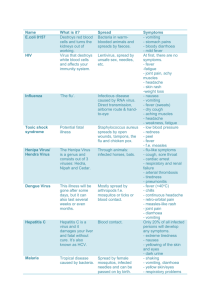
Foreign Animal Diseases of Concern
advertisement

Foreign Animal Diseases of Concern A. Jacques Fuselier, DVM, DABVP Large Animal Track 2012 ISVMA Conference Proceedings The United States is currently in a vulnerable position. Our beef and pork exports are increasing annually, as well as our food imports. A major reason for this is our safe food supply and being free of many diseases that are of concern to our global trade partners. The introduction of one of these foreign animal diseases to the United States would be economically damaging. Moreover, the Department of Homeland Security (DHS) is concerned about agroterrorism and bioterrorism. The purpose of this talk is to serve as a refresher on several foreign animal diseases of concern. Veterinarians are essentially our nation’s first line of defense and early recognition of these diseases is necessary to contain the disease and minimize the negative effects that will follow. Although all of the foreign animal diseases are important, for the purpose of this discussion, we will focus on the diseases of most concern for our livestock industry. African Swine Fever (ASF) African Swine Fever is a highly contagious viral disease of pigs. If it were to be introduced into the US, it could severely damage our pork exports valued at 2 billion dollars a year. This disease is essentially clinically indistinguishable from Classical Swine Fever and many of our domestic swine diseases. The most likely route of entry into the US will be through uncooked garbage or meat brought in by visitors from an endemic country. This disease could spread rapidly in this country because of our intensive swine industry and the extensive swine movements. African Swine Fever virus is the only member of the genus asfivirus of the family Asfarviridae. It has properties of a pox virus and is the only DNA virus transmitted by arthropods. Highly virulent strains cause peracute and acute disease with mortality reaching 100%. The low virulent strains are of most concern. These strains cause chronic disease with low mortality and infected pigs can transmit virus for up to 1 month. Recovered pigs may be life-long carriers. This virus remains stable at a pH range of 4-13 and can survive for 15 weeks in chilled pork products and 15 years in frozen carcasses. It also survives for at least 1 month in pig pens and 15 weeks in putrefied blood. Disinfectants found to be effective are Virkon 1% and bleach. Transmission Domestic and wild pigs, except African wild swine, are susceptible. Transmission is through oronasal contact (most common), feeding uncooked garbage with infected meat, Ornothodoros soft ticks, and fomites. The virus has been found to live in soft tick colonies for up to 8 years. Pathogenesis The primary route of infection is through the upper respiratory tract. The incubation period ranges from 5 to 15 days. Virus replication occurs in the tonsils and lymph nodes of the head and neck, followed by rapid, generalized infection. The reason for the hemorrhagic lesions is not well understood but suspected to be from viral disruption of the clotting mechanisms. Clinical Signs With peracute infections, pigs are just found dead. Acute disease results in nearly 100% mortality. Clinical signs before death usually include high fevers, bloody diarrhea, erythema, anorexia, and death. Animals that suffer the acute form of this disease never really lose body condition. The chronic form of this disease is the most concerning from a disease-spread standpoint. This presentation is associated with the low virulence strain and survivors may be life-long carriers. These animals present with overall low mortality, stunted growth, skin ulcers, and pneumonia. The chronically infected pigs will have an intermittent fever and lose body condition throughout the illness. The post-mortem signs commonly associated with all forms of ASF are enlarged dark red to black, friable spleen, as well as enlarged and hemorrhagic renal and gastrohepatic lymph nodes. Post-mortem signs commonly found with chronic, low virulence strains include pericarditis, consolidated lung lobes, necrotic dermal lesions, swollen joints, and generalized lymphadenopathy. If a case of ASF is suspected, the veterinarian should contact the Federal Area Veterinarian in Charge (AVIC) and the state veterinarian. Samples that will be submitted include serum, whole blood (heparin and EDTA), tonsil scraping, and fresh and fixed samples of spleen, tonsil, kidney, and distal ileum. There is no vaccine for this virus. Rapid detection, testing and slaughter is essential to control an outbreak. Heartwater Heartwater is a tick-borne disease of cattle, sheep, goats, and wild ruminants. It is caused by the Gram-negative rickettsia Ehrlichia ruminantium (previously Cowdria ruminantium). This disease is common on a few islands of the Caribbean and SubSharan Africa and is a definite threat to the Gulf Coast region of the US. Heartwater is characterized by neurologic signs, high fever, hydrothorax, hydropericardium, pulmonary edema, brain edema, and death. Transmission Although many ruminants are susceptible to this disease, variable susceptibility does exist. For example, zebu cattle have a low susceptibility and very young (less than a month old) animals are resistant. Transmission is via Amblyomma spp. Ticks. An important characteristic is that trans-stadial tick infection is common. Vertical transmission via colostrum is also likely. Cattle egrets are known to spread ticks around the Caribbean. It is possible for these migratory birds to bring infected ticks from the Caribbean to the US. We have competent tick vectors and wildlife hosts to support this disease. Importation of mammals, reptiles and valuable hides from Africa and the Caribbean adds to the risk of introducing infected ticks into the US. Pathogenesis The incubation period for this disease is 14-18 days. The rickettsia is injected into the ruminant during tick feeding. The initial bacterial replication occurs in macrophages and dendritic cells in regional lymph nodes. The bacteria enter the bloodstream and invade endothelial cells of many organs and tissues. Subsequent multiplication in the endothelial cells causes cell rupture and release of organisms, which results in increased vascular permeability. When this organism infects naïve animals, the mortality rate will range from 40-100%. Clinical Signs This disease presents in four different forms: the peracute (Boer goats & Jersey cattle), acute (most common), subacute, and subclinical forms. Animals with the peracute form are found recumbent and paddling, followed by sudden death. Sudden death is usually associated with severe pulmonary edema. Animals with the acute form are febrile, neurologic, in respiratory distress, and they die within one week. The neurologic signs include high stepping, ataxia, head pressing, and belligerence. Subacutely infected animals have pulmonary edema and fever for 10 or more days. These animals either slowly recover or die. Animals that have partial immunity, as well as newborns, will develop the subclinical disease, which consists of a transient fever. Diagnosis, Treatment, and Control Ticks should be submitted in alcohol for identification. PCR can be performed on whole blood (EDTA) and fresh lymph nodes, brain, and kidney. All samples should be submitted to NVSL in Ames, IA. Tetracyclines have been used to successfully treat heartwater since the 1950s and are still effective today. Tick control is essential to controlling this disease. It is important not to implement an intensive tick control program. This will lead to a naïve population of animals. It is good to have some exposure to maintain herd immunity. A suggested method is to only dip the animals if 10 or more ticks or evident on the animals. If this program is implemented, individual animals showing signs of disease should be treated with tetracycline. There is a live and an inactivated vaccine available, but no vaccines are approved for use in the US. Malignant Catarrhal Fever (MCF) Malignant Catarrhal Fever is caused by a gammaherpesviruses in the genus Macavirus. It is a sporadic, often fatal, multisystemic disease of cattle, deer, domestic swine, bison, and many exotic ruminants. This disease is often characterized by mucopurulent oculonasal discharge, corneal opacity originating at the limbus, keratoconjunctivitis, epithelial erosions, and enlargement of the peripheral lymph nodes. This virus is split into 2 main sub-groups: Ovine herpesvirus 2 (OvHV-2) and Alcelaphine herpesvirus 1 (AlHV-1). The OvHV-2 sub-group is commonly referred to as the sheep form and the AlHV-1 is known as the wildebeest form. OvHV-2 is endemic to the US. Caprine herpesvirus 2 (CpHV-2) and MCF of white-tailed deer (MCF of WTD) are other subgroups found to cause MCF. Transmission Sheep and wildebeest are carriers of the virus and do not show clinical signs. Close contact between carrier and susceptible animals is typically required, but transmission has occurred in animals several hundred yards away. Young offspring of the carrier animals are the most important in transmission to susceptible animals. The peak shedding of OvHV-2 occurs in nasal secretions of 6-9 month old lambs. The spread of disease has historically been associated with lambing season. Adults usually do not shed virus unless they are stressed. The AlHV-1 has been detected in nasal and ocular secretions of wildebeest calves up to 4 months old. Horizontal transmission between non-carrier animals is unlikely. Forced cohabitation studies have failed to induce horizontal transmission. As with most herpesviruses, latent infections with recrudescence could occur. Besides direct contact and aerosol transmission, MCF can be spread via ingestion of contaminated feed and water, as well as from arthropod vectors. Pathogenesis Following transmission, the virus infects the large granular T-lymphocytes resulting in severe immune dysfunction. The main dysfunction noted is decreased suppressor activity resulting in proliferation of T-lymphocytes and increased CD8+ cell activity. This leads to killing of normal cells. The incubation period for this disease can be as wide as 7-200 days following natural infection. Malignant Catarrhal Fever is known to have low morbidity (1% to 50% in naïve herds) and high mortality (80-100%). The tissues affected are mostly the epithelium of the upper respiratory tract, buccal papillae, and lymphatic structures. Clinical signs Corneal opacity – Starts at the limbus and migrates centrally Thick nasal exudate Necrotic muzzle Necrotic foci of nasal epitheium Tongue and buccal mucosal erosions Erosions of the palate Enlarged peripheral lymph nodes There are no approved vaccines for MCF in the US. If a case of MCF is suspected, the veterinarian should contact the Federal AVIC and the State Veterinarian. Foot and Mouth Disease (FMD) Foot and mouth disease is a popular topic and important viral disease of animals. As far as animal diseases, FMD is the most important constraint to international trade. Additionally, FMD was the first discovered viral disease of animals and currently serves as the disease that all other foreign animal diseases are measured against. Transmission: Foot and mouth disease is a highly contagious viral disease. Transmission occurs with either direct or indirect contact, via aerosols, fomites, contaminated feed, and direct penetrating trauma. Contaminated feed (swill feeding) is more common in swine transmission, whereas direct penetrating trauma is associated with swine to other animal transmission. Artificial insemination with infected semen can also transmit the virus. Natural hosts are even-toes ungulates (artiodactyls) including cattle, swine, sheep, goats, and more than 70 species of wild ungulates. During an outbreak, sheep serve as maintenance hosts, pigs act as amplifiers, and cattle act as indicators. Swine produce 30-100 times more virus in aerosols than sheep or cattle. Etiology: This highly contagious disease is caused by FMD virus (FMDV). FMD virus belongs to the family Picornaviridae and the genus Aphthovirus. It is a non-enveloped ssRNA virus with a positive sense genome. There are seven known FMDV serotypes (A, O, C, SAT1, SAT2, SAT3, and Asia1) and countless subtypes. All of the serotypes are antigenically distinct, so exposure to one type does not provide cross-protection against another type. This virus survives well in cold temperatures but is inactivated at prolonged exposure to temperatures above 122oF. It is quickly inactivated by pH less than 6.0 or above 9.0; therefore, it is destroyed in tissue after rigor mortis when pH drops below 6.0. Morbidity may reach 100% but mortality is as low as 1-5% in adults. Mortality in young animals is 20% or greater if they suffer from “tiger heart” or necrosis of the myocardium. Clinical Signs: Clinical signs usually appear in 3-5 days when susceptible animals are in contact with infected animals. Pigs that eat infected garbage usually start showing signs in 1-3 days. There is a persistent infection in ruminants. Cattle: Initially – pyrexia (103-105oF), shivering, and drop in milk production About 3 days into course of the disease – drooling, serous nasal discharge, kicking of the feet, lameness, and developing vesicles. Vesicles develop on tongue, dental pad, gums, palate, nostrils, muzzle, interdigital space, coronary band, and teats. Within 24 hours, vesicles rupture, leaving erosions in its place. Pregnant cows abort Calves may die Takes 2-3 weeks to recover. Sheep & goats: Pyrexia Lameness and oral lesions are mild. Lame animals have vesicles or erosions on interdigital space and coronary band. Agalactia in milking animals Abortion in pregnant animals Lambs or kids may die Vesicles or erosions on dental pad, lips, gums, or tongue Pigs: Pyrexia (104-105oF) Severe foot lesions and lameness Sloughing of claws Vesicles on pressure points of limbs, especially the carpus (knuckling) Vesicles on the snout and tongue Higher mortality than in cattle, sheep, or goats. Sows abort No drooling Diagnostics, Treatment, and Control: Immediately contact the Federal AVIC and State Veterinarian if any vesicular disease if discovered! Foot and Mouth suspect samples are immediately sent to the Foreign Animal Disease Diagnostic Laboratory (FADDL) on Plum Island, NY. Samples to be submitted include vesicular epithelium, heart, vesicular fluid if possible, whole blood, serum, nasal swabs, oral swabs, and sloughed epithelium or scabs. Sending digital photographs is also helpful. Extreme care must be taken when collecting samples because all secretions and excretions are potentially infectious; therefore, clean-up with appropriate disinfectants is required. If a FMD outbreak occurs, the following steps will be considered: Immediately slaughter infected and contact animals The decision to “ring” vaccinate or not Thoroughly disinfect vehicles and personnel Stop movement of all animals and animal products in the affected area Destroy carcasses Vaccinate? Inform and educate the public and trade partners. Vaccinating to control an outbreak is a controversial issue. Some trade partners will not allow “vaccinate to live”. Vaccinate to live means that the vaccinated animals will not be killed. The concern is that infected ruminants remain persistently infected, so there is concern that the older vaccine would lead to persistently infected cattle. Science doesn’t necessarily support this. More countries are in favor of “vaccinate to die” in the face of an outbreak. This means that vaccinated animals will be disposed of once the outbreak is under control. Areas that use the vaccinate to die method are considered free in 3 months, whereas the vaccinate to live areas are considered free in 6-12 months. The newest approved FMD vaccine developed on Plum Island is made from human adenovirus 5 vector containing FMDV genes. The anti-viral gene for IFNα type I can be added to provide protection within 3-5 days post vaccine. This vector is replication defective, so it can infect but not replicate in humans or animals. This new vaccine does not interfere with detection of natural exposure. It is a better DIVA vaccine than the previously produced vaccine. Since it is only using select FMDV genes, it can be manufactured on the US mainland. This vaccine still has the limitation of not preventing infection, but it does prevent the development of clinical signs and spread of the virus. References: Fernandez PJ, White WR. Atlas of Transboundary Animal Diseases. OIE (World Organisation for Animal Health), 2010 Committee of Foreign and Emerging Diseases of the United States Animal Health Association. Foreign Animal Diseases, seventh ed. 2008. p261-277