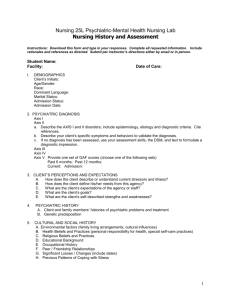
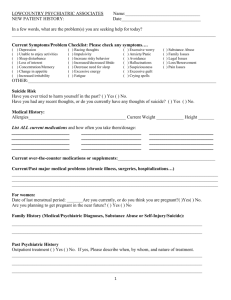
psych NEW PT template
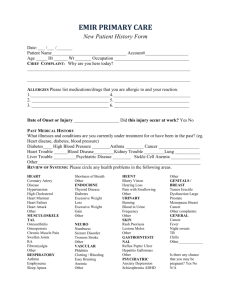
advertisement
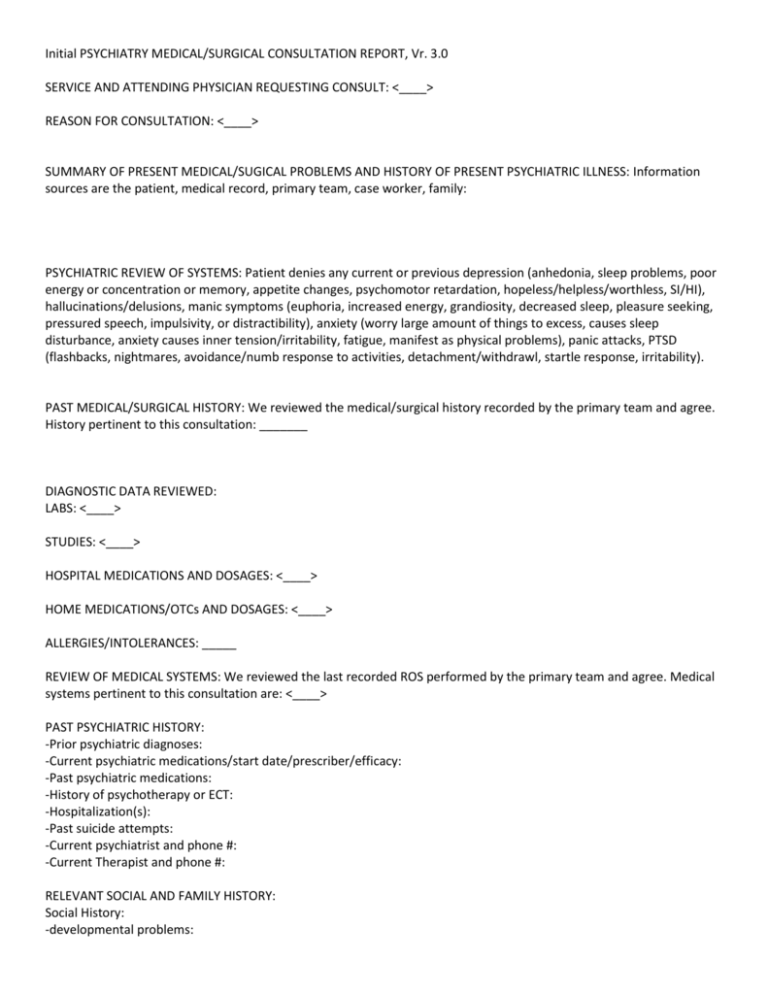
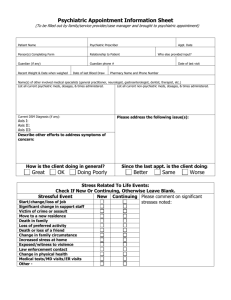
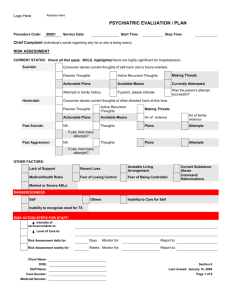
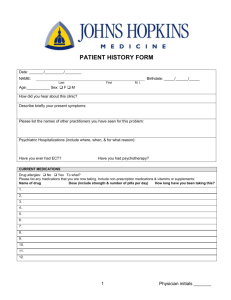
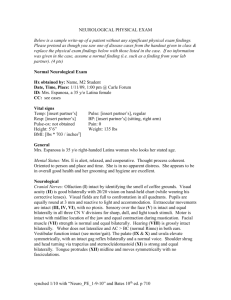
Initial PSYCHIATRY MEDICAL/SURGICAL CONSULTATION REPORT, Vr. 3.0 SERVICE AND ATTENDING PHYSICIAN REQUESTING CONSULT: <____> REASON FOR CONSULTATION: <____> SUMMARY OF PRESENT MEDICAL/SUGICAL PROBLEMS AND HISTORY OF PRESENT PSYCHIATRIC ILLNESS: Information sources are the patient, medical record, primary team, case worker, family: PSYCHIATRIC REVIEW OF SYSTEMS: Patient denies any current or previous depression (anhedonia, sleep problems, poor energy or concentration or memory, appetite changes, psychomotor retardation, hopeless/helpless/worthless, SI/HI), hallucinations/delusions, manic symptoms (euphoria, increased energy, grandiosity, decreased sleep, pleasure seeking, pressured speech, impulsivity, or distractibility), anxiety (worry large amount of things to excess, causes sleep disturbance, anxiety causes inner tension/irritability, fatigue, manifest as physical problems), panic attacks, PTSD (flashbacks, nightmares, avoidance/numb response to activities, detachment/withdrawl, startle response, irritability). PAST MEDICAL/SURGICAL HISTORY: We reviewed the medical/surgical history recorded by the primary team and agree. History pertinent to this consultation: _______ DIAGNOSTIC DATA REVIEWED: LABS: <____> STUDIES: <____> HOSPITAL MEDICATIONS AND DOSAGES: <____> HOME MEDICATIONS/OTCs AND DOSAGES: <____> ALLERGIES/INTOLERANCES: _____ REVIEW OF MEDICAL SYSTEMS: We reviewed the last recorded ROS performed by the primary team and agree. Medical systems pertinent to this consultation are: <____> PAST PSYCHIATRIC HISTORY: -Prior psychiatric diagnoses: -Current psychiatric medications/start date/prescriber/efficacy: -Past psychiatric medications: -History of psychotherapy or ECT: -Hospitalization(s): -Past suicide attempts: -Current psychiatrist and phone #: -Current Therapist and phone #: RELEVANT SOCIAL AND FAMILY HISTORY: Social History: -developmental problems: -abuse/trauma: -Highest level of educational level is ____. -Relationship status: ___ -Marital status/children: -Employment_____. -Living situation: Lives in _____, -Access to firearms ____. -Religion ___. Family History: No family history of psychiatric illness, suicide, dementia, or other relavent neurologic/medical conditions. SUBSTANCE USE HISTORY: -tobacco: -alcohol: -illicit drugs: Vital signs _____ MENTAL STATUS EXAMINATION: Appearance/Attitude: gender race age state of health dress, groom, hygiene Psychomotor Behavior: eye contact, mannerisms, involuntary movements, speed, aggitation, comfort Speech/Language: volume, rate, fluency, quanitity Affect: euthymic, depressed, dysphoric, elevated, euphoric Mood: "one word quote" Thought Process/Form of thought: word salad, flight of ideas, tangential, circumferential, goal directed, logical, coherant, echolalia, tight/loose associations, perseveration, blocking Thought Content/Perceptions: delusions, hallucinations, obsessions, prominent themes, SI, HI, death wish Sensorium/Level of awareness: level of alertness Attention/Concentration: days of week backward; ability to follow Memory/recent/remote: immediate, recent, remote, delayed recall Fund of knowledge: appropriate to level of education; current events, presidents backward Orientation: name, country, year, country, city, building, floor Executive Functions: <____> Insight/Judgment: good, fair, poor MENTAL STATUS EXAMINATION : Appearance/Attitude: Pleasant groomed Caucasian male lying in bed, good hygiene. Psychomotor Behavior: Good eye contact, appears comfortable. No abnormal movements, normal speed. Speech/Language: Fluent, appropriate quantity, volume, rate, latency. Affect: Euthymic. Mood: "" Thought Process/Form of thought: Goal-directed and logical. Thought Content/Perceptions: No delusions, hallucinations, or SI/HI. Sensorium/Level of awareness: Fully awake and alert Attention/Concentration: Fully intact and attentive. Can name days of week backwards. Memory/recent/remote: Intact for immediate, recent, and remote. 3/3 delayed recall. Fund of knowledge: Appropriate for educational level. Can name presidents backward to ____. Executive Functions: Intact. Insight/Judgment: fair/fair RATING SCALE USED AND SCORE: (MMSE, MOCA, etc) PHYSICAL AND NEUROLOGIC EXAMINATION: CN: PERRL, EOMI, facial strength and symmetry intact, tongue midline with full ROM and palate elevates symmetrically. No dysarthria. MOTOR: 5/5 strength bilaterally in UE and LE distally and proximally. SENSATION: Intact and equal sensation to light touch in UE and LE bilaterally. COORDINATION: FNF without slowing, dysmetria, or tremor. GAIT: Deferred. Reflexes: +2 bilaterally in biceps, triceps, brachioradialis, patella, and achilles. BIOPSYCHOSOCIAL FORMULATION: (ASSESSMENT) PSYCHIATRIC MULTIAXIAL ASSESSMENT: Axis I/clinical disorder: <____> Axis II/personality: <____> Axis III/medical/surgical: See reason for admission. Axis IV/psychosocial: contributors to current issues Axis V/functioning (0-100): INITIAL SUICIDE RISK ASSESSMENT: Factors that increase risk: Male, caucasian, age (15-24 or >45), depression, prior attempts, substance use, loss of rational thinking, lack of social support, no spouse, medical illness, hopeless, worthless, helpless, access to weapons, command AH, chronic pain, impulsivity. Factors that decrease risk: Denies SI, no h/o SI, no family hx, religious, family support, no substance abuse history, no gun in home. *Initial assessment and estimate of current risk: (low, moderate, high) <___> INITIAL CONSULTATION DAY RECOMMENDATIONS: * Recommendations relevant to suicide/homicide risk : <____> * Recommendations relevant to medications: <____> * Recommendations relevant to all other aspects of care: <___> We will continue to follow. Please contact this psychiatry resident or 2718 (if overnight) in the interim with questions or concerns. Seen and staffed with attending Dr. _____.