Psychiatric Evaluation Form - Gencmh.org
advertisement
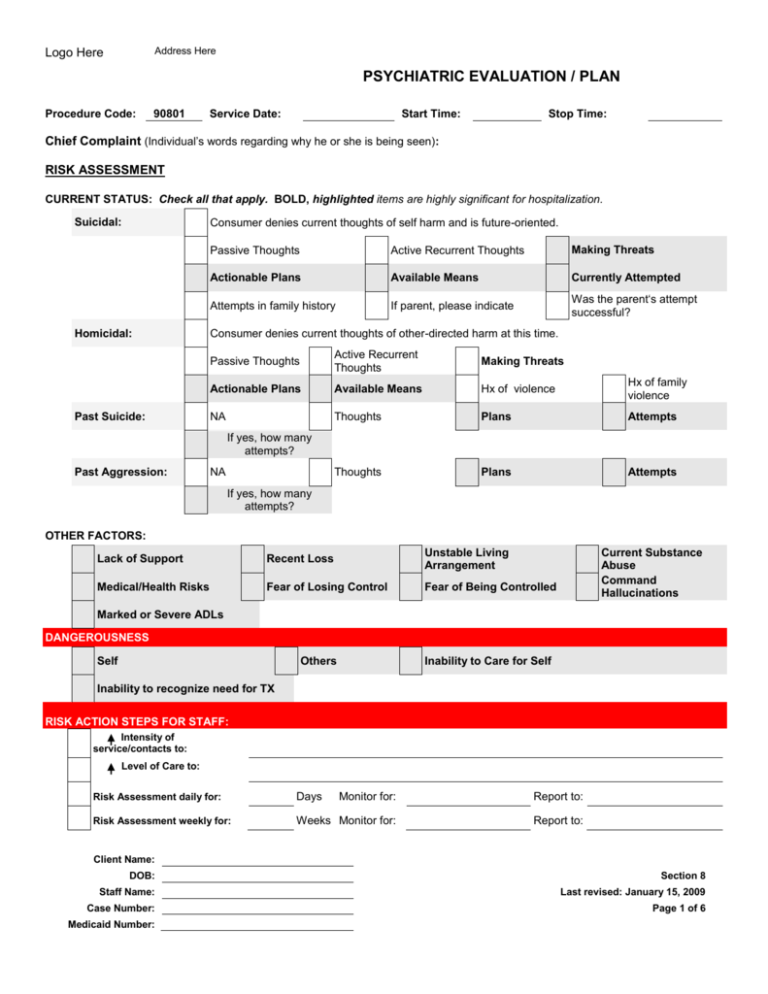
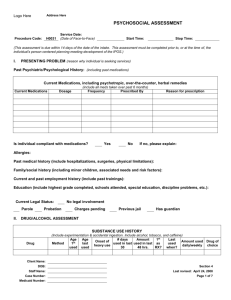
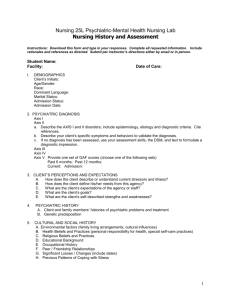
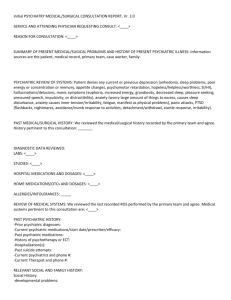
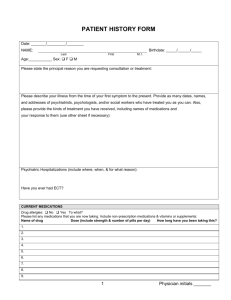
Address Here Logo Here PSYCHIATRIC EVALUATION / PLAN Procedure Code: 90801 Service Date: Start Time: Stop Time: Chief Complaint (Individual’s words regarding why he or she is being seen): RISK ASSESSMENT CURRENT STATUS: Check all that apply. BOLD, highlighted items are highly significant for hospitalization. Suicidal: Consumer denies current thoughts of self harm and is future-oriented. Homicidal: Past Suicide: Passive Thoughts Active Recurrent Thoughts Making Threats Actionable Plans Available Means Currently Attempted Attempts in family history If parent, please indicate Was the parent‘s attempt successful? Consumer denies current thoughts of other-directed harm at this time. Passive Thoughts Active Recurrent Thoughts Making Threats Actionable Plans Available Means Hx of violence Hx of family violence NA Thoughts Plans Attempts Thoughts Plans Attempts If yes, how many attempts? Past Aggression: NA If yes, how many attempts? OTHER FACTORS: Lack of Support Recent Loss Unstable Living Arrangement Medical/Health Risks Fear of Losing Control Fear of Being Controlled Current Substance Abuse Command Hallucinations Marked or Severe ADLs DANGEROUSNESS Self Others Inability to Care for Self Inability to recognize need for TX RISK ACTION STEPS FOR STAFF: Intensity of service/contacts to: Level of Care to: Risk Assessment daily for: Days Monitor for: Report to: Risk Assessment weekly for: Weeks Monitor for: Report to: Client Name: DOB: Section 8 Staff Name: Last revised: January 15, 2009 Case Number: Page 1 of 6 Medicaid Number: Logo Here Address Here PSYCHIATRIC EVALUATION / PLAN Risk Assessment monthly for: Months Monitor for: Report to: Other Action Step(s): History of Present Illness: Allergies: Current Medications (psychotropic, medical, herbal, over-the-counter): History of Adjustment to previous medications: PRN Medications (name and how administered): for the symptoms of Case referred to BMRC, date for initial BMRC review: Medical History: (check one) (sleep history (include sleep apnea), appetite, weight loss, past surgeries, past medications and response, hypertension, diabetes, seizures, liver disease) See valid data from current Psychosocial Assessment Date completed: Updated information: Psychiatric History: (check one) See valid data from current Psychosocial Assessment Date completed: Updated information: Family / Social / Sexual History: See valid data from current Psychosocial Assessment Date completed: Updated information: FORMAL MENTAL STATUS EXAM Attitude and Behavior: (attitude toward interviewer; contact with environment; dress; expressive movements; facial expression; motor activity) Stream of Mental Activity: (verbal productivity; spontaneity; distractibility; language deviations; reaction time) Emotional Reactions: (emotional display; predominant affect; persistence of mood; variability of affect; appropriateness of affect) Mental Trend: (persecutory ideas; suspiciousness; hypochondria; ideas of unreality; nihilism; depressive trends; grandiosity; hallucinations; illusions; delusions; phobias; obsessions; preoccupations; suicidal ideation; homicidal ideation) Sensorium, Mental Grasp and Capacity: (orientation; memory – recent, remote, immediate; retention and recall; calculation; school – general knowledge; intelligence) Insight and Judgment: (awareness of defects; personal judgment; impersonal judgment; plans for the future) Client Name: DOB: Section 8 Staff Name: Last revised: January 15, 2009 Case Number: Page 2 of 6 Medicaid Number: Logo Here Address Here PSYCHIATRIC EVALUATION / PLAN SUBSTANCE USE ASSESSMENT Current Substance Use Patterns: Prior Substance Use Treatment for Individual / Family: Drug Method Age 1st used Age last used Onset of heavy use Amt. used in past 48 hrs. # days used in last 30 1st as RX? Last used when? Amt. used daily/weekly Drug of choice? Comments: Any changes in patterns of use over time? Does individual ever drink or drug more than he/she intends? No Yes Has individual experienced an increase in the amount he/she can use to get the same effect? Is there a history of overdose? No Yes, describe: Is there a history of seizures? No Yes, describe: Is there a history of blackouts? No Yes, describe: Has individual ever used medications to either get high or come down from being high? No No Yes Yes With whom does individual usually use? Has individual had previous substance abuse treatment? No Yes, where: Diagnostic Impressions for this section: DSM – IV DIAGNOSIS (Codes must be specific up to the 5th digit if necessary. Indicate principal diagnosis with a ‘P’) Changes Code Code Axis I: Code Code Code Axis II: Code Code Axis III: Code Code Axis IV: Check all that are appropriate below and specify the problem: Client Name: DOB: Section 8 Staff Name: Last revised: January 15, 2009 Case Number: Page 3 of 6 Medicaid Number: Logo Here Address Here PSYCHIATRIC EVALUATION / PLAN Problems with primary support group (e.g. losses or disruptions in family or other natural supports, abuse, neglect, changes in family group) Specify: Problems related to the social environment (e.g. losses and disruptions in friendships, inadequate supports, lack of leisure opportunities, life cycle transition problems) Specify: Educational problems (e.g. inadequate environment, inadequate education, illiteracy, problems at school) Specify: Occupational problems (e.g. unemployment, threat of job loss, conflict/stress in workplace, lack of employment skills) Specify: Housing problems (e.g. homelessness, inadequate housing, unsafe neighborhood, conflict in neighborhood) Specify: Economic problems (e.g. poverty, lack of entitlements, lack of supports and resources; lack of clothing) Specify: Problems with access to health care services (e.g. little or no insurance, transportation problems, inadequate available services) Specify: Problems related to interaction with the legal system / crime (e.g. arrest, incarceration, litigation, victimization, probation/parole) Specify: Other psychosocial & environmental problems (e.g. disasters, conflict with service providers, lack of social service agencies) Specify: None Specify: Axis V: TREATMENT PLAN A. Target Symptoms/Behaviors/Concerns: (Include health/medical issues, e.g., hypertension, diabetes, etc; substance abuse; safety issues) B. Goals, Interventions and Objectives: (must address target behaviors/symptoms and include medications, recommended Client Name: DOB: Section 8 Staff Name: Last revised: January 15, 2009 Case Number: Page 4 of 6 Medicaid Number: Address Here Logo Here PSYCHIATRIC EVALUATION / PLAN evaluations, follow-up and communication with primary care physician, health and safety issues and substance abuse issues) Goal/Dream (state goal in collaboration with client): State desired result(s) in client’s words: Name of Covered Support or Service Needed (Scope) Amount/ Intensity (Units) Psychiatric Evaluation (Assessment & Evaluation) One visit By When (Duration) By Whom (Who will assist with this goal?) Objectives of this Service or Support with Target Dates: Interventions: Investigate clinical status, mental status, relevant history, personal strengths and assets. Establish plan of care for medication management. Notes: None Name of Covered Support or Service Needed (Scope) Medication Review Amount/ Intensity (Units) Visits q __ weeks/mths By When (Duration) By Whom (Who will assist with this goal?) Objectives of this Service or Support with Target Dates: Interventions: Evaluate and monitor effectiveness of medications Evaluate and monitor side effects Evaluate and monitor need for continued medication/change in medication Client Name: DOB: Section 8 Staff Name: Last revised: January 15, 2009 Case Number: Page 5 of 6 Medicaid Number: Address Here Logo Here PSYCHIATRIC EVALUATION / PLAN Notes: None SIGNATURES: Nurse Practitioner/Nurse Signature NP / RN Credentials Date Physician (Psychiatrist) Signature (if required) Credentials Date Client Name: DOB: Section 8 Staff Name: Last revised: January 15, 2009 Case Number: Page 6 of 6 Medicaid Number: