Psychosocial Evaluation Form
advertisement
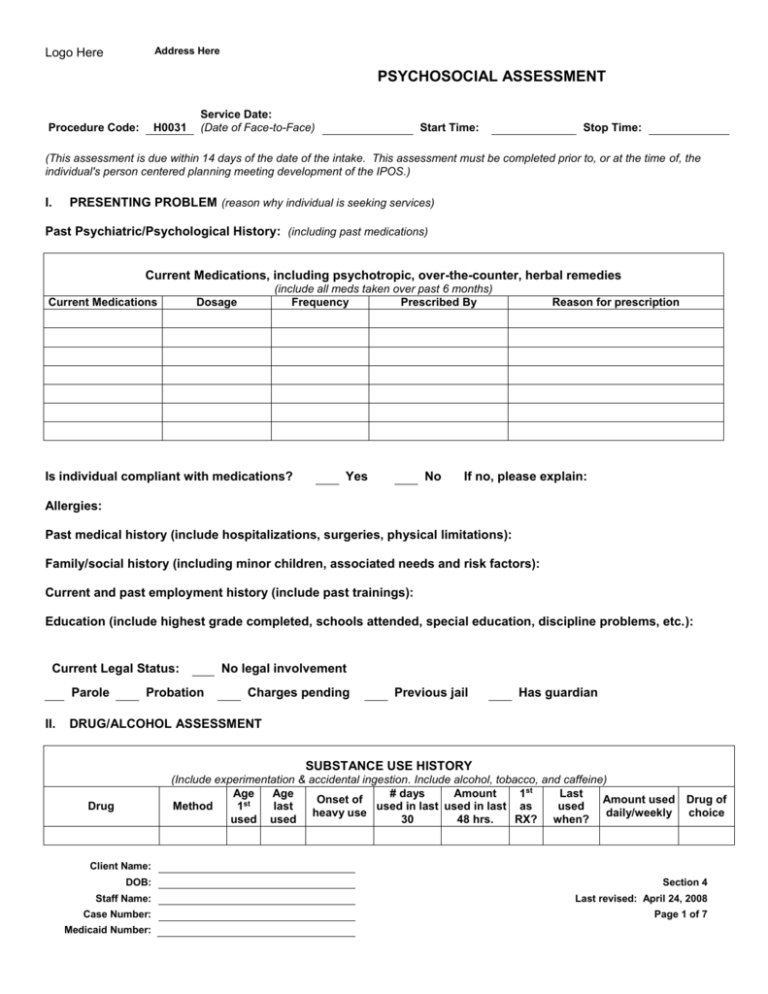
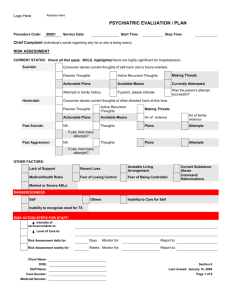
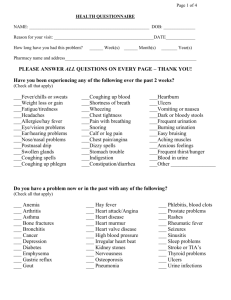
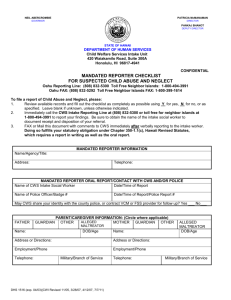
Address Here Logo Here PSYCHOSOCIAL ASSESSMENT Procedure Code: H0031 Service Date: (Date of Face-to-Face) Start Time: Stop Time: (This assessment is due within 14 days of the date of the intake. This assessment must be completed prior to, or at the time of, the individual's person centered planning meeting development of the IPOS.) I. PRESENTING PROBLEM (reason why individual is seeking services) Past Psychiatric/Psychological History: (including past medications) Current Medications, including psychotropic, over-the-counter, herbal remedies Current Medications (include all meds taken over past 6 months) Frequency Prescribed By Dosage Is individual compliant with medications? Yes No Reason for prescription If no, please explain: Allergies: Past medical history (include hospitalizations, surgeries, physical limitations): Family/social history (including minor children, associated needs and risk factors): Current and past employment history (include past trainings): Education (include highest grade completed, schools attended, special education, discipline problems, etc.): Current Legal Status: Parole II. Probation No legal involvement Charges pending Previous jail Has guardian DRUG/ALCOHOL ASSESSMENT SUBSTANCE USE HISTORY (Include experimentation & accidental ingestion. Include alcohol, tobacco, and caffeine) Age Age # days Amount 1st Last Onset of Amount used Method 1st last used in last used in last as used heavy use daily/weekly used used 30 48 hrs. RX? when? Drug Drug of choice Client Name: DOB: Section 4 Staff Name: Last revised: April 24, 2008 Case Number: Page 1 of 7 Medicaid Number: Address Here Logo Here PSYCHOSOCIAL ASSESSMENT SUBSTANCE USE HISTORY (Include experimentation & accidental ingestion. Include alcohol, tobacco, and caffeine) Age Age # days Amount 1st Last Onset of Amount used Method 1st last used in last used in last as used heavy use daily/weekly used used 30 48 hrs. RX? when? Drug Any changes in patterns of use over time? No Drug of choice Yes Does individual ever drink or drug more than he/she intends? No Yes Has individual experienced an increase in the amount he/she can use to get the same effect? Is there a history of overdose? No Yes, describe: Is there a history of seizures? No Yes, describe: Is there a history of blackouts? No Yes, describe: Has individual ever used medications to either get high or come down from being high? No No Yes Yes With whom does individual usually use? Has individual had previous substance abuse treatment? No Yes, where: Assessment of risk in this area: III. MENTAL STATUS ASSESSMENT (Describe any deviation from the norm under each category.) Appearance Mood Well groomed Disheveled Bizarre Other: Normal Depressed Anxious Euphoric Irritable Other: Describe: Describe: Attitude Speech Cooperative Uncooperative Suspicious Guarded Belligerent/Hostile Other: Describe: Normal Soft Loud Pressured Halting Incoherent Slurred Nonverbal Limited communication skills Uses yes/no only Uses a picture board Other: Describe: Client Name: DOB: Section 4 Staff Name: Last revised: April 24, 2008 Case Number: Page 2 of 7 Medicaid Number: Address Here Logo Here PSYCHOSOCIAL ASSESSMENT Motor Activity Thought Process Calm Hyperactive Agitated Other: Tremor/Tics Lethargic Describe: Intact Tangential Circumstantial Loose Associations Other: Flight of ideas Concrete thinking Inability to abstract Can only follow 1- step directions Describe: Affect Thought Content Appropriate Sad Flat Anxious Other: Inappropriate Angry Constricted Labile Describe: Normal Morbid Somatic Complaints Aggressive Other: Paranoid Phobias Obsessive Describe: Orientation: Psychosis: Person Place Time Responds to name Recognizes familiar faces or places Knows own daily schedule N/A Describe: Describe: Hallucinations: Denies Auditory Visual Other: Command Hallucinations: Denies Harm to self Harm to others Can resist commands Other: Describe: Describe: Bizarre Delusions: Denies Thought Broadcasting Thought Insertion Thought Withdrawal Other: Delusional Beliefs: Denies Religious Somatic Persecutory Grandiosity Being controlled Ideas of reference Describe: Describe: Summary/Assessment of Mental Status Exam: IV. HEALTH AND SAFETY (Assess as if person served were not in current placement.) Identified Risk Factors: None Client Name: DOB: Section 4 Staff Name: Last revised: April 24, 2008 Case Number: Page 3 of 7 Medicaid Number: Address Here Logo Here PSYCHOSOCIAL ASSESSMENT Unsafe Sex Practices Pregnancy Sexual Abuse Alcohol/Substance Abuse Self Harm Aggression Toward Others Verbal/Emotional Abuse Children at Risk Evacuation Score: Other: Physical Abuse Residential Safety IV Drug Abuse Diet/Nutrition Nicotine Use Medication Interaction Medication Management Stress Related to Parenting None Quarterly TD Screening - Due: Vision Exam Assistance With Children’s Needs Other: Impulsivity Chronic Health Problems Non-Attentive to Need for Health Care Hygiene Household Management Physical Disability Recent Loss (Parent, child, spouse, job, relationship) Psychosis Community Safety Identified Needs: Able to meet basic needs? Food Nutrition Assessment Labs - Frequency: Health Care Assessment/Yearly Checkup Dental Exam Coordination of Care N/A Medical Shelter Describe: DANGEROUSNESS A. Suicide Risk None Describe History of Suicidality: Ideation Chronic Acute Recent suicidal behavior Presence of Risk Behavior: Yes Yes Yes Yes No No No No Note Will Gives possessions away Other: Yes Yes Yes None No No No Describe: Presence of Risk Factors: Intent Means to carry out plan Access to gun None Prior attempts Lethality Plan Likelihood of rescue Describe: B. Threat of Danger to Others Thoughts of harm to others? Identified target Means to carry out plan Prior aggression None Yes Intent Lethality Plan No Recent threatening behavior? Yes No Can thoughts of harm be managed Access to gun Describe: Client Name: DOB: Section 4 Staff Name: Last revised: April 24, 2008 Case Number: Page 4 of 7 Medicaid Number: Address Here Logo Here PSYCHOSOCIAL ASSESSMENT C. Presence of Other High Risk Behaviors: Cutting Anorexia/Bulimia Other: None Head banging Risk taking Poor or dangerous relationship Other self-injurious behavior Describe: D. Presence of Deterrents: N/A Describe: E. Other Safety Concerns: None Describe: F. Assessment of Risk: V. FUNCTIONAL SUMMARY (Clinician’s view; check column as applicable) Not Applicable Function Strength Concern Function Daily Activities Safety Family relationships Legal Social Relationships Cognitive Functioning School Housing Work Social Skills Finances Impulse Control Physical Health Responsibility VI. VII. Not Applicable Strength Concern SUMMARY OF STRENGTHS, ABILITIES, NEEDS, & PREFERENCES (Clinician’s view with client’s input) OBSTACLES/BARRIERS TO SUCCESSFUL OUTCOMES VIII. DIAGNOSTIC INFORMATION (codes & nomenclature) *Designate “P” for primary diagnosis Code Client Name: DOB: Section 4 Staff Name: Last revised: April 24, 2008 Case Number: Page 5 of 7 Medicaid Number: Address Here Logo Here PSYCHOSOCIAL ASSESSMENT Code *Axis I Code Code Code Axis II Code Code Axis III Code Code Axis IV (Check all that are appropriate and specify the problem Problems with primary support group Specify: Problems related to the social environment Specify: Educational problems Specify: Occupational problems Specify: Housing problems Specify: Economic problems Specify: Problems with access to health care services Specify: Problems related to interaction with the legal system / crime Specify: Other psychosocial & environmental problems Specify: None Axis V OUTCOMES: GAF/GAS: CAFAS: Multnomah: IX. TREATMENT/SERVICES/SUPPORTS RECOMMENDATIONS FOR CLIENT/FAMILY (Add a bold letter from the list below to each checklist item (rather than a checkmark) to indicate activity required). Link Coordinate Provide Psychiatric Consultation Psychological Evaluation Speech/Language Occupational Therapy Physical Therapy Group Home/AFC Assistance with Benefits Physical Health Assessment Dept. of Human Services (formerly FIA) Train Monitor Instruct Community Support Medication Assistance Nursing Support Housekeeping Family Education Employment Assistance Money Management Dietary/Nutrition Assess Refer ADvocate Individual Therapy Group Therapy Family Therapy Dual Diagnosis Group Social Activity/Recreation Housing Assistance ADL Instruction Transportation Community Action Client Name: DOB: Section 4 Staff Name: Last revised: April 24, 2008 Case Number: Page 6 of 7 Medicaid Number: Address Here Logo Here PSYCHOSOCIAL ASSESSMENT Social Security Administration Home Health Room and Board Primary Health Care MRS/MI Jobs Commission CLF Substance Abuse Assessment Other (see Medicaid Chapter III / State Plan): Initial Completion: Clinician/Credentials Date: Supervisor/Credentials Date: Client Name: DOB: Section 4 Staff Name: Last revised: April 24, 2008 Case Number: Page 7 of 7 Medicaid Number: