CHAPTER 38 - Nursing Pharmacology FrontPage
advertisement
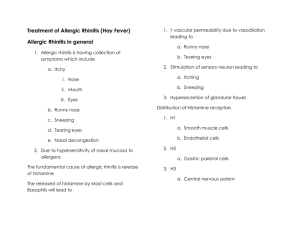
CHAPTER 38 DRUGS FOR ALLERGIC RHINITIS AND THE COMMON COLD LEARNING OUTCOME 1 Identify major functions of the upper respiratory tract. Concepts The upper respiratory tract warms, humidifies, and cleans incoming air. The upper respiratory tract traps particulate matter and many pathogens, preventing them from being carried to bronchioles and alveoli. The nasal mucosa is richly supplied with vascular tissue and is controlled by the autonomic nervous system. This first line of immunological defense incorporates ciliated epithelium, nasal mucus, and the mast cells that line the nasal mucosa to protect the body. The respiratory tract provides the body with the oxygen critical for all cells to carry on normal activities. The respiratory system also provides a means by which the body can rid itself of excess acids and bases. Figure 38-1 The Respiratory System LEARNING OUTCOME 2 Describe common causes and symptoms of allergic rhinitis. Concepts Allergic rhinitis or hay fever is inflammation of the nasal mucosa resulting from exposure to allergens. Allergic rhinitis is characterized by sneezing, watery eyes, and nasal congestion. It is caused by exposure to an antigen (allergen), which causes histamine release. The most common allegens include: pollens from weeds, grasses, and trees; mold spores; dust mites; certain foods; and animal dander. Chemical fumes, tobacco smoke, or air pollutants such as ozone are nonallergenic factors that may worsen symptoms. Pharmacotherapy is targeted at preventing the disorder or relieving its symptoms. (Figure 38.2 illustrates the mechanism of allergic rhinitis.) Figure 38.2 Mechanism of Allergic Rhinitis LEARNING OUTCOME 3 Differentiate between H1 and H2 histamine receptors. Concepts Histamine is a chemical mediator of the inflammatory response. H1 histamine receptors are found in the smooth muscle of the vascular system and bronchial tree and are responsible for many of the symptoms of allergic rhinitis. The other major histamine receptor, H2, is found in the gastric mucosa and is responsible for peptic ulcers. Adams Ch 38-1 LEARNING OUTCOME 4 Compare and contrast the oral and intranasal decongestants. Concepts 1. Intranasal glucocorticoids have become drugs of choice in treating allergic rhinitis due to their high efficacy and wide margin of safety. For maximum effectiveness, they must be administered 2 to 3 weeks prior to allergen exposure. Intranasal glucocorticoids decrease the secretion of inflammatory mediators, reduce tissue edema, and cause mild vasoconstriction. Alternative therapy is with mast cell stabilizers such as intranasal cromolyn (Nasalcrom). (See Table 38.3.) 2. The most commonly used decongestants are oral and intranasal sympathomimetics, which alleviate the nasal congestion associated with allergic rhinitis and the common cold. (See Table 38.4.) 3. Intranasal drugs are more efficacious but should only be used for 3 to 5 days due to rebound congestion. Intranasal preparations are available over the counter in sprays and drops. They affect a local action within minutes and have few systemic effects. 4. Oral preparation decongestants have more systemic effects, response time is slower, and they are less effective at relieving severe congestion. These drugs are often combined with antihistamine preparations. Table 38.3 Intranasal Glucocorticoids Table 38.4 Nasal Decongestants LEARNING OUTCOME 5 Discuss the pharmacotherapy of cough. Concepts 1. Cough is a natural reflex mechanism that serves to forcibly remove excess secretions and foreign material from the respiratory system. Common colds and allergies create cough. Antitussives are effective at relieving cough due to the common cold. Opioids are used for severe cough. Nonopioids such as dextromethorphan are used for mild or moderate cough. (See Table 38.5.) 2. Expectorants promote mucus secretion, making it thinner and easier to remove by coughing. Mucolytics directly break down mucous molecules. Table 38.5 Selected Antitussives and Expectorants Ch 38-2 Adams LEARNING OUTCOME 6 Describe the role of expectorants and mucolytics in treating bronchial congestion. Concepts 1. Expectorants are drugs that reduce the thickness or viscosity of bronchial secretions. They increase mucus flow that can then be removed more easily by coughing. The most effective OTC expectorant is guaifenesin (Mucinex, Robitussin, others). Guaifenesin has fewer adverse effects and is a common ingredient in many OTC multisymptom cold and flu preparations. It is most effective in treating dry, nonproductive cough, but may also be of benefit for patients with productive cough. 2. Mucolytics break down the chemical structure of mucus molecules. Mucolytics help loosen thick bronchial secretions. The mucus becomes thinner, and can be removed more easily by coughing. Acetylcysteine is delivered by the inhalation route and is used in patients who have cystic fibrosis, chronic bronchitis, or other diseases that produce large amounts of thick bronchial secretions. Mucomyst can trigger brochospasm and has an offensive odor resembling rotten eggs. A second mucolytic, dornase alfa (Pulmozyme), is approved for maintenance therapy in the management of thick bronchial secretions. Dornase alfa breaks down DNA molecules in the mucus, causing it to become less viscous. These agents are listed in Table 38.5. Table 38.5 Selected Antitussives and Expectorants LEARNING OUTCOME 7 For each of the classes listed in Drugs at a Glance, know representative drugs, and explain their mechanism of drug action, primary actions on the respiratory system, and important adverse effects. Concepts 1. H1 Receptor Antagonists (Antihistamines). Prototype drug: diphenhydramine (Benadryl). Mechanism of action: as a histamine (H1) receptor blocker (first generation). Primary use: to treat minor symptoms of allergy and the common cold, such as sneezing, runny nose, and tearing of the eyes. Adverse effects: drowsiness—occasionally, paradoxical CNS stimulation and excitability will be observed, rather than drowsiness. Anticholinergic effects such as dry mouth, tachycardia, and mild hypotension occur in some patients. Diphenhydramine may cause photosensitivity. (See Table 38.1.) 2. H1 Receptor Antagonists (Antihistamines). Prototype drug: fexofenadine (Allegra). Mechanism of action: as a histamine (H1) receptor blocker (second generation). Primary use: most effective when taken before symptoms develop. It reduces the severity of nasal congestion, sneezing, and tearing of the eyes. Adverse effects: drowsiness (less than first-generation H1 blockers), headache, and upset stomach. (See Table 38.2.) 3. Intranasal Glucocorticoids. Prototype drug: fluticasone (Flonase). Mechanism of action: decreases local inflammation in the nasal passages, thus reducing nasal stuffiness. Primary use: to treat seasonal allergic rhinitis. Adverse effects: nasal irritation and epistaxis. (See Table 38.3.) 4. Decongestants. Prototype drug: oxymetazoline (Afrin). Mechanism of action: stimulates alpha-adrenergic receptors in the sympathetic nervous system. This causes arterioles in the nasal passages to constrict, thus drying the mucous membranes. Primary use: to treat nasal congestion. Adverse effects: rebound congestion, which is common when oxymetazoline is used for longer than 3 to 5 days. Minor stinging and dryness in the nasal mucosa may be experienced. (Table 38.4.) Adams Ch 38-3 5. Antitussives. Prototype drug: dextromethorphan (Delsym, Robitussin). Mechanism of action: acts in the medulla to inhibit cough reflex. Primary use: as a component in most OTC severe cold and flu preparations. Adverse effects: dizziness, drowsiness, and GI upset. (See Table 38.5.) Table 38.1 H1 Receptor Antagonists Table 38.2 Selected Antihistamine Combinations Available OTC for Allergic Rhinitis Table 38.3 Intranasal Glucocorticoids Table 38.4 Nasal Decongestants Table 38.5 Selected Antitussives and Expectorants Table 38.6 Selected Opioid Combination Drugs for Severe Cold Symptoms Prototype Drug diphenhydramine (Benadryl) fexofenadine (Allegra) fluticasone (Flonase) oxymetazoline (Afrin) dextromethorphan (Benylin) ANIMATIONS AND VIDEOS Mechanism in Action: Diphenhydramine (Benadryl, others) LEARNING OUTCOME 8 Use the nursing process to care for patients who are receiving pharmacotherapy for allergic rhinitis and the common cold. Concepts 1. Patients Receiving Antihistamine Therapy—Assessment: Obtain a complete health history including previous history of symptoms and association to seasons, foods, or environmental exposures, existing cardiovascular, respiratory, hepatic, renal, or neurologic disease, glaucoma, prostatic hypertrophy or difficulty with urination, presence of fever or active infections, pregnancy or breast-feeding, alcohol use, or smoking. Obtain drug history noting type of adverse reaction or allergy, and possible drug interactions. Assess for any recent changes in diet, soaps including laundry detergent or softener, cosmetics, lotions, environment, or recent carpet-cleaning, particularly in infants and young children if allergy symptoms are of new onset. Obtain baseline ECG and vital signs, especially pulse rate and rhythm. Assess for adverse effects: dizziness, drowsiness, dry mouth, blurred vision, or headache. Evaluate appropriate laboratory findings (e.g., CBC, hepatic and renal labs). Assess respiratory status and breathing pattern. Assess neurologic status and level of consciousness. Report immediately any increasing fever, confusion, muscle weakness, tachycardia, palpitations, hypotension, syncope, dyspnea, pulmonary congestion, urinary retention, sudden severe eye pain or rainbow halos around lights. 2. Patients Receiving Antihistamine Therapy—Nursing diagnoses: Ineffective Airway Clearance; Ch 38-4 Adams Ineffective Breathing Pattern; Disturbed Sleep Pattern, related to adverse drug effects; Fatigue; Deficient Knowledge (drug therapy); Risk for Injury; Risk for Falls, related to adverse drug effects. 3. Patients Receiving Antihistamine Therapy—Planning: The patient will experience therapeutic effects (e.g., decreased nasal congestion and drainage, decreased eye watering and itching); be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects, and required precautions. Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider). 4. Patients Receiving Antihistamine Therapy—Implementation: Start therapy before beginning of allergy season and appearance of symptoms. Ensure patient safety, especially in the elderly. Monitor ambulation until effects of drug are known. Auscultate breath sounds before administering. Use with extreme caution in patients with asthma, COPD, and a history of cardiovascular disease. Keep resuscitative equipment accessible. Monitor vital signs especially pulse rate and rhythm (including ECG) for patients with existing cardiac disease before administering. Monitor for persistent dry cough, increasing cough severity, increasing congestion, or dyspnea. Monitor thyroid function. Use with caution in patients with a history of hyperthyroidism. Monitor for vision changes. Use with caution in patients with: narrow-angle glaucoma, history of kidney or urinary-tract disease, diabetes mellitus, history of seizure disorder; history of hyperthyroidism. Monitor neurologic status, especially LOC. Assess for urinary retention, especially in males over 40 or with a history of prostatic hypertrophy. Observe for signs of renal toxicity. Measure intake and output. Monitor periodic hepatic and renal function labs, especially in patients on long-term antihistamine use or those with previous history of hepatic or renal impairment. Monitor serum-glucose levels with increased frequency. Use with caution in patients with a history of GI disorders, especially peptic ulcers or liver disease. Monitor for GI side effects. Monitor for side effects, such as dry mouth; observe for signs of anticholinergic crisis. Instruct patient and/or family in proper self-administration of drug. 5. Patients Receiving Antihistamine Therapy—Evaluation: The patient will experience therapeutic effects (e.g., decreased nasal congestion and drainage, decreased eye watering and itching); be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects, and required precautions. Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider). 6. Patients Receiving Symptomatic Cold Relief: Antitussive, Nasal Decongestant, and Expectorant Therapy—Assessment: Obtain a complete health history, including previous history and length of symptoms, existing cardiovascular, respiratory, hepatic, or renal disease, presence of fever, pregnancy or breast-feeding, alcohol use, or smoking; data on anaphylaxis, asthma, or and allergies, drug history, and possible drug interactions. Evaluate appropriate laboratory findings (e.g., CBC, hepatic and renal labs). Obtain vital signs, especially pulse rate and rhythm in patients with existing cardiac disease. Assess for adverse effects: dizziness, drowsiness, blurred vision, headache, epistaxis. 7. Patients Receiving Symptomatic Cold Relief: Antitussive, Nasal Decongestant, and Expectorant Therapy—Nursing diagnoses: Ineffective Airway Clearance; Ineffective Breathing Pattern; Disturbed Sleep Pattern, related to somnolence or agitation; Deficient Knowledge (drug therapy); Risk for Injury, related to adverse drug effects; Risk for Injury, related to adverse drug effects; Risk for Falls, related to adverse drug effects. 8. Patients Receiving Symptomatic Cold Relief: Antitussive, Nasal Decongestant, and Expectorant Therapy—Planning: The patient will experience therapeutic effects (e.g., decreased nasal congestion and drainage, increased ease in expectorating mucus, thinner secretions, breath sounds clear). Be free from, or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects and required precautions. Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider). Adams Ch 38-5 9. Patients Receiving Symptomatic Cold Relief: Antitussive, Nasal Decongestant, and Expectorant Therapy—Implementation: Monitor for persistent dry cough, increasing cough severity, increasing congestion, or dyspnea. Assess color and consistency of any expectorated sputum. Monitor for GI effects. Use decongestant nasal spray first followed in 5 to 10 minutes by the glucocorticoid. Instruct patient and/or family in proper self-administration of drug. Auscultate breath sounds before administering. Use with extreme caution in patients with: asthma, COPD, and a history of cardiovascular disease. Keep resuscitative equipment accessible. Monitor vital signs especially pulse rate and rhythm. Monitor for vision changes. Use with caution in patients with: narrow-angle glaucoma, history of kidney or urinary-tract disease, diabetes mellitus, history of seizure disorder, history of hyperthyroidism. Monitor neurologic status, especially LOC. Observe for signs of renal toxicity. Measure intake and output. Monitor serum- glucose levels with increased frequency. Monitor for GI side effects. Use with caution in patients with a history of GI disorders, especially peptic ulcers or liver disease. Monitor for side effects, such as dry mouth; observe for signs of anticholinergic crisis. Report immediately any increasing fever, tachycardia, palpitations, syncope, dyspnea, pulmonary congestion, or confusion. 10. Patients Receiving Symptomatic Cold Relief: Antitussive, Nasal Decongestant, and Expectorant Therapy—Evaluation: The patient will experience decreased nasal congestion and drainage, increased ease in expectorating mucus, thinner secretions, clear breath sounds; be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects and required precautions. Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider). Ch 38-6 Adams