Urine Myoglobin Screen
advertisement
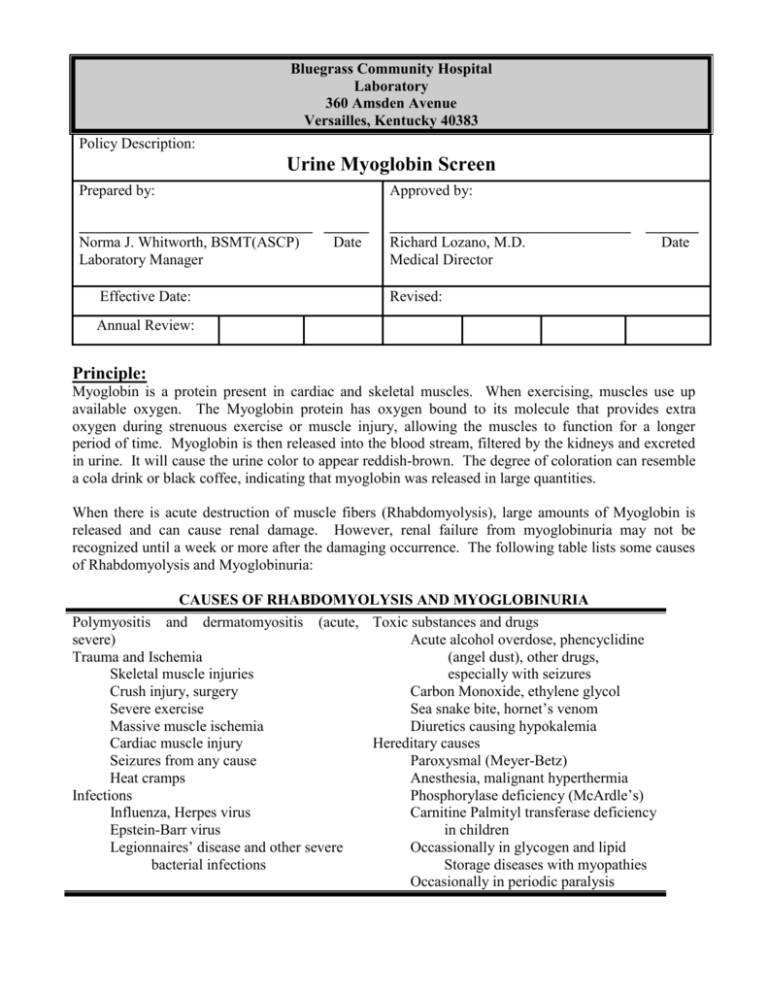
Bluegrass Community Hospital Laboratory 360 Amsden Avenue Versailles, Kentucky 40383 Policy Description: Urine Myoglobin Screen Prepared by: Approved by: _______________________________ ______ Norma J. Whitworth, BSMT(ASCP) Date Laboratory Manager ________________________________ Richard Lozano, M.D. Medical Director Effective Date: _______ Date Revised: Annual Review: Principle: Myoglobin is a protein present in cardiac and skeletal muscles. When exercising, muscles use up available oxygen. The Myoglobin protein has oxygen bound to its molecule that provides extra oxygen during strenuous exercise or muscle injury, allowing the muscles to function for a longer period of time. Myoglobin is then released into the blood stream, filtered by the kidneys and excreted in urine. It will cause the urine color to appear reddish-brown. The degree of coloration can resemble a cola drink or black coffee, indicating that myoglobin was released in large quantities. When there is acute destruction of muscle fibers (Rhabdomyolysis), large amounts of Myoglobin is released and can cause renal damage. However, renal failure from myoglobinuria may not be recognized until a week or more after the damaging occurrence. The following table lists some causes of Rhabdomyolysis and Myoglobinuria: CAUSES OF RHABDOMYOLYSIS AND MYOGLOBINURIA Polymyositis and dermatomyositis (acute, Toxic substances and drugs severe) Acute alcohol overdose, phencyclidine Trauma and Ischemia (angel dust), other drugs, Skeletal muscle injuries especially with seizures Crush injury, surgery Carbon Monoxide, ethylene glycol Severe exercise Sea snake bite, hornet’s venom Massive muscle ischemia Diuretics causing hypokalemia Cardiac muscle injury Hereditary causes Seizures from any cause Paroxysmal (Meyer-Betz) Heat cramps Anesthesia, malignant hyperthermia Infections Phosphorylase deficiency (McArdle’s) Influenza, Herpes virus Carnitine Palmityl transferase deficiency Epstein-Barr virus in children Legionnaires’ disease and other severe Occassionally in glycogen and lipid bacterial infections Storage diseases with myopathies Occasionally in periodic paralysis The distinction between hemoglobinuria and myoglobinuria can be difficult to make on urine color alone. Myoglobinuria should be considered if positive occult blood and protein tests on a reagent dipstick are seen. A quantitative measurement should then follow to determine whether the heme protein in the urine is hemoglobin or Myoglobin. The detection of protein is based on the “protein error of pH indicators.” The indicator 3, 3, 5, 5 tetrachlorophenol-3, 4, 5, 6-tetrabromosulfophthalein used in this test is a more recent development. A positive reaction is indicated by a color change from yellow to light green/green. The chemical detection of blood is based on the strong pseudoperoxidase action of erythrocytes and hemoglobin. The detection of blood in urine is based on the o-tolidine method by Leonards and further developed. Hemoglobin and Myoglobin, if present, catalyze the oxidation of the indicator by the organic peroxide contained in the test paper. Intact erythrocytes hemolyze on the test paper and liberate hemoglobin that produces a green dot. Separate sets of color blocks are representative of erythrocytes and hemoglobin. Scattered or compacted green dots on the yellow test paper are indicative of intact erythrocytes. Precautions: Universal precautions should be maintained during testing. Gloves, shield, fluid-resistant lab coat should be worn. Reagent dipsticks and controls are for in vitro diagnostic use only. Storage and Stability: Chemstrip 10 UA dipsticks should be stored at < 30 C (room temperature). Do NOT freeze. The vial must be closed when not in use. Rapid deterioration of dipsticks due to moisture and light can occur is vial uncapped for extended periods of time. Each vial is stable until expiration date printed on each vial label. Kova-trol I and III must be kept at 2 - 8 C and is stable until expiration date listed on each control bottle. Reconstituted controls must be kept refrigerated and are stable for 7 days. Aliquots of controls are stable up to 4 months when stored at –20 to –40 C. Do not shake roughly or expose to air or light for excessive amounts of time. Specimen Collection and Handling: A freshly voided clean catch urine specimen or first-morning collected in a clean, sterile screw-capped container may be used. At least, 20 ml of urine is required for screen and quantitative test if needed. Specimen should be brought to lab within one hour. If unable to transport immediately, refrigerate specimen at 2 – 8 C. Refer to the Specimen Collection SOP for details on collecting a urine specimen. Materials Needed: Plastic conical tube Clean, sterile screw-capped container Chemstrip 10 UA dipsticks/strips Chemstrip 101 reader Kova-Trol I Kova-Trol III Disposable paper towels Quality Control: Kova-Trol I and III are performed once per 24 hours usually on 3rd shift to verify reader and dipsticks results are within acceptable ranges. Results are recorded on each controls individual control logsheet. Procedure: Automated: 1) Label a plastic conical tube with patient’s last name and first initial. Place in specimen rack. 2) Mix urine specimen gently. Open lid and pour 10-12 ml of urine into conical tube. 3) Press “start” on Chemstrip 101 reader. 4) Open Chemstrip 10 UA vial and remove 1 dipstick. Immerse entire dipstick into urine specimen in conical tube. 5) Hold dipstick sideways against paper towel to allow excess urine specimen to drain. 6) Place dipstick into Chemstrip 101 reader pads facing upwards. 7) Press “start” to begin measurement. Results will print in approximately 60 seconds. Write patient’s name and medical record, date of birth, or social security number onto printout. 8) Record results of the blood (BLO) and protein (PRO) tests onto patient’s miscellaneous result form under “Urinalysis.” 9) Record results on Urinalysis Patient Log. Manual/Visual: 1a) Label a plastic conical tube with patient’s last name and first initial. Place in specimen rack. 2a) Mix urine specimen gently. Open lid and pour 10-12 ml of urine into conical tube. 3a) Open Chemstrip 10 UA vial and remove 1 dipstick. Immerse entire dipstick into urine specimen in conical tube. 4a) Hold dipstick sideways against paper towel to allow excess urine specimen to drain. 5a) Hold dipstick nest to the color blocks interpretation chart on side of Chemstrip 10 UA vial. 6a) Read Protein and Blood at 30 – 60 sec. Color changes are stable up to 120 sec after immersion in urine specimen. Do not read color changes that only occur along the edges of the test pads. 7a) Record results of the blood (BLO) and protein (PRO) tests onto patient’s miscellaneous result form under “Urinalysis.” 8a) Record results on Urinalysis Patient Log. Results and Interpretation: Positive for blood and protein, write in “Miscellaneous” area, “Myoglobin may be present, quantitative urine Myoglobin to follow.” Order Myoglobin quantitative test and send to referral lab for testing. Negative for blood and/or protein, result as “Myoglobin screen is negative, no further testing required.” Protein: A color change from yellow to light green/green will occur if protein is present. The concentrations given on the Chemstrip 10 UA vial label correspond with the albumin concentration in urine. Pathological proteinuria will usually produce persistent values above 30 mg/dl. Blood: Erythrocyte excretion up to 5 Ery/ul may be expected in normal urine. Levels above these should be investigated further. DIFFERENTIATION OF RED BLOOD CELLS, HEMOGLOBIN, AND MYGLOBIN IN URINE FINDINGS Reagent dipstick Red blood cells in sediment Urine appearance Plasma/serum appearance Total serum CK RED CELLS Positive Present HEMOGLOBIN Positive Absent (few) MYOGLOBIN Positive Absent (few) Cloudy Red Normal Clear Red Pink to Red (hemolysis) Clear Red-brown Normal Normal Total serum LD LD isoenzymes 1 and 2 LD isoenzymes 4 and 5 Normal Normal Normal Slight elevation (10x normal upper limit) Elevated Elevated Normal Marked elevation (40x normal upper limit) Elevated Normal Elevated Limitations: Blood: False-positive Results: 1) Strong oxidizing cleaning agents such as chlorine beach cause false-positive results because of oxidation of the chromogen in the absence of peroxide. 2) Microbial peroxidase activity associated with urinary tract infection may result in a positive reaction. 3) Blood as a contaminant from menstruation will give positive results of no clinical significance. False-negative Results: 1) Formalin used as a preservative, large amounts of nitrite (more than 10 mg/dl), and treatment with captopril (an antihypertensive). 2) Elevated specific gravity (high salt concentration) and elevated protein levels may reduce the lysis of red cells. 3) Testing the supernatant urine from centrifugation or settling when only; a few intact red cells are present. 4) Ascorbic acid (generally more than 25 mg/dl) which is above the reasonable or normal levels. Protein: False-positive Results: 1) In strongly basic urine (pH 9 or higher). 2) During therapy with phenazopyridine. 3) When infusions of polyvinylpyrrolidone (blood substitutes) are administered. 4) When residues of disinfectants containing quaternary ammonium groups or chlorohexidine are present in the urine container. References: 1. Roche Diagnostics: Chemstrip 10 UA Package Insert, Roche Diagnostics, Indianapolis, IN., 1999. 2. Hycor Biomedical: Kova-Trol: Human Urinalysis Controls Package Insert, Hycor Biomedical LTD., Garden Grove, CA., 07/03. 3. Burtis, Carl A., Ashwood, Edward R.: Tietz Textbook of Clinical Chemistry, 2nd edition, pg 2085, 1994. 4. Ringsrud, Karen, Linne, Jean: Urinalysis and Boddy Fluids: A Colortext and Atlas, MosbyYear Book, Inc., St. Louis, MO., pg 55 – 57, 1995. 5. Henry, John: Clinical Diagnosis and Management by Laboratory Methods, 17th edition, W. B. Saunders Co., Philadelphia, PA., pg 418 – 419, 1984.