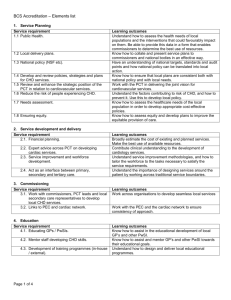
Lambeth and Southwark Adult Breathlessness Assessment Algorithm
advertisement

NHS Lambeth Clinical Commissioning Group NHS Southwark Clinical Commissioning Group Lambeth and Southwark Adult Breathlessness Assessment Algorithm Common Causes of Breathlessness to Consider Focus on co-morbidities Cardiac Respiratory Mental Illness /Addiction Fitness/Lifestyle Anaemia/Kidney disease Everyone who is breathless will have some degree of anxiety If the patient already has a diagnosis causing breathlessness consider at each stable review (or if symptoms worsening) whether this remains the only diagnosis and whether you need to reconsider causation. STEP 1 The history and examination still constitutes 90% of most diagnoses HISTORY Smoking history (pack years) and what is smoked including tobacco, cannabis and other smoked drugs Impact of breathlessness on daily life Levels of habitual physical exercise Environmental and occupational risk factors Acute or Chronic breathlessness Co-morbid conditions/Medications Sleep Quality Mental Health/Psychological Distress Onset of breathlessness associated with identifiable emotional /physical event Consider professional carer support and informal systems around the patient ie. relatives, neighbours etc STEP 2 EXAMINATION Vital signs: BP, Pulse (rate and rhythm), RR, Temperature, oxygen saturation Observe breathing pattern (use of accessory muscles) Auscultate chest & assess airways patency Assessment for peripheral oedema and JVP BMI, waist circumference, neck circumference PEF % predicted (for age, sex and height) Expired carbon monoxide (ppm) Identify Type of Breathlessness (Code breathlessness using READ code 173) Acute severe breathlessness (less than 48 hours) Consider admission (Red Flags: O2<92%, bradycardia OR Chronic persistent breathlessness (daily for more than 6 weeks) Continue to follow breathlessness algorithm <60bpm, tachycardia >100bpm, PEF<33% of best or predicted, RR>30 breath/mn) Provide patients with chronic persistent breathlessness leaflet ‘Taking Charge of your Breathlessness’ STEP 3 Tier 1 Investigations for presentation of chronic breathlessness The minimum tests required for all patients presenting with chronic breathlessness: Full Blood Count Urea & Electrolytes Initial ECG (scan using "photo" setting) Albumin/Creatinine Ratio Consultation Thyroid Function Test NT-ProBNP PHQ4 (screening for anxiety PHQ2 and Peak Flow Diary depression GAD2) – Assess the extent to which anxiety and/or depression are contributing to the breathlessness, and/or associated distress, and/or ability to selfmanage From the tests results identify possible contributory factors to the breathlessness and confirm suspected diagnoses through step 4 investigations Subsequent Consultation Holistic Assessment Liver Function Test Microspirometry (FEV1) Chest X-ray (if not done within last 6 months) Breathlessness Score – MRC Scale STEP 4 Tier 2 Investigations for presentation of chronic breathlessness Based on history, examination and tier 1 investigations should further tests be carried out to confirm diagnoses or to provide further information? Only order tests if you would act upon the results. Common Causes of Breathlessness Cardiac Further Examinations/Tests Possible Diagnoses/Reasons for Breathlessness If raised BNP refer via choose and book to one stop heart failure clinic to diagnose or exclude heart failure (echo and specialist opinion together) Consider 24/7 day tape if patient has intermittent symptoms – palpitations/falls/dizziness Consider Echocardiogram if murmur/abnormal BNP/abnormal chest x-ray/abnormal ECG Consider stress/exercise echocardiography if exertional dyspnoea along with an assessment of cardiovascular risk Consider using GSTFT Cardiology Choose & Book advice and guidance option for opinion on further investigations Referral to diagnostic spirometry if FEV1 < 80% predicted Consider using the respiratory single point of referral for advice and guidance on further investigations and onward management Heart failure Angina-equivalent Valve disease Arrhythmia Ischemic heart disease Respiratory Mental Illness and Addiction GAD 7 and PHQ9 Addiction assessment Obstructive airways disease ILD Obesity Scoliosis Neuromuscular pulmonary hypertension hyperventilation poor home air quality eg damp/no ventilation Anxiety and/or depression hyperventilation Fitness and Lifestyle Audit score for alcohol Eat Well Plate and Food Diary (template on Southwark Intranet) If available use 7 day pedometer assessment for patients with MRC 1-3 Use Short Physical Performance Battery (SPPB), including the 4 Meter Gait Speed Test to assess frailty with patients with MRC 4-5 low levels of fitness obesity smoking/alcohol Use choose and book advice and guidance option to get further opinion from a nephrologist or haematologist before testing or referral Malignancy Deficiency anaemia Renal Failure Chronic disease anaemia Anaemia/Kidney Disease STEP 5 Consider Contributing Factors to Breathlessness There may be more than one contributing factor to breathlessness. Breathlessness is likely to be multi-factorial without a single specific diagnosis. If a physical cause is identified still consider whether psychological factors are contributing to or a consequence of the breathlessness. Order each of the possible contributory factors for the chronic breathlessness (Cardiac/Respiratory/mental Illness/Fitness and Lifestyle/Anaemia and Kidney Disease) this allows prioritisation of investigations, treatments plans and referrals. Revisit relative weighting to each of the possible contributory factors for the breathlessness at each review. If there are no obvious cause(s) of breathlessness identified it is likely that fitness and lifestyle factors need to be addressed. If you have worked through this algorithm with your patient and come to this conclusion it is reasonable now to refer for therapeutic interventions for quitting smoking, alcohol reduction, weight management, physical activity improvement and psychosocial support. Collaboratively agree goals/care plan. Guideline Adapted from IMPRESS Breathlessness Algorithm http://www.impressresp.com/index.php?option=com_docman&Itemid=82 Guideline Agreed July 2014 (Review date: January 2015)