nearly 40 genes that are associated with the mitotic phase of the cell cycle, including genes encoding chromosome segregation and spindle associated proteins. Altogether, these results agree with the ability of AA2P to promote the proliferation of contact-inhibited fibroblasts. This may also explain the fact that AA2P increased the expression of genes involved in lipid and steroid biosynthesis, including a key regulator of cholesterol synthesis, the low-density lipoprotein receptor (LDLR). In fact, cells that are undergoing mitotic division have a higher demand of free cholesterol and fatty acids for the synthesis of new membranes, and hence express more LDLR than quiescent cells [18-19]. On the other hand, AA2P repressed the expression of genes involved in glucose metabolism, including the glucose transporter 1 (GLUT1), which is involved in the cellular 11 uptake of the oxidised form of AA, dehydroascorbate, . Furthermore, AA2P caused a 2-fold down-regulation of a gene involved in iron uptake, transferrin receptor (TFRC), as previously described [10], and reduced the expression of 4 members of a family of negative regulators of transcription, inhibitor of DNA binding 1-4. In addition, AA2P modulated the expression of genes involved in extracellular matrix remodelling and cell adhesion, as well as genes encoding cytoskeleton proteins. A comprehensive list of all significant expression changes is presented in supplementary table 1, which also contains results from AA-incubated fibroblasts. The expression profiles of fibroblasts incubated with 100 µM AA were almost identical to those obtained with AA2P (supplementary table 1), which is not surprising given the fact that both vitamin C derivatives yield similar intracellular ascorbate levels [10], and that the pro-oxidant effect of AA in culture media is minimised when cells are at a high density [12]. The microarray results were validated by confirming the expression of genes involved in G2 to M phase transition (cyclin B1, CCNB1), DNA replication/repair (TOP2A, FEN1, NEIL3), lipid metabolism (LDLR), iron metabolism (TFRC) and glucose metabolism (GLUT1) by real-time quantitative RT-PCR. This independent technique confirmed that all selected genes were significantly modulated by AA or AA2P in the same fashion as in the microarray analysis (Figure 2). If at all different, the expression changes had slightly higher amplitude in the RT-PCR analysis, which is probably due to the higher sensitivity of the assay. Cell cycle re-entry 12 Our gene expression profiling results showed that AA and AA2P modulate cell cycle progression and thus stimulate the post-confluent growth of contact-inhibited fibroblasts. In vivo, skin fibroblasts are only exposed to serum growth factors during the process of wound healing, where resting fibroblasts are required to proliferate. Therefore, we wondered whether AA2P would stimulate quiescent fibroblasts to re-enter the cell cycle when exposed to a mitogenic stimulus. For this purpose, nearly confluent fibroblasts were made quiescent by serum starvation (0.5 % FBS) for 48 hr. This protocol arrests cells at the G0/G1 phase of the cell cycle, but these cells can be stimulated to re-enter the cell cycle by exposure to serum (10 % FBS) [20]. As depicted in Table 3, over 96 % of the serum starved cells were at the G0/G1 phase of the cell cycle. Culture medium was subsequently replaced with fresh low-serum medium (0.5 % FBS) or complete growth medium (10 % FBS) and cells were further incubated for 24 hr. As expected, cells that were returned to low-serum medium for further 24 hr remained arrested at G0/G1. In contrast, a proportion of the cells that were returned to complete growth medium re-entered the cell cycle, as indicated by an increase in the percentage of cells in S and G2/M phases. The addition of AA2P with low-serum medium did not change cell cycle arrest at G0/G1. But the addition of AA2P to growth medium increased the number of cells undergoing division. In particular, AA2P caused a significant, 2-fold increase in the number of cells undergoing DNA synthesis (P<0.001). We can thus conclude that the presence of AA2P in the medium is not enough to modulate fibroblast cell cycle progression, but it stimulates the cell cycle re-entry of quiescent fibroblasts in the presence of serum. Cell motility 13 During the early stages of the physiological response to a wound, not only are fibroblasts required to proliferate, they’re also the first cell type to migrate and invade the wound. Cell motility/migration is a process that involves the coordinated expression of several motility factors and extracellular matrix proteases. In this study, AA2P increased the expression of the urokinase-type plasminogen activator, a protease that plays an important role in cellular migration and is vital during the initial phases of wound healing [21] (Table 2). Likewise, AA2P up-regulated the hyaluronan-mediated motility receptor, which is required for fibroblast migration in the context of wound healing [22], and interleukin 6, which also promotes cell motility and matrix remodelling during wound healing [23]. We could thus hypothesise that vitamin C may have yet another role in fibroblast activation during wound healing by enhancing cell migration. We investigated the effect of AA2P on cellular migration using a standard in vitro wound healing assay [24]. Post-confluent fibroblasts were incubated in the presence or absence of 100 µM AA2P for 3 days, when an artificial wound was created by gently scratching the cell monolayer. Cells were returned to growth medium with or without AA2P and wound closure was assessed 24 hr later. As expected, fibroblasts migrated as a loosely connected cell population. However, wound invasion occurred at substantially different rates in control (scorbutic) and AA2P-treated cells (Figure 3). Whilst control cells migrated slowly towards the wound area, treated cells show full invasion of the wound within 24 hr post insult. Results clearly show that AA2P (100 μM) increased the number of cells that migrated into the wound area, which is indicative of enhanced healing. DNA repair 14 We have shown here that AA2P induces the expression of a cluster of genes that are essential for DNA replication during S phase of the cell cycle (Table 2). Some of these genes, however, also play important roles in DNA repair. For example, RAD51 is involved in DNA unwinding during replication but also in double-strand break repair via homologous recombination. Histone H2A.X is also required for double-strand break repair [25]. Other genes, up-regulated by AA2P, which are associated with base excision repair (BER) include FEN1, replication factor C and NEIL3. Tissue injury is often associated with oxidative damage and indeed most products of base oxidation are thought to be repaired by BER [26]. In addition, it has been suggested that vitamin C may promote DNA repair in vivo [27]. In this study, we investigated whether continuous exposure to AA2P could render skin fibroblasts more capable of processing base lesions resulting from DNA oxidation. We induced oxidative damage to DNA by exposing cells to the polar photosensitizer Ro19-8022 in the presence of light. This system is a generator of singlet oxygen, leading to the formation of oxidised purines, predominantly 8-oxoGua, in much higher yield than single-strand breaks or sites of base loss [28]. To monitor the formation and subsequent removal of oxidised bases from genomic DNA, we employed the alkaline comet assay in conjunction with the hOGG1 repair glycosylase. OGG1 removes oxidation products of guanine from DNA, mainly 8-oxoG and, to a much lower extent, ring opened guanine, i.e., formamidopyrimidine [29]. In the method, hOGG1 acts at the sites of oxidised bases, leaving apurinic/apyrimidinic sites that are converted into breaks in the assay. Smith et al. [14] have used the assay before and reported high specificity towards oxidative DNA damage. The DNA repair assay was implemented here with several modifications, compared with the protocol of Smith et al [14]. To ensure that we were only measuring the lesions of interest, rather than non-specific breakage, we established the 15 optimal reaction conditions by titration, varying concentration of enzyme and time of incubation. An incubation time of 45 min at 37 ºC was needed to ensure full enzyme digestion (data not shown). Preliminary experiments have also shown that hOGG1 cutting of samples treated with Ro19-8022 and light increased with increasing amounts of the enzyme until a plateau was reached at about 0.16 U of the enzyme (Figure 4A). No adventitious cutting was observed in untreated samples, which confirms assay specificity (Figure 4A). We have used the assay conditions above (digestion time and amount of enzyme) in subsequent experiments and obtained a linear dose-response on the enzyme digestion of samples exposed to visible light in the presence of the photosensitizer for increasing times (Figure 4B). A treatment with visible light in the presence of the photosensitizer for 30 min was enough to induce an amount of DNA damage that was within the dynamic range of the assay (Figure 4B). Minimal levels of damage were present in the samples where no hOGG1 treatment was employed, confirming that this treatment specifically generates oxidatively damaged DNA that is recognised by hOGG1 (Figure 4B). In the DNA repair experiments, we incubated post-confluent fibroblasts with growth medium in the presence or absence of 100 µM AA2P for 3 days before exposing them to visible light in the presence of the photosensitizer. It is worth noting that the treatment with Ro19-8022 plus light was not toxic to fibroblasts. Cells were exposed to Ro19-8022 plus light and cell viability was assessed 48 hr later by the propidium iodide uptake method, as indicated in Materials and Methods. Irrespective of AA2P pre-incubation, the viability of cells exposed to Ro19-8022 plus light was higher than 95 %. Following treatment with Ro19-8022 plus light, fibroblasts were incubated for up to 9 hr and the repair of 8-oxoGua was monitored at regular intervals. Whilst the amounts of damage detected in AA2P-treated and in scorbutic 16 cells immediately post exposure to Ro19-8022 plus light were identical, the repair kinetics was much faster in the former. In fact, most damage persisted in scorbutic cells at the end of the 9-hour period post-insult, whereas cells that were pre-incubated with AA2P had removed most of the damage within the same time period (Figure 4C). We can thus conclude that AA2P stimulates the repair of 8-oxoGua lesions in contact-inhibited dermal fibroblasts. Discussion This is the first report of the genome-wide effects of vitamin C on gene expression in primary dermal fibroblasts. Non-dividing populations of fibroblasts were employed here as they may represent a better model of dermal cells in vivo than actively growing cells. Moreover, instead of looking at the immediate effects of a single addition of vitamin C to cell medium, we focused on the effects of sustained exposure. The most striking effect of both vitamin C derivatives in the gene expression profiling experiments was the induction of a large set of genes that are involved in DNA replication, or in the control or execution of the progression through the G2/M phases of the mitotic cell cycle, thus stimulating cell proliferation. This confirms previous reports that both AA [16-17] and AA2P [15] promote post-confluent proliferation of primary fibroblasts. But our results suggest that vitamin C may have a broader range of actions that are relevant to the process of wound healing. We showed that AA2P increased the percentage of quiescent fibroblasts that were stimulated to synthesise DNA and proliferate after serum stimulation. In vivo, dermal fibroblasts are exposed to serum during the re-colonisation of a wound. Growth factors released at a wound site can act as mitogens or as chemotactic factors for dermal fibroblasts. In response, fibroblasts begin to proliferate and 17 eventually migrate into the wound clot. This response is not immediate though, the ratelimiting step in this phase of wound contraction being the time required for fibroblasts to emerge from quiescence [30]. In this respect, our results suggest that vitamin C may favour wound healing by stimulating re-entry of quiescent fibroblasts into the cell cycle and by promoting cell migration. Indeed, fibroblasts incubated in the presence of AA2P expressed higher levels of genes involved in cell motility and matrix remodelling during wound healing such as urokinase-type plasminogen activator, hyaluronan-mediated motility receptor and interleukin 6, and showed markedly faster wound invasion in vitro. Studies in humans and in guinea pigs have shown that vitamin C deficiency impairs wound healing and repletion of the vitamin corrects the problem [31-32]. Recently, studies in mice showed that vitamin C enhances the healing of wounds caused by gamma-irradiation, namely by increasing the degree of wound contraction and reducing mean wound healing time [33]. Our work suggests that vitamin C may have an important role in wound healing by stimulating the activation of quiescent fibroblasts and fibroblast wound invasion. Notably, we also report that AA2P-treated fibroblasts repair 8-oxoGua lesions faster than scorbutic cells. BER proteins are known to associate with DNA replication proteins in cycling cells, allowing recruitment of the former at DNA base lesions and strand breaks occurring at replication forks and thereby ensuring fidelity of genomic replication in proliferating cells [34]. Indeed, the long patch-BER subpathway utilises the DNA replication machinery, including proliferating cell nuclear antigen, replication factor C and FEN1. The latter plays a central role by cleaving a single-stranded DNA flap of 5-7 deoxynucleotides that are displaced during repair synthesis by nuclear replicative DNA polymerases Polδ/ε (reviewed in [26]). Here we show that these factors are co-expressed in cycling cells and 18 present evidence for preferential repair of oxidised bases in replicating cells. Although we cannot exclude the possibility that the intracellular ascorbate remaining during the postincubation period may somehow enhance the induction of DNA repair enzymes secondary to the exposure to photosensitizer+light, our data suggest that vitamin C, by stimulating cell cycle progression, may increase the cellular ability to perform BER. It is widely considered that hOGG1 is the principal repair protein responsible for the removal of 8-oxoGua [35]. However, in our experiments hOGG1 mRNA expression was not affected by either vitamin C derivative. Nevertheless, it is known that mammalian cells have back-up systems for repairing the lesion, involving another family of oxidative lesion-specific DNA glycosylases [36-37]. We show that AA2P and AA increased the expression of NEIL3, a recently discovered DNA glycosylase that belongs to the Fpg/Nei family of oxidised basespecific DNA glycosylases [38-39]. Although the glycosylase activity of NEIL3 has not been established yet [40], Morland et al. [39] showed that it could excise Fapy lesions. Whilst oxidised base-specific glycosylases such as hOGG1 and NTH1 excise base lesions only from duplex DNA, members of the NEIL family preferentially excise their substrates from single-stranded DNA or unpaired sequences in bubble DNA structures, which suggests that NEILs are preferentially involved in BER of oxidized bases during transcription or DNA replication [41]. The specific activation of NEIL1 is specifically activated during Sphase [42] and binds to the proliferating cell nuclear antigen [43], but no such information exists for NEIL3. However, NEIL3 co-localises with replication protein A in the cell nucleus [39]. We have not established whether NEIL3 is implicated in the enhancement of DNA repair kinetics by AA2P, but our expression results support the idea that the gene is preferentially up-regulated in cycling cells and may associate with the replication machinery to remove 19 oxidised lesions from single-stranded DNA. We propose that the importance of this, with regard to wound healing, might be in providing fibroblast, in proximity to the wound, greater protection from ‘collateral’ ROS-induced DNA damage, arising from the activity of inflammatory cells. It is worth noting that fibroblast proliferation can also be induced in vivo in response to cytokines and growth factors released from inflammatory cells, potentially leading to tissue fibrosis. We have previously proposed that vitamin C may enhance oxidative tissue injury in conditions associated with elevated production of ROS (e.g. during inflammation) [10], which could potentially result in higher production of inflammatory agents. Here we show that vitamin C stimulates fibroblast proliferation. Hence, it would be interesting to determine whether AA supplementation could aggravate tissue fibrosis in vivo. Our work shows that vitamin C can activate intracellular signalling cascades that regulate fibroblast proliferation and motility. Presumably, the same mechanism explains the increased DNA repair capacity, as discussed. A proliferative response is generally mediated by the binding of growth factors to specific transmembrane tyrosine kinase receptors. The identification of the particular signal transduction pathway(s) sensitive to vitamin C warrants further investigation. However, it is possible that the effects reported herein are related with its ability to stimulate collagen synthesis. Dermal fibroblasts express two unrelated transmembrane receptors, namely α1β1 integrin receptor [44] and discoidin domain receptor 2 (DDR2) [45], which can transduce signals in response to collagen. Whilst DDRs possess intrinsic tyrosine kinase activity, integrins activate cytoplasmic protein tyrosine kinases of the Src- and focal adhesion kinase (Fak)-family [46]. Both DDRs and integrin receptors thus respond to collagen binding by initiating intracellular signals that synergize with those of 20 growth factors in the activation of protein tyrosine kinases and result in the downstream modulation of cytoskeletal tension and cell migration, as well as cell proliferation [46-47]. Vitamin C is necessary for the intracellular hydroxylation of prolyl and lysyl residues during collagen biosynthesis and therefore AA2P, which increases collagen deposition in skin fibroblasts [15], may activate either DDRs or integrin receptors (or indeed both) and downstream intracellular signalling pathways that modulate fibroblast proliferation and migration. It is unlikely, however, that such signalling pathways could explain all the gene expression effects described in the present study, some of which may relate to baseline physiological roles of vitamin C in cells, rather than to its involvement in wound healing. As discussed, the main effect of vitamin C depletion is the inactivation of prolyl hydroxylase reactions, resulting in insufficiently hydroxylated collagen and subsequently scurvy. These reactions are catalysed by members of the family of Fe2+- and 2-oxoglutarate-dependent dioxygenases that are also responsible for the hydroxylation of prolyl residues in the α subunit of the hypoxia-inducible transcription factor-1 (HIF-1), which prompts HIF-1 for destruction by the proteasome [48]. Ascorbate, which we have previously shown to increase intracellular catalytic iron (i.e. Fe2+) [10], is required for optimal activity of these enzymes, presumably by keeping the iron centre in the reduced state. Accordingly, it was recently shown that human skin fibroblasts and other cell types cultured in vitamin C-deficient media have a basal level of HIF-1 protein that is abolished when the medium is supplemented with physiological concentrations of ascorbate [49]. In our experiments, cells were grown to post-confluence, which induces a mild hypoxia [50]. According to our microarray results, dermal fibroblasts do not express some of the most studied HIF-1 targets, such as nitric oxide synthase or 21 erythropoietin. However, for several other genes that were previously shown to be upregulated during hypoxia in a HIF-1-dependent manner, the expression levels were significantly lower in AA- or AA2P-treated cells when comparing with vitamin C-depleted cells: vascular endothelial growth factor, TFRC, endothelin 1, stanniocalcin 1, several genes involved in glucose and energy metabolism (GLUT1, hexokinase 2, aldolase A, phosphoglycerate kinase 1, enolase 2, pyruvate dehydrogenase kinase 1), and two of the key enzymes in collagen synthesis, prolyl 4-hydroxylase-α 1 and lysyl-hydroxylase [51,52]. Our results thus support the idea that ascorbate plays an important role in primary cells by limiting HIF-1 signalling and inhibiting the response to hypoxic stress [49]. In summary, whilst the activation of specific signalling pathways remains to be elucidated, our results present new evidence that vitamin C repletion in skin cells is required for efficient wound healing and replication-associated repair of potentially mutagenic products of DNA oxidation. 22 Acknowledgements We are grateful to Dr. E. Moiseeva (University of Leicester) for collecting the wound repair assay images. We acknowledge two anonymous reviewers for helpful suggestions, in particular regarding the involvement of HIF-1 signalling. This work was supported by funding from the Fundação para a Ciência e a Tecnologia, Portugal, and the European Social Fund, Third Framework Programme to T. L. D. Comet assay studies in the laboratory of GDDJ are supported by grants from Cancer Research UK (Ref C13560/A46) and the Hope Foundation. M.S.C. and G.D.D.J. are partners of ECNIS (Environmental Cancer Risk, Nutrition and Individual Susceptibility), a network of excellence operating within the European Union 6th Framework Program, Priority 5:"Food Quality and Safety" (Contract No 513943). 23 List of Abbreviations 8-oxoGua, 7,8-dihydro-8-oxo-guanine AA, ascorbic acid AA2P, ascorbic acid 2-phosphate BER, base excision repair CCNB1, cyclin B1 DDR, discoidin domain receptor FBS, foetal bovine serum FEN1, flap structure-specific endonuclease 1 GLUT1, glucose transporter 1 HIF-1, hypoxia-inducible transcription factor-1 hOGG1, human 8-oxoguanine DNA glycosylase 1 LDLR, low-density lipoprotein receptor NEIL3, nei endonuclease VIII-like 3 ROS, reactive oxygen species TFRC, transferrin receptor TOP2A, DNA topoisomerase 2 alpha 24 References 1. Martin P. Wound healing-aiming for perfect skin regeneration. Science 276:75-81; 1997. 2. Wong, T.; McGrath, J. A.; Navsaria, H. The role of fibroblasts in tissue engineering and regeneration. Br J Dermatol 156:1149-1155; 2007. 3. Trautinger, F. Mechanisms of photodamage of the skin and its functional consequences for skin ageing. Clin Exp Dermatol 26 573-577; 2001. 4. Kvam, E.; Tyrrell, R. M. Induction of oxidative DNA base damage in human skin cells by UV and near visible radiation. Carcinogenesis 18:2379-2384; 1997. 5. Cooke, M. S.; Evans, M. D. Dizdaroglu, M.; Lunec, J. Oxidative DNA damage: mechanisms, mutation, and disease. FASEB J 17:1195-214; 2003. 6. Blanck, T. J.; Peterkofsky, B. The stimulation of collagen secretion by ascorbate as a result of increased proline hydroxylation in chick embryo fibroblasts. Arch Biochem Biophys 171:259-267; 1975. 7. Ponec, M.; Weerheim, A.; Kempenaar, J.; Mulder, A.; Gooris, G. S.; Bouwstra, J.; Mommaas, A. M. The formation of competent barrier lipids in reconstructed human epidermis requires the presence of vitamin C. J Invest Dermatol 109:348-355; 1997. 8. Duarte, T. L.; Lunec, J. When is an antioxidant not an antioxidant? A review of novel actions and reactions of vitamin C. Free Rad Res 39:671-686; 2005. 9. Marionnet, C.; Vioux-Chagnoleau, C.; Pierrard, C.; Sok, J.; Asselineau, D.; Bernerd, F. Morphogenesis of dermal-epidermal junction in a model of reconstructed skin: beneficial effects of vitamin C. Exp Dermatol 15:625-633; 2006. 25 10. Duarte, T. L.; Jones, G. D. D. Vitamin C modulation of H2O2-induced damage and iron homeostasis in human cells. Free Radic Biol Med 43:1165-1175; 2007. 11. Davis, P. K.; Ho, A.; Dowdy, S. F. Biological methods for cell-cycle synchronization of mammalian cells. Biotechniques 30:1322-1331; 2001. 12. Duarte, T. L.; Almeida, G. M.; Jones, G. D. D. Investigation of the role of extracellular H2O2 and transition metal ions in the genotoxic action of ascorbic acid in cell culture models. Toxicol Lett 170:57-65; 2007. 13. Li, C.; Wong, W. H. Model-based analysis of oligonucleotide arrays: expression index computation and outlier detection. Proc Natl Acad Sci U S A 98:31-36; 2001. 14. Smith, C. C.; O'Donovan, M.R.; Martin, E. A. hOGG1 recognizes oxidative damage using the comet assay with greater specificity than FPG or ENDOIII. Mutagenesis 21:185-190; 2006. 15. Hata, R.; Senoo, H. L-ascorbic acid 2-phosphate stimulates collagen accumulation, cell proliferation, and formation of a three-dimensional tissuelike substance by skin fibroblasts. J Cell Physiol 138:8-16; 1989. 16. Hata, R.; Sunada, H.; Arai, K.; Sato, T.; Ninomiya, Y.; Nagai, Y.; Senoo, H. Regulation of collagen metabolism and cell growth by epidermal growth factor and ascorbate in cultured human skin fibroblasts. Eur J Biochem 173:261-267; 1988. 17. Phillips, C. L.; Combs, S. B.; Pinnell, S. R. Effects of ascorbic acid on proliferation and collagen synthesis in relation to the donor age of human dermal fibroblasts. J Invest Dermatol 103:228-232; 1994. 26 18. Fernandez, C.; Lobo, M. D. V. T.; Gomez-Coronado, D.; Lasuncion, M. A. Cholesterol is essential for mitosis progression and its deficiency induces polyploid cell formation. Exp Cell Res 300:109-120; 2004. 19. Goldstein, J. L.; Brown, M. S. Atherosclerosis - Low-density lipoprotein receptor hypothesis. Metabolism-Clin Experim 26:1257-1275; 1977. 20. Danesh, F. R.; Ye, M.; Salmi, S.; LaPointe, M.; Batlle, D. Temporal profile of seruminduced S-phase entry and retinoblastoma protein phosphorylation in human skin fibroblasts. Kidney Int 56:1282-1285; 1999. 21. Choong, P. F.; Nadesapillai, A. P. Urokinase plasminogen activator system: a multifunctional role in tumor progression and metastasis. Clin Orthop Relat Res 415:S46-58; 2003. 22. Tolg, C.; Hamilton, S. R.; Nakrieko, K. A.; Kooshesh, F.; Walton, P.; McCarthy, J. B.; Bissell, M. J.; Turley, E. A. Rhamm-/- fibroblasts are defective in CD44-mediated ERK1,2 motogenic signaling, leading to defective skin wound repair. J Cell Biol 175:1017-1028; 2006. 23. Luckett, L. R.; Gallucci, R. M. Interleukin-6 (IL-6) modulates migration and matrix metalloproteinase function in dermal fibroblasts from IL-6KO mice. Br J Dermatol 156:11631171; 2007. 24. Liang, C. C.; Park, A. Y.; Guan, J. L. In vitro scratch assay: a convenient and inexpensive method for analysis of cell migration in vitro. Nat Protoc 2:329-333; 2007. 25. Ismail, I. H.; Hendzel, M. J. The gamma-H2A.X: is it just a surrogate marker of doublestrand breaks or much more? Environ Mol Mutagen 49:73-82; 2008. 26. Evans, M. D.; Dizdaroglu, M.; Cooke, M. S. Oxidative DNA damage and disease: induction, repair and significance. Mutat Res 567:1-61; 2004. 27 27. Cooke, M. S.; Evans, M. D.; Podmore, I. D.; Herbert, K. E.; Mistry, N.; Mistry, P.; Hickenbotham, P. T.; Hussieni, A.; Griffiths, H. R.; Lunec, J. Novel repair action of vitamin C upon in vivo oxidative DNA damage. FEBS Letters 439:363-367; 1998. 28. Will, O.; Gocke, E.; Eckert, I.; Schulz, I.; Pflum, M.; Mahler, H. C.; Epe, B. Oxidative DNA damage and mutations induced by a polar photosensitizer, Ro19-8022. Mutat Res 435: 89-101; 1999. 29. Krokan, H. E.; Standal, R.; Slupphaug, G. DNA glycosylases in the base excision repair of DNA. Biochem J 325:1-16; 1997. 30. McClain, S. A.; Simon, M.; Jones, E.; Nandi, A.; Gailit, J. O.; Tonnesen, M. G.; Newman, D.; Clark, R. A. F. Mesenchymal cell activation is the rate-limiting step of granulation tissue induction. Am J Pathol 149:1257-1270; 1996. 31. Hirschmann, J. V.; Raugi, G. J. Adult scurvy. J Am Acad Dermatol 41:895-906; 1999. 32. Peterkofsky, B. Ascorbate requirement for hydroxylation and secretion of procollagen relationship to inhibition of collagen synthesis in scurvy. Am J Clin Nutr 54:S1135-S1140; 1991. 33. Jagetia, G. C.; Rajanikant, G. K.; Rao, K. V. M. N. Ascorbic acid increases healing of excision wounds of mice whole body exposed to different doses of gamma-radiation. Burns 33:484-94; 2007. 34. Parlanti, E.; Locatelli, G.; Maga, G.; Dogliotti, E. Human base excision repair complex is physically associated to DNA replication and cell cycle regulatory proteins. Nucl Acids Res 35:1569-1577; 2007. 35. Klungland, A.; Bjelland, S. Oxidative damage to purines in DNA: role of mammalian Ogg1. DNA Repair 6:481-488; 2007. 28 36. Hazra, T. K.; Das, A.; Das, S.; Choudhury, S.; Kow, Y. W.; Roy, R. Oxidative DNA damage repair in mammalian cells: a new perspective. DNA Repair 6:470-480; 2007. 37. Minowa, O.; Arai, T.; Hirano, M.; Monden, Y.; Nakai, S.; Fukuda, M.; Itoh, M.; Takano, H.; Hippou, Y.; Aburatani, H.; Masumura, K.; Nohmi, T.; Nishimura, S.; Noda, T. Mmh/Ogg1 gene inactivation results in accumulation of 8-hydroxyguanine in mice. Proc Natl Acad Sci U S A 97:4156-4161; 2000. 38. Bandaru, V.; Sunkara, S.; Wallace, S. S.; Bond, J. P. A novel human DNA glycosylase that removes oxidative DNA damage and is homologous to Escherichia coli endonuclease VIII. DNA Repair 1:517-529; 2002. 39. Morland, I.; Rolseth, V.; Luna, L.; Rognes, T.; Bjoras, M.; Seeberg, E. Human DNA glycosylases of the bacterial Fpg/MutM superfamily: an alternative pathway for the repair of 8-oxoguanine and other oxidation products in DNA. Nucl Acids Res 30:4926-4936; 2002. 40. Hegde, M. L.; Hazra, T. K.; Mitra, S. Early steps in the DNA base excision/single-strand interruption repair pathway in mammalian cells. Cell Res 18:27-47; 2008. 41. Dou, H.; Mitra, S.; Hazra, T. Repair of oxidized bases in DNA bubble structures by human DNA glycosylases NEIL1 and NEIL2. J Biol Chem 278:49679-49684; 2003. 42. Hazra, T. K.; Izumi, T.; Boldogh, I.; Imhoff, B.; Kow, Y. W.; Jaruga. P.; Dizdaroglu, M.; Mitra, S. Identification and characterization of a human DNA glycosylase for repair of modified bases in oxidatively damaged DNA. Proc Natl Acad Sci U S A 99:3523-3528; 2002. 43. Dou, H.; Theriot, C. A.; Das, A.; Hegde, M. L.; Matsumoto, Y.; Boldogh, I.; Hazra, T. K.; Bhakat, K. K.; Mitra, S. Interaction of the human DNA glycosylase NEIL1 with proliferating cell nuclear antigen. The potential for replication-associated repair of oxidized bases in mammalian genomes. J Biol Chem 283:3130-40; 2008. 29 44. Pozzi, A.; Wary, K. K.; Giancotti, F. G.; Gardner, H. A. Integrin alpha1beta1 mediates a unique collagen-dependent proliferation pathway in vivo. J Cell Biol 142:587-594; 1998. 45. Olaso, E.; Labrador, J. P.; Wang, L. H.; Ikeda, K.; Eng, F. J.; Klein, R.; Lovett, D. H.; Lin, H. C.; Friedman, S. L. Discoidin domain receptor 2 regulates fibroblast proliferation and migration through the extracellular matrix in association with transcriptional activation of matrix metalloproteinase-2. J Biol Chem 277:3606-3613; 2002. 46. Schlaepfer, D. D.; Hunter, T. Integrin signalling and tyrosine phosphorylation: just the FAKs? Trends Cell Biol 8:151-157; 1998. 47. Vogel, W. F.; Abdulhussein, R.; Ford, C. E. Sensing extracellular matrix: an update on discoidin domain receptor function. Cell Signal 18:1108-1116; 2006. 48. Weidemann, A.; Johnson, R. S. Biology of HIF-1α. Cell Death Differ 15: 621–627; 2008. 49. Vissers, M. C. M.; Gunningham, S. P.; Morrison, M. J.; Dachs, G. U.; Currie, M. J. Modulation of hypoxia-inducible factor-1 alpha in cultured primary cells by intracellular ascorbate. Free Rad Biol Med 42: 765–772; 2007. 50. Karaczyn, A.; Ivanov, S.; Reynolds, M.; Zhitkovich, A.; Kasprzak, K. S.; Salnikow, K. Ascorbate depletion mediates up-regulation of hypoxia-associated proteins by cell density and nickel. J Cell Biochem 97:1025–1035; 2006. 51. Maxwell, P. H.; Pugh, C. W.; Ratcliffe, P. J. Activation of the HIF pathway in cancer. Curr Opin Genet Dev 11: 293–299; 2001. 52. Scheurer, S. B.; Rybak, J. N.; Rösli, C.; Neri, D.; Elia, G. Modulation of gene expression by hypoxia in human umbilical cord vein endothelial cells: A transcriptomic and proteomic study. Proteomics 4: 1737–1760; 2004. 30 Table 1. Real-time PCR conditions. Gene Name HPRT1 CCNB1 TOP2A LDLR FEN1 NEIL3 TFRC GLUT1 Annealing Temp. (°C) 57 55 55 57 57 57 57 57 MgCl2 (mM) Forward Primer Sequence (5’-3’) Reverse Primer Sequence (5’-3’) 2.5 2 2 3 2 2 3.5 2 GCAGACTTTGCTTTCCTTGGTCAG ATGATGTGGATGCAGAAGATGGA TCAAGCCCTCCTGCTACACATTTC GCAAGTGGCTTTCAACACACAACAG CCCATTATACCTCCTTCACCCCAGA GGAAGTCGGAAGAGCACTGGACCT TCTGACACGTCTGCCTACCCATTCG TGCAACGGCTTAGACTTCGACTCA GTCTGGCTTATATCCAACACTTCGTG TCTGACTGCTTGCTCTTCCTCAA TTTGCTGCTGTCTTCTTCACTGTCA GGGTTTGGCTTAGAGATTGGTGGATG TAGAATCCTCTCTCCACCCCGTGA TCAAGCAAGCATCACATGCCTTAGA TATGATGGTTCACTCACGGAGCTTCG TCTCTGGGTAACAGGGATCAAACAGA 31 Product Size (bp) 103 104 94 85 81 94 84 100 Table 2. Genes involved in cell proliferation, differentiation or migration with significant differential expression in response to 100 µM AA2P in contact-inhibited dermal fibroblasts*. Probe set ID† Gene ID‡ Gene name Fold Change P-value Regulation of cell cycle 204170_s_at 1164 203214_x_at 983 202870_s_at 991 201853_s_at 994 205167_s_at 995 204126_s_at 8318 204510_at 8317 221436_s_at 83461 224753_at 113130 224428_s_at 83879 221520_s_at 55143 203418_at 890 214710_s_at 891 202705_at 9133 204826_at 899 209714_s_at 1033 228033_at 144455 219990_at 79733 238756_at 283431 CDC28 protein kinase regulatory subunit 2 cell division cycle 2 cell division cycle 20 cell division cycle 25B cell division cycle 25C cell division cycle 45L cell division cycle 7 cell division cycle A3 cell division cycle A5 cell division cycle A7 cell division cycle A8 cyclin A2 cyclin B1 cyclin B2 cyclin F cyclin-dependent kinase inhibitor 3 E2F transcription factor 7 E2F transcription factor 8 growth arrest-specific 2 like 3 2.4 2.6 2.8 2.1 2.9 2.9 2.4 3.0 2.2 2.2 2.5 2.3 2.8 2.8 2.7 2.7 2.9 3.0 2.6 0.001 0.001 0.002 0.000 0.002 0.004 0.010 0.000 0.002 0.003 0.000 0.001 0.000 0.001 0.003 0.001 0.002 0.002 0.002 DNA replication and/or repair 228868_x_at 81620 204768_s_at 2237 218350_s_at 51053 205436_s_at 3014 202107_s_at 4171 222036_s_at 4173 216237_s_at 4174 219502_at 55247 204835_at 5422 205053_at 5557 205024_s_at 5888 204128_s_at 5983 203022_at 10535 209773_s_at 6241 202338_at 7083 1554696_s_at 7298 201292_at 7153 DNA replication factor flap structure-specific endonuclease 1 geminin, DNA replication inhibitor H2A histone family, member X MCM2 minichromosome maintenance deficient 2 MCM4 minichromosome maintenance deficient 4 MCM5 minichromosome maintenance deficient 5 nei endonuclease VIII-like 3 polymerase (DNA directed), alpha 1 primase, polypeptide 1, 49kDa RAD51 homolog (RecA homolog) replication factor C (activator 1) 3, 38kDa ribonuclease H2, subunit A ribonucleotide reductase M2 polypeptide thymidine kinase 1, soluble thymidylate synthetase topoisomerase (DNA) II alpha 170kDa 2.5 2.0 2.0 2.1 2.2 2.1 2.8 2.9 2.0 2.2 2.5 2.1 2.4 3.4 2.4 3.2 2.3 0.005 0.000 0.004 0.000 0.000 0.000 0.000 0.005 0.008 0.008 0.002 0.009 0.005 0.000 0.000 0.000 0.000 2.6 2.7 0.001 0.000 M phase of the mitotic cell cycle 219918_s_at 259266 asp (abnormal spindle)-like 208079_s_at 6790 aurora kinase A 32 209464_at 212949_at 215509_s_at aurora kinase B barren homolog 1 BUB1 budding uninhibited by benzimidazoles 1 homolog BUB1 budding uninhibited by benzimidazoles 1 homolog beta cell division cycle associated 1 centromere protein A centromere protein E, 312kDa centromere protein F, 350/400ka (mitosin) centromere protein K centromere protein M centromere protein N centrosomal protein 55kDa chromosome condensation protein G G-2 and S-phase expressed 1 kinesin family member 11 kinesin family member 14 kinesin family member 18A kinesin family member 20A kinesin family member 23 kinesin family member 2C kinesin family member 4A kinesin family member C1 kinetochore associated 1 kinetochore associated 2 MAD2 mitotic arrest deficient-like 1 M-phase phosphoprotein 1 NIMA (never in mitosis gene a)-related kinase 2 nucleolar and spindle associated protein 1 NudE nuclear distribution gene E homolog 1 PDZ binding kinase polo-like kinase 4 protein regulator of cytokinesis 1 spindle pole body component 24 homolog spindle pole body component 25 homolog TPX2, microtubule-associated, homolog TTK protein kinase 3.2 3.6 3.3 0.001 0.004 0.001 2.5 0.000 3.2 3.3 3.0 2.9 2.5 3.5 2.3 2.4 3.1 2.2 2.4 2.5 2.3 2.3 2.8 3.0 3.0 2.2 2.1 4.2 2.5 2.6 2.7 2.5 2.0 2.7 3.2 2.7 3.5 3.1 3.1 2.6 0.001 0.001 0.002 0.001 0.002 0.001 0.007 0.005 0.000 0.004 0.008 0.001 0.002 0.001 0.000 0.010 0.001 0.006 0.001 0.000 0.000 0.001 0.004 0.000 0.001 0.002 0.007 0.000 0.000 0.006 0.000 0.006 Lipid and steroid metabolism 200862_at 1718 208962_s_at 3992 201626_at 3638 202068_s_at 3949 200831_s_at 6319 24-dehydrocholesterol reductase fatty acid desaturase 1 insulin induced gene 1 low-density lipoprotein receptor stearoyl-CoA desaturase (delta-9-desaturase) 2.1 2.0 3.8 2.6 2.4 0.003 0.002 0.004 0.001 0.003 Glucose metabolism 238996_x_at 226 201313_at 2026 201250_s_at 6513 aldolase A, fructose-bisphosphate enolase 2 (gamma, neuronal) facilitated glucose transporter 1 -2.5 -3.2 -2.9 0.000 0.004 0.003 203755_at 223381_at 204962_s_at 205046_at 207828_s_at 222848_at 218741_at 219555_s_at 218542_at 218662_s_at 204318_s_at 204444_at 206364_at 221258_s_at 218755_at 204709_s_at 211519_s_at 218355_at 209680_s_at 206316_s_at 204162_at 1554768_a_at 205235_s_at 204641_at 218039_at 227249_at 219148_at 204886_at 218009_s_at 235572_at 209891_at 210052_s_at 204822_at 9212 23397 699 701 83540 1058 1062 1063 64105 79019 55839 55165 64151 51512 3832 9928 81930 10112 9493 11004 24137 3833 9735 10403 4085 9585 4751 51203 54820 55872 10733 9055 147841 57405 22974 7272 33 202934_at 200738_s_at 226452_at 200822_x_at 3099 5230 5163 7167 hexokinase 2 phosphoglycerate kinase 1 pyruvate dehydrogenase kinase, isozyme 1 triosephosphate isomerase 1 Negative regulation of transcription 202672_s_at 467 activating transcription factor 3 204998_s_at 22809 activating transcription factor 6 208937_s_at 3397 inhibitor of DNA binding 1 201565_s_at 3398 inhibitor of DNA binding 2 207826_s_at 3399 inhibitor of DNA binding 3 209292_at 3400 inhibitor of DNA binding 4 202364_at 4601 max interactor 1 Extracellular matrix/Cell adhesion or migration 229271_x_at 1301 collagen, type XI, alpha 1 207977_s_at 1805 dermatopontin 227265_at 10875 fibrinogen-like 2 209709_s_at 3161 hyaluronan-mediated motility receptor 205207_at 3569 interleukin 6 210150_s_at 3911 laminin, alpha 5 211668_s_at 5328 plasminogen activator, urokinase 202620_s_at 5352 procollagen-lysine, 2-oxoglutarate 5-dioxygenase 2 207543_s_at 5033 procollagen-proline, 2-oxoglutarate 4-dioxygenase, alpha 1 218638_s_at 10417 spondin 2, extracellular matrix protein 203083_at 7058 thrombospondin 2 203868_s_at 7412 vascular cell adhesion molecule 1 212171_x_at 7422 vascular endothelial growth factor Cytoskeleton 205132_at 222608_s_at 210334_x_at 203764_at 215116_s_at 222802_at 238621_at 201596_x_at 209016_s_at 203276_at 216952_s_at 237206_at 222077_s_at 222513_s_at 204288_s_at 219888_at 203145_at 217714_x_at 238688_at 70 54443 332 9787 1759 1906 342184 3875 3855 4001 84823 93649 29127 10580 8470 6676 10615 3925 7168 actin, alpha, cardiac muscle 1 anillin, actin binding protein baculoviral IAP repeat-containing 5 (survivin) discs, large homolog 7 dynamin 1 endothelin 1 formin 1 keratin 18 keratin 7 lamin B1 lamin B2 myocardin Rac GTPase activating protein 1 sorbin and SH3 domain containing 1 sorbin and SH3 domain containing 2 sperm associated antigen 4 sperm associated antigen 5 stathmin 1/oncoprotein 18 tropomyosin 1 (alpha) 34 -3.9 -2.0 -3.8 -2.0 0.000 0.000 0.000 0.000 2.0 -2.2 -16.8 -3.1 -3.9 -3.2 -2.2 0.003 0.010 0.005 0.001 0.001 0.001 0.001 2.5 2.2 -5.9 2.2 2.0 -2.3 2.2 -2.0 -3.1 0.000 0.000 0.003 0.001 0.005 0.004 0.004 0.002 0.000 2.9 2.2 2.3 -2.2 0.000 0.000 0.001 0.000 -4.3 2.4 2.5 2.7 2.1 -2.2 -3.4 -2.5 -2.2 2.9 2.3 -3.2 2.1 -2.6 -2.4 -3.0 2.5 2.2 -2.3 0.000 0.000 0.001 0.001 0.003 0.010 0.003 0.005 0.003 0.003 0.006 0.002 0.000 0.005 0.001 0.002 0.000 0.000 0.001 *See supplementary table 1 for full list of results. †Probe set ID according to Affymetrix. ‡Gene ID according to Entrez Gene. 35 Table 3. Effect of AA2P on cell cycle re-entry in serum starved fibroblasts Time post serum starvation Cell cycle distribution* G0/G1 S G2/M 0 hr 24 hr low-serum medium 24 hr low-serum medium + AA2P (100 µM) 24 hr growth medium 24 hr growth medium + AA2P (100 µM) 96.2 ± 0.2 95.8 ± 0.2 94.2 ± 0.2 87.5 ± 0.3 79.1 ± 0.8 3.3 ± 0.2 3.5 ± 0.1 4.8 ± 0.1 6.6 ± 0.1 8.2 ± 0.2 0.6 ± 0.0 0.8 ± 0.2 1.0 ± 0.1 6.0 ± 0.4 12.7 ± 0.7 *** *Results are the mean ± S.D. from 3 independent experiments. ***, P < 0.001 versus the proportion of cells in S phase in cells returned to growth medium for 24 hr. 36 Figure 1. Molecular structure of L-ascorbic acid 2-phosphate, magnesium salt. Figure 2. Validation of the expression of target genes by RT-PCR. Confluent GM5659 fibroblasts were incubated in complete growth medium alone or in the presence of 100 µM AA or AA2P added fresh every day for 5 days. T-RNA was extracted and the relative steadystate mRNA levels of cyclin B1 (CCNB1), DNA topoisomerase 2A (TOP2A), flap endonuclease 1 (FEN1), nei endonuclease VIII-like 3 (NEIL3), low-density lipoprotein receptor (LDLR), transferrin receptor (TFRC) and glucose transporter 1 (GLUT1) were measured by real-time RT-PCR as described in Materials and Methods. Results are the mean ± S.D. from 3 separate determinations. All results are P<0.005 versus control. Figure 3. Effect of AA2P on cellular migration towards the wound area. Fibroblasts plated on 12-well plates were grown to confluence and further incubated with growth medium alone (plates A-B) or in the presence of 100 µM AA2P (plates C-D) for 3 days. Post-confluent cells were wounded by gently scratching using a micropipette tip and incubated in fresh growth medium (plates A-B) or in medium containing AA2P (plates C-D) for 24 hr. The arrow mark represents the wound edge. Results are representative of 2 independent experiments, each containing 16 individual replicates. Figure 4. Effect of AA2P on the repair of oxidative DNA base lesions. A. Cells were either incubated with phosphate-buffered saline containing 0.4 µM Ro19-8022 and visible light for 30 min or sham-irradiated. Cells were harvested immediately and kept on ice. DNA damage was measured with the alkaline comet assay in conjunction with increasing amounts of hOGG1 37 enzyme, as described in Materials and Methods. Results are the mean ± S.E.M. of 100 cells pooled from duplicate slides. B. Cells were exposed to Ro19-8022 and visible light for 0, 15, 30 and 45 min. DNA damage was measured with the alkaline comet assay in conjunction with hOGG1 enzyme, as described in Materials and Methods. Enzyme was used at 0.16 U in 50 µL of enzyme buffer. Control samples received enzyme buffer only. Results are the mean ± S.E.M. of 100 cells pooled from duplicate slides. C. Confluent fibroblasts were incubated with growth medium in the presence or absence of 100 µM AA2P for 3 days before exposure to Ro19-8022 plus visible light, as described in Materials and Methods. Following treatment, cells were returned to growth medium and the repair of 8-oxoGua was monitored at 0, 3, 6 and 9 hr with the hOGG1 alkaline comet assay. Results are the mean ± S.D. from 3 independent experiments. 38