LIVING WITH BREATHLESSNESS PROGRAMME
advertisement

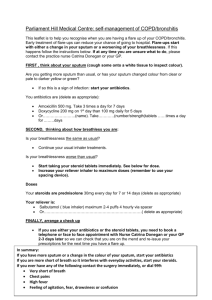
LIVING WITH BREATHLESSNESS PROGRAMME. Operational Plan. Introduction. It is recognised that breathlessness is a problem commonly experienced by people with lung cancer. Breathlessness in advanced lung cancer is reported by Muers (1993) to be found in 75% of patients and is a symptom that is often poorly controlled. emotional and social implications for those who experience it. Breathlessness has physical, There is evidence that an integrated, multi-dimensional approach to assessment combined with supportive interventions including breathing control, actively pacing, relaxation techniques and psychosocial support can lead to improvements in the experience of breathlessness, performance status and physical and emotional wellbeing (Bredin, Corner, Krishnasamy, Plant, Bailey and A‘Hern 1999). This approach can offer patients an individualised approach to help them cope with breathlessness. The SIGN guidelines on the Management of Lung Cancer (1998) recommend that adaptation, coping strategies and breathing control techniques should be an integral part of treatment. This is a proposal to pilot a breathlessness programme. This is a joint initiative between staff of NHS Grampian. The pilot will run for six months and will then be evaluated. Oaks.BreathProg.OpPol. WE/mh.2004 Aim and Objectives. Aim. To provide a supportive intervention to people with lung cancer experiencing breathlessness to assist them to achieve their physical, emotional, social and spiritual potential. Objectives. To undertake a holistic assessment of the experience of breathlessness for each individual. To assist patients, through a structured programme of interventions, to identify and use strategies to reduce their perception of breathlessness. To evaluate the effectiveness of these interventions on the patient’s perception of breathlessness and on their quality of life. Programme Establishment. The programme will operate one afternoon a week in The Oaks’ Palliative Care Day Unit. This facility offers access to consulting rooms and areas suitable for relaxation therapy, including the Snoezelen room. Use of two interview rooms within the Day Care Centre has been secured. Access from the car park is a short walk. Transport to the clinic. Patients will be encouraged to make full use of their own transport. Clinic staff The core clinic staff will be one Macmillan Nurse for Specialist Palliative Care and one Community / Hospital Nurse Manager. It is envisaged that a flexible programme will be developed. Medical input. The General Practitioner will remain lead clinician or patients in the community. Number of patients. A maximum of four patients per week will be seen at each session. Patients will be invited to bring their carer or other relative with them. 2 Referrals. Referrals to the clinic should be made following medical assessment, to exclude all reversible causes of breathlessness and with agreement from the lead clinician. Referrals can be made via the Macmillan Clinic Nurse Specialist, Specialist Palliative Care Services. (Appendix 1 Common Referral Point Form) Self-referrals to the Breathlessness Programme will be considered on an individual basis in consultation with their healthcare team. Patients will have primary lung cancer or mesothelioma. Patients should be well enough to attend on a weekly basis for four weeks. Patients will identify breathlessness as a problem for them. Patients will have completed first line treatment and all other treatable causes of breathlessness considered. The Intervention. Patients will be invited to attend a flexible programme on an out-patient basis. This programme will include breathlessness assessment using the assessment guide developed by the Centre for Cancer and Palliative Studies. Strategies for breathing control, activity pacing and anxiety management, including relaxation and visualisation will be offered in a supportive environment. The intervention will take an approach that focuses on rehabilitation and introduction of strategies to help people cope with the experience of breathlessness. The programme will be flexible and can be adjusted to individual needs. The series of booklets, CD’s and audio tapes on breathlessness, produced by Macmillan Cancer Relief will be used. (Appendix 2) Communication. This programme is intended for patients who are living at home. remain the lead clinician. The General Practitioner will Communication will be maintained with the Primary Healthcare Team and the Cancer Team. Following the first visit, a letter will be sent to the General Practitioner and the Cancer Team. These parties will also be informed on completion of attendance. 3 Patient Records. Patient records will be maintained for patients attending the programme and will be held within The Oaks’ records whilst the patient is participating. Evaluation. The programme will be evaluated by gathering data during assessment, goal-setting and intervention. The tools to be used are visual analogue scale of distress caused by breathlessness, the Hospital Anxiety and Depression Scale and Symptom Checklist. User feedback will also be obtained using patient and carer questionnaires. A report will be compiled at the end of the pilot. 4 APPENDIX 1. The Oaks, Palliative Care Day Centre Morriston Road, Elgin. Referral Form - Breathlessness Programme. Date referral received…………………………………. Taken by ………………………………… PATIENT DETAILS: Name …………………………………………………… d.o.b………………………………………. Address……………………………………………………………………………………………………… ……………………………………………………………………………………………………………….. Telephone No…………………………………………... Main Care………………………………………………. Relationship……………………………… Address………………………………………………………………………………………………………. Next of Kin………………………………………………………………………………………………….. Relationship…………………………………………….. Tel. No……………………………………. Address……………………………………………………………………………………………………… ……………………………………………………………………………………………………………….. General Practitioner………………………………….. Tel. No…………………………………… District Nurse…………………………………………… Tel. No…………………………………… Macmillan Nurse………………………………………………………………………………….……….. Oncologist / Palliative / Hospital Consultant …………………………………………………………… ………………………………………………………………………………………………………………. Unit Number…………………………………………… Diagnosis: Advanced/Recurrence/Other (please circle). Primary………………………………………………….. Date of diagnosis……………………….. Secondaries………………………………………………………………………………………………… Other significant medical history…………………………………………………………………………. ……………………………………………………………………………………………………………….. ……………………………………………………………………………………………………………….. 5 Page 2 … Investigations and Treatment Surgery………………………………………………………………………………………………………. Radiotherapy………………………………………………………………………………………………… Chemotherapy………………………………………………………………………………………………. X-ray………………………………………………………………………………………………………….. Scan………………………………………………………………………………………………………….. Anything else of note……………………………………………………………………………………….. Source of Referral ………………………………………………………………………………………………………………… Has patient’s permission for referral been given? Yes No Is patient aware of diagnosis? Yes No Is carer aware of diagnosis? Yes No Is patient/carer aware of referral? Yes No Reason for referral / Problems at present: Current Medication. Signature of Doctor/Nurse………………………………………………………………………………… Print name………………………………………………………………………………………………….. Date………………………………………… Urgency…………………………………………………………………………………………………….. 6 APPENDIX 2. Programme of intervention. Week 1 Breathlessness assessment. Completion of baseline assessment tools. Introduction of coping strategies and breathing techniques. Goal setting. Booklet 1. Coping with shortness of breath. Week 2 Breathing techniques and coping strategies. Management of anxiety and panic. Individualised problem solving and goal setting. Booklet 2. Living with breathlessness. Week 3 Activity pacing. Review of activities of daily living. Breathing techniques and relaxation. Booklet 3. Managing the experience of breathlessness. Week 4 Flexible session depending on patient and carer needs. Relaxation and visualisation. Group session on areas identified by patients and carers. Opportunity for interactive health education session. 7