Control of Ventilation
advertisement
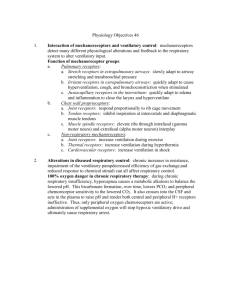
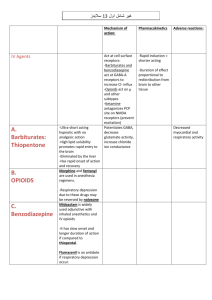
Lectures on respiratory physiology Control of Ventilation Respiratory control system Diagram showing the pons and medulla oblongata Rhythm controllers in the brainstem 1) Medulla Dorsal respiratory group – associated with inspiration Ventral respiratory group – associated with expiration. Pre-Botzinger Complex - pattern generator, also ventral 2) Pons Apneustic center – has an excitatory function Pneumotaxic center – can inhibit inspiration Other regions of the brain that can affect respiration 1) Cortex Can exercise voluntary control 2) Limbic system and hypothalamus Emotional states Effectors 1) Diaphragm 2) Intercostal muscles 3) Abdominal muscles 4) Accessory muscles Sensors 1) Central chemoreceptor 2) Peripheral chemoreceptors 3) Lung receptors 4) Other receptors Chemoreceptors Specialized tissues that responds to a change in the chemical composition of the blood or other fluid Central chemoreceptor Peripheral chemoreceptors Central chemoreceptor Central chemoreceptor Responds to pH of ECF CO2 diffuses across the bloodbrain barrier Normal CSF pH is 7.32 CSF has little buffering CSF bicarbonate controlled by choroid plexus Sites of peripheral chemoreceptors Carotid body receptor and its response Carotid bodies Respond to PO2, PCO2 and pH Little response in normoxia Very high blood flow Respond to arterial, not venous PO2 Fast response Lung receptors 1) Pulmonary stretch receptors (also called slowly-adapting pulmonary stretch receptors) Responsible for the Hering-Breuer reflex 2) Irritant receptors (also called rapidly-adapting pulmonary stretch receptors) 3) J receptors (juxta-capillary receptors) 4) Bronchial C fibers Other receptors 1) Nose and upper airway 2) Joint and muscle 3) Gamma system 4) Arterial baroreceptors 5) Pain and temperature Integrated responses 1) Response to increased PCO2 2) Response to reduced PO2 3) Response to changes in pH 4) Response to exercise Ventilatory response to CO2 Response to CO2 Primary factor in the control of ventilation Measured by rebreathing from a bag Inspiratory pressure following brief occlusion Response is altered by sleep, age, genetic factors Reduced by increasing the work of breathing Ventilatory response to PO2 Response to reduced PO2 No role under normoxic conditions Measured by rebreathing from a bag Increased response if the PCO2 is raised Important at high altitude Important in some patients with chronic lung disease Response to reduced pH Sensed by the peripheral chemoreceptors Important in metabolic acidosis If the reduction is severe, central chemoreceptors may be stimulated Response to exercise Blood gases are normal pH is normal except at heavy exercise ? Cortex, impulses from limbs, increased temperature, resetting of CO2 reference level Sleep apnea 1) Obstructive: very common; often associated with obesity; sleep deprivation may cause daytime somnolence and impaired cognitive function 2) Central: respiratory depression during sleep; recognized by the absence of respiratory efforts Periodic Breathing at High Altitude
![Respiratory System Lecture:9 [PPT]](http://s2.studylib.net/store/data/010095677_1-807d395ef4decfdd1b95f3c6166ad4e0-300x300.png)