Maria Lobo`s Skin Notes
advertisement

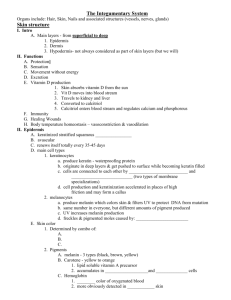
Maria Lobo The Skin 1. Explain the concept of the skin as a single organ of the body with its complex intra-relationships with other organ systems of the body. The skin is the largest organ of the body and essential for life. Diseases of other organs eg jaundice can affect the skin and skin can show the first signs of systemic disease. Functions of the skin include barrier function, peripheral outposts to the immune system, sexual attraction, temperature control. 2. Describe the basic anatomical structure of the skin and the intra-relationships between the epidermis, dermis and subcutis. There are three layers to the skin- epidermis (stratified squamous epithelium), dermis (structural and support), deep subcutaneous adipose tissue. Some cell types migrate through the different layers of the skin. 3. Describe the structure of the epidermis and associated adnexal structures, its foetal development and regulation of growth. The epidermis and adnexae originate from the ectoderm. Epidermis: 3rd week- single layer of glycogen-filled cells making up the epidermis 6th week- periderm (outer layer) and basal layer (inner layer) making up epidermis 21st week- periderm disappears, basal layer forms epidermal cells for rest of life. Hair follicles: 9th week- hair follicles appear in eyebrows, upper lip, chin. Appear as a cluster of cells in the basal layer of the epidermis, and then grow downwards into the dermis (hair pegs). Associated with fibroblasts and mesenchymal cells to form hair papilla. The tip of the hair peg becomes progressively bulbous and surrounds the dermal papilla. Lower bulge (arrector pili), middle bulge (sebaceous glands 16th week), upper bulge (apocrine glands and ducts). Glands numerous in whole body surface of foetus, most disappear in 3rd trimester. Stratum corneum- 15-20 layers keratinised cells. Anucleated and cannot divide. Change in type of keratin. Stratum granulosum- flat cells with dense keratohyalin granules containing fillagrin (promotes aggregation of keratin gilaments). Stratum spinosum- prickle cells with many tonofilaments (keratin intermediate filaments that attach to desmosomes). Stratum basale- 1-3cells thick. Small cells with large nuclei. Numerous desmosomes give strength. Function is to divide. Keratinocytes- labile cells that are produced in the stratum basale and move upwards. Cell division in the basal layer is controlled by stimulatory signals (EGF epidermal growth factors, TGFα transforming growth factor alpha, IL-1 interleukin 1, IL-6 interleukin 6, GM-CSF granulocyte macrophage colony stimulating factor) and inhibitory signals (TFG β transforming growth factor beta, IFN α and γ interferons alpha and gamma, TNF α tumour necrosis factor alpha). Cytokines and growth factors produced by keratinocytes, langerhans cells and lymphocytes. Adnexal structures include hair follicles, sebaceous glands and sweat glands and are in continuity with the epidermis. Sebaceous glands are lobulated. Small germinative basophilic cells at the periphery. Daughter cells migrate to centre, accumulate lipid droplets in cytoplasm, disintegrate and discharge cellular debris (sebum) into sebaceous duct. pH protects against bacterial infection. Sweat glands Maria Lobo Eccrine- whole skin, thermoregulation. Convoluted tube between dermis and subcutaneous fat secretes sweat, excreted by a straight duct crossing the dermis, acrosyringium in epidermis. Apocrine- scent glands, axillae, anogenital skin, around umbilicus. Secretory coil 10x bigger. Surrounded by myoepithelial cells. Apoecrine duct ends in the hair follicle above the sebaceous duct. Enlarge under hormonal influences. Apoeccrine glands- axillae, duct opens onto skin surface. 4. Outline the mechanisms by which the integrity of the dermo-epidermal junction is maintained and the results of failures of these mechanisms. Hemidesmosomes are the adhesion units between the basal layer of the epidermis and the dermis. Their main function is attachment but also control permeability across the dermis. Keratins 5 and 14 attach to the hemidesmosome. 6 key proteins span the dermo-epidermal junction (plectin, 230 kDa BP antigen, α6β4integrin, type 17 collagen, laminin 5, type 7 collagen) and bind to the lamina densa and anchoring fibrils in the dermis. 5. Describe the migrant cell populations within the epidermis and detail their origins. Langerhans cell- Antigen presenting cell with branched (dentritic) morphology. Specialised macrophage originating from bone marrow. Melanocyte- originate from neural crest synthesise melanin. Lower epidermis. Merkel cell- close to axonal processes involved in sensory perception. Basal layer of epidermis. 6. Describe the structure of the dermis including the vascular and nerve supply to the skin, the development of the dermis, regulation of collagen formation and events that occur in senescence. The dermis develops from the mesoderm. 2nd month- cellular. Fibrillar components and bands of collagen fibres →Distinct papillary and reticular layers. 4th month- Hair follicles develop, under surface of epidermis becomes irregular (rete ridge pattern). 5th month- connective tissue sheets around hair follicles. The dermis is a ground substance matrix in which polysaccharides and proteins interact to produce proteoglycans. Collagen (tensile strength) and elastin (elasticity) fibres. Superficial thin papillary dermis (interdigitates with epidermis) and underlying reticular dermis (blends with subcutaneous fat). Fibroblasts are the main cells (also mast cells, histiocytes, macrophages, leukocytes, melanocytes). Synthesise ground substance and collagen, possibly elastin. Collagen synthesis stimulated by PDGF platelet derived growth factor and TGFβ transforming growth factor beta (fibroblast proliferation stimulated by these and FGF fibroblast growth factor). After skin damage fibroblasts are activated and migrate onto fibronectin and fibrin, synthesise new collagen and induce healing tissue formation. Senescence (biological ageing) in skin is due to intrinsic ageing and environmental insults (UV radiation, menopausal hormonal changes). Dermis- ↓collagen, ↓elastic fibres, ↓number and size fibroblasts= wrinkles Maria Lobo Epidermis- rete ridge pattern of dermo-epidermal junction is flattened, epidermis thins, ↓water binding capacity of corneum, ↓sebaceous gland function= drier and flakier Pigmentation- melanocytes undergo localised proliferation at dermo-epidermal junction= liver spots Hair- bulbs lacking tyrosinase activity= grey, lack of melanocytes=white, ↓density of hair follicles ↓Sebum production, axillary apocrine glands regress. Blood vessels- coagulation, inflammation, angiogenesis Arteries enter the skin from the fascial network. The deep plexus gives braches to sweat glands and hair follicles. Diffusion from the superficial plexus keeps the epidermis alive. Skin perfusion is controlled by precapillary sphincters (by the deep and superficial vascular plexi), arteriovenous shunts (anastomoses mainly at the deep plexus so the blood can bypass skin) and vascular tone. Skin perfusion is controlled by the sympathetic nervous system and also by local factors. There are the greatest density of nerve fibres in the face and extremities. Most end in the dermis. Also ruffini nerve endings (sustained pressure), Krause end bulb (superficial dermis) and Golgi-Mazzoni (fingers). Nerves ascend to the thalamus via the spinothalamic or dorsal columns tracts. Efferent nerves from the sympathetic nervous system innervate vasculature, eccrine glands and the arrector pili muscles of the pilosebaceous unit. Afferent nerve endings Corpuscular (contain nonnervous endings) Encapsulated Meissner’s corpuscle superficial dermis, light touch Pacinian corpuscle deep touch (pressure vibration) myelinated axons Free Non-encapsulated Merkel cells sustained touch, pressure 7. Describe skin pigmentation, the development, function and control of melanocytes and the principals of immediate and delayed tanning. Melanocytes originate in the neural crest and migrate into the skin by week 8. Melanin production occurs by week 10. An epidermal melanin unit is made up of 1 melanocyte for 36 keratinocytes. There are two types of melanin both derived from tyrosine: eumelanin (brown/black insoluble) and phaeomelanin (yellow/redbrown soluble in alkalis, red heads). Melanin synthesis is regulated by melanocyte-stimulating hormone. It is packaged in granules called melanosomes. Melanin is needed to prevent damage to the DNA of keratinocytes. It decreases cutaneous carcinogenesis and prevents skin ageing. Immediate tanning- UVA radiation. Oxidation of pre-formed melanin. Delayed tanning- UVB radiating. Proliferation of melanocytes with increased tyrosinase activity and transfer of melanosomes. 8. Describe the development and maturation of acquired melanocytic naevi and the features of carcinogenic change within these lesions. Maria Lobo 9. Understand the structure and function of hair. Describe the development of the hair follicle, its anatomy and regulation of growth through life including the effect of sex hormones and age on hair growth. Understand the anatomy and growth of finger and toe nails. Function: Protect the skin (UV), thermoregulation, communication (sexual attraction, erect to convey threatening behaviour/fright, camouflage, sensation) Lanugo hair- 3rd trimester, shed by 8 months. Fine, soft, unpigmented unmedullated prenatal hair. Vellus hair- postnatal, shed by 4 months soft, some pigmented, unmedullated, <2cm, covers skin (except palms, soles, genitalia) Terminal hair- longer, pigmented, coarse, medullated, scalp, eyebrows, eyelashes (after puberty sex hormones convert vellus to terminal in beard, axilla, pubic regions). Hair is the keratinised product of the hair follicle. Intermediate filaments of alpha keratin made up of acid/base heterodimers in a double helix. Cuticle- Cells wrap round horizontally. 15 cells thick. Protection. Disulphide bridges. Cortex- Tightly bound bundles of keratin Medulla- Airspace Stem cells reside close to the insertion of the arrector pili muscle. Cells of hair bulb matrix divide often and give rise to hair shaft and inner root sheath. Melanocytes located in cells that become the cortex. Dermal papilla is fibroblast-like cells embedded in extracellular matrix with lots of proteins and proteoglycans. Hair cycle: Anagen- 2-6 years. Active hair growth. Catagen- 2-3 weeks. Proximal part of hair shaft keratinises to form a club-shaped structure. Lower part of follicle involutes by apoptosis. Base of follicle moves upwards. Telogen- 2-3 months. Club hair shed. At birth hair growth is synchronous, over time it becomes asynchronous. Influences: Testosterone- for most of life scalp is androgen insensitive and terminal follicle is maintained. However with balding terminal follicle becomes androgen sensitive and reverts to a vellus follicle. Prolactin, oestrogens and melanin also affect the hair cycle. Increased anagen duration is caused by pregnancy, hypertrichosis, trichostasis spinulosa. Decreased anagen duration is caused by androgenic alopecia, alopecia areata, telogen effluvium. Nails are made up of alpha keratin. Germinal matrix- half moon where the nail grows from. Thick epithelium of matrix cells. Eponychium- cuticle Nail plate- Multilayered lamellae of packed keratinised cornified cells. Hyponychium- under nails stops microorganism entry Maria Lobo 10. Describe the principles of barrier function of the skin and its role in controlling percutaneous water loss and absorption and defence against microbial invasion. The skin is a two way barrier to prevent inward and outward passage of water and electrolytes. The stratum corneum is selectively permeable and the dermis is durable and provides support. Liposomes rich in sphingolipids and lipids are arranged in Odland bodies inside keratinocytes. In the stratum granulosum the Odland bodies fuse with the cell membrane and discharge the contents where the discs of liposomes fuse to form intercellular lamellae, a good barrier for transepidermal water loss and preventing water being absorbed through the skin. The stratum corneum prevents invasion of the skin by normal skin flora or pathogenic microorganisms. Sebaceous lipids may have antibacterial properties (and the acidic pH). Glycophospholipids and fatty acids in the stratum corneum have bacteriostatic effects. 11. Explain the control of body temperature and the role of the cutaneous vasculature in maintaining body temperature. Thermoregulation is important because it enables human to live in a wide range of temperatures. The normal oral temperature is between 36.7°C and 37°C. It is 0.6°C higher when measured rectally. Peripheral temperature is lower than core temperature. Mental functions are impaired when outside the range of 35-40°C. There is diurnal variation in body temperature, it is also affected by age, external temperature, exercise and ovulation. Subcutaneous fat is a good insulator. Sources of heat: basal metabolic rate, muscle activity, effects of thyroxine, effects of sympathetic stimulation. Sources of heat loss: radiation (60%), evaporation (25%), conduction (12%), convection (3%) The main centre for detecting body temperature is the preoptic area in the anterior hypothalamus. There are also thermoreceptors in the skin and deep tissues (spinal cord, great veins, abdominal viscera). During infection the immune response to neutralise bacteria or viruses is to raise the set point, resulting in fever. Warming the body up: -sympathetic vasoconstriction of the dermal capillaries -piloerection (sympathetic stimulation of the arrector pili muscle) -shivering (increase in peripheral muscle tone) -chemical thermogenesis (cellular metabolism increased by adrenaline, noradrenaline or thyroxine) -behaviour (move, wear more clothes) Cooling the body down -sympathetic inhibition of vasoconstriction of the dermal capillaries -sweating (gland innervated by sympathetic nerve fibres) -decrease heat production (inhibition of shivering and chemical thermogenesis) -behaviour (move, wear less, cold drink) 12. Explain the importance of the skin as an immunological organ and describe the role of individual cell types in the cutaneous immune system. Innate immune system Skin as a barrier, sebum, sweat (lysozyme damages bacterial cell wall) Keratinocytes express toll-like receptors (recognise pathogen associated molecular patterns) that activate the production of chemokines and cytokines. Antimicrobial peptides kill bacteria, fungi, some viruses and activate immune cells. There are cathelicidin and defensin immune families. Small amounts produced in keratinocytes in follicular openings and sweat ducts and after injury or inflammation there is a rapid increase. (Reduction leads to atopic dermatitis) Keratinocytes produce proinflammatory and down regulatory cytokines. Mast cells are effector cells in allergic disease and are near hair follicles, sebaceous and sweat glands and near blood vessels. They have IgE receptors and release histamine. Monocytes circulate in the blood and migrate into tissue including the skin where they activate as macrophages. Phagocytic. Toll like receptors, pro-inflammatory cytokines, down-regulatory cytokines, growth factors. Maria Lobo Melanocytes produce melanin and prevent UV-induced immune suppression. Endothelial cells allow cells to adhere to and migrate through them when E-selectin is expressed Acquired immune system Keratinocytes can be induced to express MHC class II antigen by γ interferon, however they lack co-stimulatory molecules. They may induce tolerance in T cells. Langerhans cells make up only 2% of cells in the epidermis but cover 25% of the skin surface and are involved in immune surveillance. They are dendritic and contain Birbeck granules (trilaminate tennis racket granules involved in endocytosis). They process antigens and migrate to the paracortex of lymph nodes and present antigens to T cells activating them. (Contact dermatitis) T cells- in the steady state the main type is CD8+, in inflammatory skin conditions CD4+ helper T cells interact with Langerhans cells. In graft-versus-host disease donor T cells are stimulated to mount an immune response by host dendritic cells. 13. Explain the mechanism of skin wound healing. Healing after injury is regeneration (replacement with labile cells that can divide) or repair (formation of a fibrotic scar) Inflammatory phase Vasodilation of arterioles caused by histamine and prostaglandins. Increased permeability of post capillary venules caused by histamine and leukotrienes. Fluid containing water and ions moves into the interstitium causing the area to become red and swollen. Neutrophils and then macrophages move into the tissues attracted by chemotactic factors. Activation→rolling→adhesion→transmigration. The cells form the exudate which gets rid of dead cells, inflammatory debris, damaged collagen and stimulates regeneration of the epidermis and deposition of collagen in the dermis. Proliferative phase Macrophages produce growth factors that cause the formation of granulation tissue made up of proliferated capillaries, intercellular matrix (glucosaminoglycans) and type III collagen. Epidermis replaced by a scab. Dead epithelium produces epithelial growth factor that stimulates basal cells to proliferate. Maturation phase Type III collagen replaced by type I collagen. Increased deposition of collagen. Decrease in number of capillaries. Decrease in glucosaminoglycans in matrix. Harder, whiter scar Myofibroblasts appear containing actin filaments contract the scar so that it becomes narrower. A wound can be closed by primary intention (borders approximated, faster healing, smaller scar) or secondary intention (left to heal by itself, infection, concave, greater extent of healing processes). Complications of healing: Vitamin C deficiency→difficulty healing Diabetes→non-enzymatic glycosylation makes proteins less active and healing takes longer, greater risk of infection Keloids→fibrotic lesions after healing, excessive inflammatory process Dehiscence→tension at closure 14. Describe the consequence of skin organ failure and give examples of the impact of this on the body and other organ systems. Twenty Nail DystrophyIdeopathic. Early childhood. Ridging, striations, discolouration. Slowly return to normal. Hypohidrotic Ectodermal DysplasiaHypotrichosis (little hair), anodontia (lack of teeth), hypohidrosis (no sweat). X linked recessive or autosomal dominant. Recurrent high fever may lead to seizures. Maria Lobo AlbinismDisruption of melanocyte migration/ melanin synthesis/ melanosome formation/ transfer of melanosome to keratinocytes. VitiligoAutoimmune disease in which melanocytes are attacked Toxic Epidermal Necrolysis95% is drug induced, cell mediated cytotoxic reaction, fever cough sore throat malaise, then red macules of sheetlike epidermal detachment, mucosa affected first. Dehydration, protein and heat loss. Renal tubular necrosis. Bacterial sepsis. Epidermolysis Bullosa- genetic skin condition causing blistering, bullae break and leave areas of erosion.