Cholinergic drug
advertisement

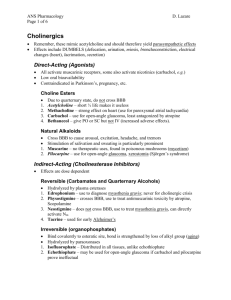
Cholinergic Acetylcholine The word choline generally refers to the various quaternary ammonium salts containing the N,N,N-trimethylethanolammonium cation. Found in most animal tissues, choline is a primary component of acetylcholine, the neurotransmitter, and functions with inositol as a basic constituent of lecithin. It prevents fat deposits in the liver and facilitates the movement of fats into the cells. The richest sources of choline are liver, kidneys, brains, wheat germ, brewer's yeast, and egg yolk. Therefore, cholinergic often refers to the neurotransmitter acetylcholine,[1] and is typically used in a neurological perspective. The parasympathetic nervous system, which uses acetylcholine almost exclusively to send its messages, is said to be almost entirely cholinergic. Neuromuscular junctions, preganglionic neurons of the sympathetic nervous system, the basal forebrain, and brain stem complexes are also cholinergic. In addition, the receptor for the merocrine sweat glands are also cholinergic since acetylcholine is released from post ganglionic sympathetic neurons. In neuroscience and related fields, the term cholinergic is used in the following related contexts: A substance (or ligand) is cholinergic if it is capable of producing, altering, or releasing acetylcholine ("indirect-acting") or mimicking its behaviour at one or more of the body's acetylcholine receptor types ("direct-acting"). A receptor is cholinergic if it uses acetylcholine as its neurotransmitter.[2] A synapse is cholinergic if it uses acetylcholine as its neurotransmitter. Cholinergic drug Structure Activity Relationship for Cholinergic Drugs 1. molecule must possess a Nitrogen atom capable of bearing a positive charge, preferably a quarternary ammonium salt. 2. for maximum potency, the size of the alkyl groups substituted on the Nitrogen should not exceed the size of a methyl group. 3. The molecule should have an oxygen atom, preferably an ester-like oxygen capable of participating in a hydrogen bond. 4. There should be a two-carbon unit between the oxygen atom and the nitrogen atom. A cholinergic drug, also known as a cholinergic agent, cholinergic agonist,[4] or a parasympathomimetic drug,[5] is any drug that functions to enhance the effects mediated by acetylcholine in the central nervous system, the peripheral nervous system, or both. These include acetylcholine's precursors and cofactors, acetylcholine receptor agonists,acetylcholinesterase inhibitors and cholinergic enzymes: Acetylcholine receptor agonists o Alvameline o Muscarine (muscarinic receptors) o Nicotine (nicotinic receptors) o Pilocarpine (M3 receptors) o Suxamethonium (muscle type receptors) From Wikipedia, the free encyclopedia Jump to: navigation, search The N,N,N-trimethylethanolammonium cation, with an undefined counteranion, X− Acetylcholine The word choline generally refers to the various quaternary ammonium salts containing the N,N,N-trimethylethanolammonium cation. Found in most animal tissues, choline is a primary component of acetylcholine, the neurotransmitter, and functions with inositol as a basic constituent of lecithin. It prevents fat deposits in the liver and facilitates the movement of fats into the cells. The richest sources of choline are liver, kidneys, brains, wheat germ, brewer's yeast, and egg yolk. Therefore, cholinergic often refers to the neurotransmitter acetylcholine,[1] and is typically used in a neurological perspective. The parasympathetic nervous system, which uses acetylcholine almost exclusively to send its messages, is said to be almost entirely cholinergic. Neuromuscular junctions, preganglionic neurons of the sympathetic nervous system, the basal forebrain, and brain stem complexes are also cholinergic. In addition, the receptor for the merocrine sweat glands are also cholinergic since acetylcholine is released from post ganglionic sympathetic neurons. In neuroscience and related fields, the term cholinergic is used in the following related contexts: A substance (or ligand) is cholinergic if it is capable of producing, altering, or releasing acetylcholine ("indirect-acting") or mimicking its behaviour at one or more of the body's acetylcholine receptor types ("direct-acting"). A receptor is cholinergic if it uses acetylcholine as its neurotransmitter.[2] A synapse is cholinergic if it uses acetylcholine as its neurotransmitter. Anticholinergic neurotransmitter acetylcholine in the central and the peripheral nervous system. An example of an anticholinergic is dicycloverine, and the classic example is atropine. Anticholinergics are administered to reduce the effects mediated by acetylcholine on acetylcholine receptors in neurons through competitive inhibition. Therefore, their effects are reversible. Anticholinergics are a class of medications that inhibit parasympathetic nerve impulses by selectively blocking the binding of the neurotransmitter acetylcholine to its receptor in nerve cells. The nerve fibers of the parasympathetic system are responsible for the involuntary movements of smooth muscles present in the gastrointestinal tract, urinary tract, lungs, etc. Anticholinergics are divided into three categories in accordance with their specific targets in the central and/or peripheral nervous system: antimuscarinic agents, ganglionic blockers, and neuromuscular blockers. Pharmacology Anticholinergics are classified according to the receptors that are affected: Antimuscarinic agents operate on the muscarinic acetylcholine receptors. The majority of anticholinergic drugs are antimuscarinics. Antinicotinic agents operate on the nicotinic acetylcholine receptors. The majority of these are non-depolarising skeletal muscle relaxants for surgical use, along with a few of the depolarising agents and drugs of other categories structurally related to curare. Examples of anticholinergics: ipratropium bromide (Atrovent) oxitropium bromide (Oxivent) tiotropium (Spiriva) Glycopyrrolate (Robinul) Physostigmine is one of a few drugs that are used as antidotes for anticholinergic poisoning. Nicotine also counteracts anticholinergics. Effects Anticholinergic drugs are used in treating a variety of conditions: Gastrointestinal disorders (e.g., gastritis, pylorospasm, diverticulitis, ulcerative colitis) Genitourinary disorders (e.g., cystitis, urethritis, prostatitis) Respiratory disorders (e.g., asthma, chronic bronchitis) Parkinson's disease and Parkinson-like adverse medication effects Sinus bradycardia - Hypersensitive vagus nerve Insomnia, though usually only on a short term basis. Anticholinergics generally have antisialagogue effects (decreasing saliva production), and most have at least some sedative effect, both being advantageous in surgical proceduresWhen a significant amount of an anticholinergic is taken into the body, a toxic reaction known as acute anticholinergic syndrome may result. This may happen accidentally or intentionally as a consequence of recreational drug use. Anticholinergic drugs are usually considered the least enjoyable by experienced recreational drug users,[citation needed] possibly due to the lack of euphoria caused by them. In terms of recreational use, these drugs are commonly referred to as deliriants. Because most users do not enjoy the experience, they do not use it again, or do so very rarely. The risk of addiction is low in the anticholinergic class. The effects are usually more pronounced in the elderly, due to natural reduction of acetylcholine production associated with age. Exceptions to the above include scopolamine, orphenadrine, dicycloverine/dicyclomine and first-generation antihistamines with central nervous system penetration. Possible effects of anticholinergics include: Ataxia; loss of coordination Decreased mucus production in the nose and throat; consequent dry, sore throat Xerostomia or dry-mouth with possible acceleration of dental caries Cessation of perspiration; consequent decreased epidermal thermal dissipation leading to warm, blotchy, or red skin Increased body temperature Pupil dilation (mydriasis); consequent sensitivity to bright light (photophobia) Loss of accommodation (loss of focusing ability, blurred vision — cycloplegia) Double-vision (diplopia) Increased heart rate (tachycardia) Tendency to be easily startled Urinary retention Diminished bowel movement, sometimes ileus - (decreases motility via the vagus nerve) Increased intraocular pressure; dangerous for people with narrow-angle glaucoma Shaking Possible effects in the central nervous system resemble those associated with delirium, and may include: Confusion Disorientation Agitation Euphoria or dysphoria Respiratory depression Memory problems[2] Inability to concentrate Wandering thoughts; inability to sustain a train of thought Incoherent speech Wakeful myoclonic jerking Unusual sensitivity to sudden sounds Illogical thinking Photophobia Visual disturbances o Periodic flashes of light o Periodic changes in visual field o Visual snow o Restricted or "tunnel vision" Visual, auditory, or other sensory hallucinations o Warping or waving of surfaces and edges o Textured surfaces o "Dancing" lines; "spiders", insects; form constants o Lifelike objects indistinguishable from reality o Hallucinated presence of people not actually there Rarely: seizures, coma, and death Adrenergic agonist An adrenergic agent is a drug, or other substance, which has effects similar to, or the same as, epinephrine (adrenaline). Thus, it is a kind of sympathomimetic agent. Alternatively, it may refer to something which is susceptible to epinephrine, or similar substances, such as a biological receptor (specifically, the adrenergic receptors). Beta blockers block the action of epinephrine and norepinephrine in the body. Adrenergic drugs either stimulate a response (agonists) or inhibit a response (antagonists). The five categories of adrenergic receptors are: α1, α2, β1, β2, and β3, and agonists vary in specificity between these receptors, and may be classified respectively. However, there are also other mechanisms of adrenergic agonism. Epinephrine and norepinephrine are endogenous and broad-spectrum. More selective agonists are more useful in pharmacology. Alpha-adrenergic agonist An adrenergic alpha-agonist (or alpha-adrenergic agonist) is a drug that selectively stimulates alpha adrenergic receptors. The alpha-adrenergic receptor has two subclasses α1 and α2. Classes Although complete selectivity between receptor agonism is rarely achieved, some agents have partial selectivity. α1 agonists Main article: Alpha-1 adrenergic receptor#agonists α1 agonists: stimulates phospholipase C activity. (vasoconstriction and mydriasis; used as vasopressors, nasal decongestants and eye exams). Selected examples are: Methoxamine Methylnorepinephrine Midodrine Oxymetazoline Phenylephrine [1] α2 agonists Main article: Alpha-2 adrenergic receptor#Agonists α2 agonists: inhibits adenylyl cyclase activity. (reduce brainstem vasomotor center-mediated CNS activation; used as antihypertensives, sedatives & treatment of opiate and alcohol withdrawal symptoms). Selected examples are: Clonidine (mixed alpha2-adrenergic and imidazoline-I1 receptor agonist) Guanfacine,[2] (preference for alpha2A-subtype of adrenoceptor) Guanabenz (most selective agonist for alpha2-adrenergic as opposed to imidazoline-I1) Guanoxabenz (metabolite of guanabenz) Guanethidine (peripheral alpha2-receptor agonist) Xylazine,[3] Tizanidine Methyldopa Fadolmidine Beta-adrenergic agonist From Wikipedia, the free encyclopedia Jump to: navigation, search Beta-adrenergic agonists are adrenergic agonists which act upon the beta receptors β1 agonists Main article: Beta-1 adrenergic receptor#agonists β1 agonists: stimulates adenylyl cyclase activity; opening of calcium channel. (cardiac stimulants; used to treat cardiogenic shock, acute heart failure, bradyarrhythmias). Selected examples are: Dobutamine Isoproterenol (β1 and β2) Xamoterol epinephrine β2 agonists β2 agonists: stimulates adenylyl cyclase activity; closing of calcium channel (smooth muscle relaxants; used to treat asthma and COPD). Selected examples are: salbutamol) Fenoterol Formoterol Isoproterenol (β1 and β2) Metaproterenol Salmeterol Terbutaline Clenbuterol Isoetarine pirbuterol procaterol ritodrine epinephrin Beta-adrenergic agonist From Wikipedia, the free encyclopedia Jump to: navigation, search Beta-adrenergic agonists are adrenergic agonists which act upon the beta receptors β1 agonists Main article: Beta-1 adrenergic receptor#agonists β1 agonists: stimulates adenylyl cyclase activity; opening of calcium channel. (cardiac stimulants; used to treat cardiogenic shock, acute heart failure, bradyarrhythmias). Selected examples are: Dobutamine Isoproterenol (β1 and β2) Xamoterol epinephrine β2 agonists Main article: Beta2-adrenergic agonist β2 agonists: stimulates adenylyl cyclase activity; closing of calcium channel (smooth muscle relaxants; used to treat asthma and COPD). Selected examples are: salbutamol (albuterol in USA) Fenoterol Formoterol Isoproterenol (β1 and β2) Metaproterenol Salmeterol Terbutaline Clenbuterol Isoetarine pirbuterol procaterol ritodrine epinephrin Beta-adrenergic agonist From Wikipedia, the free encyclopedia Jump to: navigation, search Beta-adrenergic agonists are adrenergic agonists which act upon the beta receptors β1 agonists Main article: Beta-1 adrenergic receptor#agonists β1 agonists: stimulates adenylyl cyclase activity; opening of calcium channel. (cardiac stimulants; used to treat cardiogenic shock, acute heart failure, bradyarrhythmias). Selected examples are: Dobutamine Isoproterenol (β1 and β2) Xamoterol epinephrine β2 agonists Main article: Beta2-adrenergic agonist β2 agonists: stimulates adenylyl cyclase activity; closing of calcium channel (smooth muscle relaxants; used to treat asthma and COPD). Selected examples are: salbutamol (albuterol in USA) Fenoterol Formoterol Isoproterenol (β1 and β2) Metaproterenol Salmeterol Terbutaline Clenbuterol Isoetarine pirbuterol procaterol ritodrine epinephrin Mixed action Ephedrine Pseudoephedrine Amphetamine (USAN) or amfetamine (INN) is a psychostimulant drug of the phenethylamine class which produces increased wakefulness and focus in association with decreased fatigue and appetite. Brand names of medications that contain, or metabolize into, amphetamine include Adderall, Dexedrine, Dextrostat, Desoxyn, ProCentra, and Vyvanse, as well as Benzedrine in the past. Physical effects of dextroamphetamine can include anorexia, hyperactivity, dilated pupils, blood shot eyes, flushing, restlessness, dry mouth, bruxism, headache, tachycardia, bradycardia, tachypnea, hypertension, hypotension, fever, diaphoresis, diarrhea, constipation, blurred vision, aphasia, dizziness, twitching, insomnia, numbness, palpitations, arrhythmias, tremors, dry and/or itchy skin, acne, pallor, convulsions, and with chronic and/or high doses, seizure, stroke, coma, heart attack and death can occur There is also significant research which highlights the possible neurotoxic effects of amphetamine on the dopaminergic system, even in clinical doses Psychological effects Psychological effects can include euphoria, anxiety, increased libido, alertness, concentration, energy, self-esteem, self-confidence, sociability, irritability, aggression, psychosomatic disorders, psychomotor agitation, grandiosity, excessive feelings of power and superiority, repetitive and obsessive behaviors, paranoia, and with chronic and/or high doses, amphetamine psychosis can occur.[11][12] Withdrawal effects Withdrawal symptoms of amphetamine primarily consist of mental fatigue, mental depression and an increased appetite. Symptoms may last for days with occasional use and weeks or months with chronic use, with severity dependent on the length of time and the amount of amphetamine used. Withdrawal symptoms may also include anxiety, agitation, excessive sleep, vivid or lucid dreams, deep REM sleep and suicidal ideation.[13][14][15] Side effects Contraindications Amphetamine elevates cardiac output and blood pressure making it dangerous for use by patients with a history of heart disease or hypertension. Amphetamine can cause a life-threatening complication in patients taking MAOI antidepressants. The use of amphetamine and amphetamine-like drugs is contraindicated in patients with narrow-angle glaucoma or anatomically narrow angles. Like other sympathomimetic amines, amphetamine can induce transient mydriasis. In patients with narrow angles, pupillary dilation can provoke an acute attack of angle-closure glaucoma. These agents should also be avoided in patients with other forms of glaucoma, as mydriasis may occasionally increase intraocular pressure. Amphetamine has been shown to pass through into breast milk. Because of this, mothers taking amphetamine are advised to avoid breastfeeding during their course of treatment Dependence and addiction Tolerance is developed rapidly in amphetamine abuse; therefore, periods of extended use require increasing amounts of the drug in order to achieve the same effect Overdose An amphetamine overdose is rarely fatal but can lead to a number of different symptoms, including psychosis, chest pain, and hypertension. Tyramine (4-Hydroxyphenethylamine; para-Tyramine; Mydrial, Uteramin) is a naturally-occurring monoamine compound and trace amine derived from the amino acid tyrosine.[1] Tyramine acts as a catecholamine (dopamine, norepinephrine (noradrenaline), epinephrine (adrenaline)) releasing agent. Notably, however, it is unable to cross the blood-brain-barrier (BBB), resulting in only non-psychoactive peripheral sympathomimetic effects. When ingested unintentionally from certain foods in conjunction with a monoamine oxidase inhibitor (MAOI), tyramine is responsible for the so-called "cheese effect" often seen with their use. Occurrence Tyramine occurs widely in plants and animals and is metabolized by the enzyme monoamine oxidase. In foods, it is often produced by the decarboxylation of tyrosine during fermentation or decay. Foods containing considerable amounts of tyramine include meats that are potentially spoiled or pickled, aged, smoked, fermented, or marinated (some fish, poultry, and beef); most pork Physical effects and pharmacology Physiologically metabolized by MAOA. In humans, if monoamine metabolism is compromised by the use of monoamine oxidase inhibitors (MAOIs) and foods high in tyramine are ingested, a hypertensive crisis can result as tyramine can cause the release of stored monoamines, such as dopamine, norepinephrine, epinephrine. The first signs of this were discovered by a neurologist who noticed his wife, who at the time was on MAOI medication, had severe headaches when eating cheese. For this reason, the crisis is still called the "cheese syndrome" even though other foods can cause the same problem]. Most processed cheeses do not contain high enough tyramine to cause hypertensive effects, although some aged cheeses (such as Stilton cheese) do. A large dietary intake of tyramine (or a dietary intake of tyramine while taking MAO inhibitors) can cause the 'tyramine pressor response,' which is defined as an increase in systolic blood pressure of 30 mmHg or more. The displacement of norepinephrine (noradrenaline) from neuronal storage vesicles by acute tyramine ingestion is thought to cause the vasoconstriction and increased heart rate and blood pressure of the pressor response. In severe cases, adrenergic crisis can occur. However, if one has had repeated exposure to tyramine, there is a decreased pressor response; tyramine is degraded to octopamine, which is subsequently packaged in synaptic vesicles with norepinephrine (noradrenaline). Therefore, after repeated tyramine exposure, these vesicles contain an increased amount of octopamine and a relatively reduced amount of norepinephrine (noradrenaline). When these vesicles are secreted upon tyramine ingestion, there is a decreased pressor response, as less norepinephrine (noradrenaline) is secreted into the synapse, and octopamine does not activate alpha or beta adrenergic receptors. When using a MAO inhibitor (MAOI), the intake of approximately 10 to 25 mg of tyramine is required for a severe reaction compared to 6 to 10 mg for a mild reaction. The possibility that tyramine acts directly as a neurotransmitter was revealed by the discovery of a G protein-coupled receptor with high affinity for tyramine, called TA1. The TA1 receptor is found in the brain as well as peripheral tissues, including the kidney. The existence of a receptor with high affinity for tyramine supports the hypothesis that tyramine may also act directly to affect blood pressure regulation. Dietary tyramine intake has also been associated with migraine in select populations, leading many sufferers to restrict foods high in tyramine. Reports on the tyramine-migraine link have been both affirmed and denied. A 2007 review published in Neurological Sciences[4] presented data showing that migraine and cluster headaches are characterised by an increase of circulating neurotransmitters and neuromodulators (including tyramine, octopamine and synephrine) in the hypothalamus, amygdala and dopaminergic system. Adrenergic antagonist An Adrenergic antagonist is a pharmaceutical substance that acts to inhibit the action of the adrenergic receptors. It is thus a type of sympatholytic. It has the opposite effect as adrenergic agonists. More specifically, they can be divided into: Alpha blockers Beta blockers Alpha blocker α blockers or (adrenergic) α-antagonists are pharmacological agents that act as antagonists of α adrenergic receptors (α-adrenoceptors).[1] Classification α1 blockers or antagonists act at α1-adrenoceptors α2 blockers or antagonists act at α2-adrenoceptors When the term "alpha blocker" is used without further qualification, it sometimes refers to α1 blockers, and sometimes refers to agents that act at both types of receptorsGuanfacine, Clonidine and Prazosin are examples of Alpha Blockers. Non-selective α-adrenergic blockers include: Phenoxybenzamine Phentolamine . Uses α blockers are used in the treatment of several conditions, such as Raynaud's disease, hypertension, and scleroderma.[2] Alpha Blockers can also be used to treat anxiety and panic, such as Generalized Anxiety Disorder, Panic Disorder or PTSD. Alpha2-adrenergic receptor agonists, such as clonidine and guanfacine, act at noradrenergic autoreceptors to inhibit the firing of cells in the locus ceruleus, effectively reducing the release of brain norepinephrine (3). Clonidine has shown promise among patients with Anxiety, Panic and PTSD in clinical trials and was used to treat severely and chronically abused and neglected preschool children. It improved disturbed behavior by reducing aggression, impulsivity, emotional outbursts, and oppositionality (4). Insomnia and nightmares were also reported to be reduced. Kinzie and Leung (5) prescribed the combination of clonidine and imipramine to severely traumatized Cambodian refugees with Anxiety, Panic and PTSD. Global symptoms of PTSD were reduced among sixty-six percent and nightmares among seventy-seven percent. Guanfacine produces less sedation than clonidine and thus may be better tolerated. Guanfacine reduced the trauma-related nightmares (6). A recently completed randomized double-blind trial among veteran patients with chronic PTSD showed that augmentation with guanfacine was associated with improvement in anxiety and PTSD.nightmares, as well as overall Anxiety and PTSD symptoms. Beta blocker Beta blockers (sometimes written as β-blockers) or beta-adrenergic blocking agents, beta-adrenergic antagonists, or beta antagonists, are a class of drugs used for various indications, but particularly for the management of cardiac arrhythmias, As beta adrenergic receptor antagonists, they diminish the effects of epinephrine (adrenaline), significant use of beta blockers with propranolol and pronethalol; it revolutionized the medical management of angina pectoris[5] and is considered by many to be one of the most important contributions to clinical medicine and pharmacology of the 20th century Beta blockers block the action of endogenous catecholamines (epinephrine (adrenaline) and norepinephrine (noradrenaline) in particular), on β-adrenergic receptors, part of the sympathetic nervous system which mediates the "fight or flight" response.[7][8] There are three known types of beta receptor, designated β1, β2 and β3 receptors.[9] β1-adrenergic receptors are located mainly in the heart and in the kidneys.[8] β2-adrenergic receptors are located mainly in the lungs, gastrointestinal tract, liver, uterus, vascular smooth muscle, and skeletal muscle.[8] β3-adrenergic receptors are located in fat cells.[10] β-Receptor antagonism Stimulation of β1 receptors by epinephrine induces a positive chronotropic and inotropic effect on the heart and increases cardiac conduction velocity and automaticity Stimulation of β1 receptors on the kidney causes renin release. Stimulation of β2 receptors induces smooth muscle relaxation, induces tremor in skeletal muscle and increases glycogenolysis in the liver and skeletal muscle Stimulation of β3 receptors induces lipolysis. Beta blockers inhibit these normal epinephrine-mediated sympathetic actions but have minimal effect on resting subjects]. That is, they reduce excitement/physical exertion on heart rate and force of contraction,] and also tremo and breakdown of glycogen, but increase dilation of blood vessels] and constriction of bronchi. It is therefore expected that non-selective beta blockers have an antihypertensive effect The primary antihypertensive mechanism of betablockers is unclear but it may involve reduction in cardiac output (due to negative chronotropic and inotropic effects It may also be due to reduction in renin release from the kidneys, and a central nervous system effect to reduce sympathetic activity (for those β-blockers that do cross the blood-brain barrier, e.g. Propranolol). Antianginal effects result from negative chronotropic and inotropic effects, which decrease cardiac workload and oxygen demand. Negative chronotropic properties of beta blockers allow the lifesaving property of heart rate control. Beta blockers are readily titrated to optimal rate control in many pathologic states. The antiarrhythmic effects of beta blockers arise from sympathetic nervous system blockade – resulting in depression of sinus node function and atrioventricular node conduction, and prolonged atrial refractory periods. Sotalol, in particular, has additional antiarrhythmic properties and prolongs action potential duration through potassium channel blockade. Blockade of the sympathetic nervous system on renin release leads to reduced aldosterone via the renin angiotensin aldosterone system with a resultant decrease in blood pressure due to decreased sodium and water retention. Intrinsic sympathomimetic activity Also referred to as intrinsic sympathomimetic effect, this term is used particularly with beta blockers that can show both agonism and antagonism at a given beta receptor, depending on the concentration of the agent (beta blocker) and the concentration of the antagonized agent (usually an endogenous compound such as norepinephrine). See partial agonist for a more general description. Some beta blockers (e.g. oxprenolol, pindolol, penbutolol and acebutolol) exhibit intrinsic sympathomimetic activity (ISA). These agents are capable of exerting low level agonist activity at the β-adrenergic receptor while simultaneously acting as a receptor site antagonist. These agents, therefore, may be useful in individuals exhibiting excessive bradycardia with sustained beta blocker therapy. Agents with ISA are not used in post-myocardial infarction as they have not been demonstrated to be beneficial. They may also be less effective than other beta blockers in the management of angina and tachyarrhythmia.[23] α1-Receptor antagonism Some beta blockers (e.g. labetalol and carvedilol) exhibit mixed antagonism of both β- and α1-adrenergic receptors, which provides additional arteriolar vasodilating action. Other effects Beta blockers decrease nocturnal melatonin release, perhaps partly accounting for sleep disturbance caused by some agents. Beta blockers protect against social anxiety] "Improvement of physical symptoms has been demonstrated with betablockers such as propranolol; however, these effects are limited to the social anxiety experienced in performance situations] (example: an inexperienced symphony soloist) They can also be used to treat glaucoma because they decrease intraocular pressure by lowering aqueous humor secretion. Clinical use Large differences exist in the pharmacology of agents within the class, thus not all beta blockers are used for all indications listed below. Indications for beta blockers include: Angina pectoris Atrial fibrillation Cardiac arrhythmia Congestive heart failure Essential tremor Glaucoma Hypertension Migraine prophylaxis Mitral valve prolapse Myocardial infarction Phaeochromocytoma, in conjunction with α-blocker Symptomatic control (tachycardia, tremor) in anxiety and hyperthyroidism Beta blockers have also been used in the following conditions: Acute aortic dissection Hypertrophic obstructive cardiomyopathy Marfan syndrome (treatment with propranolol slows progression of aortic dilation and its complications) Prevention of variceal bleeding in portal hypertension Possible mitigation of hyperhidrosis Social anxiety disorder and other anxiety disorders Congestive heart failure Although beta blockers were once contraindicated in congestive heart failure, as they have the potential to worsen the condition, studies in the late 1990s showed their efficacy at reducing morbidity and mortality in congestive heart failure. Bisoprolol, carvedilol and sustained-release metoprolol are specifically indicated as adjuncts to standard ACE inhibitor and diuretic therapy in congestive heart failure. Beta blockers are primarily known for their reductive effect on heart rate, although this is not the only mechanism of action of importance in congestive heart failure]. Beta blockers, in addition to their sympatholytic B1 activity in the heart, influence the renin/angiotensin system at the kidneys. Beta blockers cause a decrease in renin secretion, which in turn reduce the heart oxygen demand by lowering extracellular volume and increasing the oxygen carrying capacity of blood. Beta blockers sympatholytic activity reduce heart rate, thereby increasing the ejection fraction of the heart despite an initial reduction in ejection fraction. Trials have shown that beta blockers reduce the absolute risk of death by 4.5% over a 13 month period. As well as reducing the risk of mortality, the number of hospital visits and hospitalizations were also reduced in the trials. Anxiety and performance enhancement There is clear evidence from many controlled trials in the past 25 years that beta blockers are effective in anxiety disorders, though the mechanism of action is not known. Some people have used beta blockers for performance enhancement, and especially to combat 'performance anxiety'. In particular, musicians, public speakers, actors, and professional dancers, have been known to use beta blockers to avoid stage fright and tremor during public performance and especially auditions. The physiological symptoms of the fight/flight response associated with performance anxiety and panic (pounding heart, cold/clammy hands, increased respiration, sweating, etc.) are significantly reduced, thus enabling anxious individuals to concentrate on the task at hand. Stutterers also use beta blockers to avoid fight/flight responses, hence reducing the tendency to stutter. Since they promote a lower heart rate and reduce tremor, beta blockers have been used by some Olympic marksmen to enhance performance, though beta blockers are banned by the International Olympic Committee (IOC). Although they have no recognisable benefit to most sports, it is acknowledged that they are beneficial to sports such as archery and shooting. A recent, high-profile transgression took place in the 2008 Summer Olympics, where 50 metre pistol silver medallist and 10 metre air pistol bronze medallist Kim Jong-su tested positive for propranolol and was stripped of his medal.