Objectives 46 - U
advertisement

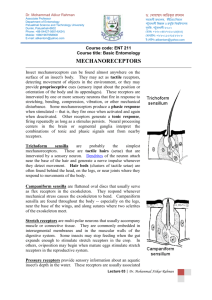
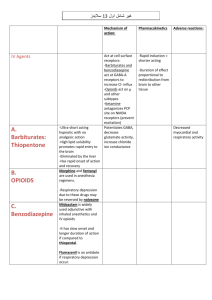
Physiology Objectives 46 1. Interaction of mechanoreceptors and ventilatory control: mechanoreceptors detect many different physiological alterations and feedback to the respiratory system to alter ventilatory input. Function of mechanoreceptor groups: a. Pulmonary receptors: a. Stretch receptors in extrapulmonary airways: slowly adapt to airway stretching and transbronchial pressure b. Irritant receptors in extrapulmonary airways: quickly adapt to cause hyperventilation, cough, and bronchoconstriction when stimulated c. Juxtacapillary receptors in the interstitium: quickly adapt to edema and inflammation to close the larynx and hyperventilate b. Chest wall proprioceptors: a. Joint receptors: respond proportionally to rib cage movement b. Tendon receptors: inhibit inspiration at intercostals and diaphragmatic muscle tendons c. Muscle spindle receptors: elevate ribs through intrafusal (gamma motor neuro) and extrafusal (alpha motor neuron) interplay c. Non-respiratory mechanoreceptors: a. Joint receptors: increase ventilation during exercise b. Thermal receptors: increase ventilation during hyperthermia c. Cardiovascular receptors: increase ventilation in shock 2. Alterations in diseased respiratory control: chronic increases in resistance, impairment of the ventilatory pumpdecreased efficiency of gas exchange,and reduced response to chemical stimuli can all affect respiratory control. 100% oxygen danger in chronic respiratory therapy: during chronic respiratory insufficiency, hypercapnea causes a metabolic alkalosis to balance the lowered pH. This bicarbonate formation, over time, lowers PCO2 and peripheral chemoreceptor sensitivity to the lowered CO2. It also crosses into the CSF and acts in the plasma to raise pH and render both central and peripheral H+ receptors ineffective. Thus, only peripheral oxygen chemoreceptors are active; administration of supplemental oxygen will stop hypoxic ventilatory drive and ultimately cause respiratory arrest. 3. Different breathing patterns and physiologic basis: a. Cheyne-Stokes breathing: oscillation of tidal volume due to instability in a control system (CNS dysfunction, cardiac failure with low cardiac output, sleep, hypoxia, profound hypocapnia) b. Apneustic breathing: deep inspiration with a pause before rapid, brief expiration due to dissociation of the pneumotaxic center (brainstem trauma, stroke, infection) c. Biot’s breathing: fixed tidal volume, frequency, and period, followed by apnea caused by CNS damage and loss of input (meningitis, encephalitis) d. Kussmaul respiration: deep, rapid inspiration with no end-expiratory pause due to profound acidosis (diabetic keto-acidosis, metabolic acidosis) 4. Integrated control of respiration during exercise: a. Phase 1: increase in ventilation before exercise onset due to cortical anticipation of exercise and joint proprioception of movement b. Phase 2: increase in ventilation at the onset of exercise due to increase in temperature, blood flow, and metabolite chemoreceptors c. Phase 3: plateau of ventilation during exercise that may be due to factors influencing phase 2 ventilation increases Note: after exercise there is a rapid drop in ventilation followed by a slow decline (perhaps in response to loss of cortical inputs followed by loss of metabolite chemoreceptor input)






![Respiratory System Lecture:9 [PPT]](http://s2.studylib.net/store/data/010095677_1-807d395ef4decfdd1b95f3c6166ad4e0-300x300.png)