Poison Prevention
advertisement

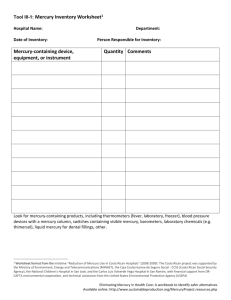
Wellness Tips… POISON PREVENTION Poison Prevention Each year in the U.S., thousands of people are accidentally poisoned. They often require emergency care. Poisoning can involve carbon monoxide fumes, cleaning products, medicines, vitamins and other household chemicals. Young children and senior citizens are often the victims. Handling and Storing Toxic Chemicals Most homes have cleaning products, lawn chemicals, insecticides, paint thinners, and medicines. When used for the right purpose, these products make our lives easier. But when they are used the wrong way or accidentally swallowed by a curious child, these chemicals can cause serious problems or death. Tips on poison prevention: Protect your family from carbon monoxide. Install a detector near bedrooms in your home. Have your furnace inspected every fall. Store chemicals and medicines in their original containers. These containers list information that can help in case of a poisoning. Using drinking glasses, cups or soda cans to store medicines and other chemicals can lead to poisonings. Read and follow label directions. Select products that are safe for your home and for nature. If you have questions about the use and disposal of a product, call the manufacturer at the number on the label. Buy only as much chemical as you need for the job. Although a larger amount may be cheaper, storing left over chemicals may be dangerous. Never mix products that contain chlorine bleach with products that contain acids or ammonia. Mixing these chemicals creates deadly chlorine gas. Tips to prevent childhood poisonings: Store dangerous chemicals in cabinets that are locked or too high to be reached by small children. Store vitamins, iron pills, and medicine in locked cabinets. Hide the key. Buy products in childproof containers. Learn about the plants in your home and yard. Some common poisonous plants are philodendrons, poinsettias and holly. Loan dangerous house plants to someone else or take them to work until your toddler is older. Living in a Home with Lead-Based Paint If your home was built before 1978, it may have lead paint or varnish. Dust or chips from lead paint can easily poison preschool-age children. Children under 3 years old are at highest risk. They can be lead poisoned if they play near windows or in bare soil with flaking paint. They can also be poisoned if they get dust on their fingers and toys and then put them in their mouths. Children who are exposed to lead can have life-long problems with learning, growth and behavior. An adult who is exposed to lead can have problems with blood pressure and trouble getting pregnant. Tips on Lead: Have preschool-age children tested for lead. Lead poisoned children don't look sick. The only way to know if they are lead poisoned is to have their blood tested. Your doctor, local health department, or clinic can test your child. From the Center for Disease Control (CDC) and Prevention © 2004 Magellan Health Services, Inc. Doc#0933—11/20/04 Wellness Tips… POISON PREVENTION Clean up as much chips and dust from lead paint with damp cloths as you can. Do not sweep. Clean up the remains using a vacuum with a HEPA filter. Many local health departments have HEPA vacuums you can borrow. Wash your hands thoroughly after cleaning up paint chips and dust. Control lead dust by damp dusting hard surfaces, wet mopping floors and vacuuming carpets often. Wash dust rags separate from other laundry or throw them away. Focus on windows and woodwork. Use paper towels, warm water and soap (any cleaner will work) to wash dust and pick up loose paint chips. Rinse well. Don't allow children to play or sleep in areas that have chips or dust from lead paint. Wash children's hands often. This is especially important before meals, snacks, naptime or bedtime. Feed your children foods that are high in calcium and iron. These minerals help to prevent lead absorption. Never disturb old paint when children are around. Keep children away while you refinish old painted surfaces. Never dry scrape, dry sand or burn old paint. Never use an open flame torch or a heat gun. Use a spray bottle with water to wet down the area where you will remove paint. Clean up paint chips right away. Call your local health department or for more information. Mercury in Your Home Many thermometers, electric switches, fluorescent light bulbs, and smoke detectors contain mercury. If these are broken or burned the mercury can enter the air of your home. Breathing air that contains mercury can cause nerve and kidney damage. Tips on mercury: Don't buy items that contain mercury. Buy digital or alcohol thermometers and thermostats. If a mercury thermometer breaks, use care to do the following: open windows to bring fresh air into the room, use two pieces of paper to carefully scoop the mercury into a plastic bag or container with a lid. Put another plastic bag over the first bag or container to prevent any vapor release. The bag can then be safely brought to an approved disposal area. Contact your local health department for information on disposal area locations. Never vacuum mercury droplets. This can cause dangerous levels of mercury vapors to be released into the air. If the mercury cannot be scooped up, contact your local public health department for a mercury spill clean up kit. The kit provides directions and a substance to make the mercury harmless. Contact your local health department immediately for help with mercury spills larger than a teaspoon. These spills need special cleanup attention. Disposing of Hazardous Household Waste Use "clean sweeps" programs in your area to get rid of household wastes like leftover paints, solvents, and pesticides. Take used motor oil and batteries to recycling centers. Resources Are Available Additional information, self-help tools and other resources are available online at www.MagellanHealth.com. Or call us for more information, help and support. Counselors are available 24 hours a day, seven days a week to provide confidential assistance at no cost to you. From the Center for Disease Control (CDC) and Prevention © 2004 Magellan Health Services, Inc. Doc#0933—11/20/04
![[Agency] recognizes the hazards of lead](http://s3.studylib.net/store/data/007301017_1-adfa0391c2b089b3fd379ee34c4ce940-300x300.png)