Disease Modifying Drugs in Inflammatory Bowel Disease (IBD)
advertisement

DISEASE MODIFYING DRUGS IN INFLAMMATORY BOWEL DISEASE
Dr A.F. Muller DM FRCP
Consultant Gastroenterologist
On behalf on the Inflammatory Bowel Disease Committee of the
BRITISH SOCIETY OF GASTROENTEROLOGY
1
DISEASE MODIFYING DRUGS IN INFLAMMATORY BOWEL DISEASE
This document is designed to provide information for Gastroenterologists, Primary
Care Clinicians and patients with IBD regarding the use of disease modifying drugs,
their indications, side effects and guidelines for safe monitoring. This document does
not cover the use of biological agents whose use is considered elsewhere.
It is expected that this information will be made available on the British Society of
Gastroenterology and Crohn’s and Colitis Association websites.
INDEX
1. Azathioprine / 6 Mercaptopurine
2. Ciclosporin
3. Methotrexate
4. 5-Amino Salicylates
2
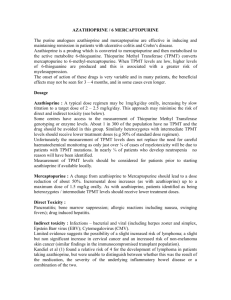
AZATHIOPRINE / 6 MERCAPTOPURINE
The purine analogues azathioprine and mercaptopurine are effective in inducing and
maintaining remission in patients with ulcerative colitis and Crohn’s disease.
Azathioprine is a prodrug which is converted to mercaptopurine and then metabolised
to the active metabolite 6-thioguanine. Thiopurine Methyl Transferase (TPMT)
converts mercaptopurine to 6-methyl-mercaptopurine. When TPMT levels are low,
higher levels of 6-thioguanine are produced and this is associated with a greater risk
of myelosuppression.
The onset of action of these drugs is very variable and in many patients, the beneficial
effects may not be seen for 3 – 4 months, and in some cases even longer.
Dosage
Azathioprine : A typical dose regimen may be 1mg/kg/day orally, increasing by slow
titration to a target dose of 2 – 2.5 mg/kg/day. This approach may minimise the risk of
direct and indirect toxicity (see below).
Some centres have access to the measurement of Thiopurine Methyl Transferase
genotyping or enzyme levels. About 1 in 300 of the population have no TPMT and the
drug should be avoided in this group. Similarly heterozygotes with intermediate
TPMT levels should receive lower treatment doses (e.g 50% of standard dose
regimen).
Unfortunately the measurement of TPMT levels does not replace the need for careful
haematochemical monitoring as only just over ¼ of cases of myelotoxicity will be due
to patients with TPMT mutations. In nearly ¾ of patients who develop neutropenia
no reason will have been identified.
Measurement of TPMT levels should be considered for patients prior to starting
azathioprine if available locally.
Mercaptopurine : A change from azathioprine to Mercaptopurine should lead to a
dose reduction of about 50%. Incremental dose increases (as with azathioprine) up to
a maximum dose of 1.5 mg/kg orally. As with azathioprine, patients identified as
being heterozygotes / intermediate TPMT levels should receive lower treatment
doses.
Direct Toxicity :
Pancreatitis; bone marrow suppression; allergic reactions including nausea, swinging
fevers); drug induced hepatitis.
Indirect toxicity : Infections – bacterial and viral (including herpes zoster and
simplex, Epstein Barr virus (EBV); Cytomegalovirus (CMV).
Limited evidence suggests the possibility of a slight increased risk of lymphoma; a
slight but non significant increase in cervical cancer and an increased risk of nonmelanoma skin cancer (similar findings in the immunocompromised transplant
population).
Kandiel et al (1) found a relative risk of 4 for the development of lymphoma in
patients taking azathioprine, but were unable to distinguish between whether this was
3
the result of the medication, the severity of the underlying inflammatory bowel
disease or a combination of the two.
The recent reports of six cases of hepato-splenic lymphoma in young people on
combined thiopurine/infliximab therapy for Crohn’s disease is of concern. The
relative contribution of each drug is not clear.
There are very few case reports of an association between cervical cancer and IBD
patients taking azathioprine, although there is more evidence available for patients
with rheumatoid arthritis or systemic lupus erythematosus. There are occasional
reports of IBD patients on immunosuppressive therapy developing skin tumours (2).
Laboratory monitoring
Close long term follow up of Full blood count (FBC) and LFT’s is required in all
patients taking AZA/MP. The risk of a patient developing a drug induced neutropenia
may not occur for many months after starting treatment and this is not accounted for
by variations in TPMT levels.
British Society of Gastroenterology
Recommendation
Pre-treatment
assessment
FBC, U&E, creatinine, LFT’s.
Consider TPMT genetic testing or enzyme
levels.
Avoid treatment if TPMT homozygous
recessive or low enzyme activity
Immunisation with influenza and pneumovax
recommended whilst on treatment
Monitoring
FBC & LFT’s weekly for 4 weeks or when
associated with dose increase
Once the dose, disease and blood monitoring
is stable reduce to 3 monthly
U&E, Creatinine at 4, 12 & 26 weeks, then
yearly
What to do if :
1. Bone marrow suppression occurs : Mild – (WCC > 2.5) – reduce dose of
azathioprine and repeat FBC regularly to confirm improvement; Moderate –
(WCC 1.5 – 2.5) stop azathioprine for 1 week, then consider restarting at
much lower dosage with weekly FBC monitoring; Severe (WCC < 1.5) –
withdraw treatment. If patient pyrexial admit for intravenous antibiotics and
consider use of granulocyte-colony stimulating factor (G-CSF).
2. Patient develops pancreatitis : discontinue treatment
3. Patient develops abnormal LFT’s – withdrawal of the drug usually leads to a
resolution of the abnormalities and a liver biopsy is rarely required. Consider
other causes of abnormal LFT’s.
4. Pregnancy : there is no evidence that azathioprine is teratogenic so the
treatment can be continued. Generally azathioprine should not be started
during pregnancy.
4
Recommendations
- Advise patients to use sunscreens and protective covering to reduce sunlight
exposure.
- Immunisation with LIVE vaccines should be avoided. Influenza and
pneumovax can be given.
- Avoid in patients with hepatitis B/C or history of TB.
- AZA / MP are partly metabolised by xanthine oxidase. Care should be taking
in patients taking allopurinol, as the combination of these drugs may lead to
enhanced effects and increased toxicity. Ideally, the combination of
allopurinol and AZA / MP should be avoided. When the combination is
necessary, the dose of AZA / MP should be reduced by 25% or more to avoid
drug accumulation and toxicity.
- The combination of AZA / MP with amino salicylates can occasionally
increase the risk of neutropenia.
The combination of azathioprine and infliximab treatment is superior to azathioprine
alone for inducing and maintaining remission and complete steroid withdrawal in
steroid dependent patients with active Crohn’s disease (3). However, clearly this
approach carries implications with respect to the increased potential for drug-related
toxicity.
Clear recommendations as to the duration of therapy cannot be drawn from the
available literature. In practice, most physicians now intend to continue therapy for 35 years, and discuss withdrawing azathioprine at this time with the patient. It should
be made clear to patients that there is a degree of uncertainty with respect to longterm toxicity if treatment is continued beyond this time frame.
.
1. Kandiel A et al : Increased risk of lymphoma among inflammatory bowel disease
patients treated with azathioprine and mercaptopurine GUT 2005; 54 : 1121 – 5.
2. Austin AS, Spiller RC. Inflammatory bowel disease, azathioprine and skin cancer :
case report and review of the literature. Eur. J. Gastroenterol. Hepatol. 2001; 13 :
193-4.
3. Lemann M. et al. Infliximab and azathioprine for steroid dependent Crohn’s
disease patients - a randomised placebo controlled trial. Gastroenterology 2006; 130
: 1054 – 61.
5
AZATHIOPRINE / 6-MERCAPTOPURINE TREATMENT FOR IBD
PATIENTS
INFORMATION SHEET
This information leaflet is designed to answer common questions patients ask about
their medicine. Further information can be found in the information leaflet supplied
by the manufacturer or from your pharmacist or doctor.
What are they ? • Azathioprine and 6-Mercaptopurine are immunosuppressant
drugs used in the treatment of inflammatory bowel disease. They are often prescribed
when steroids have proved insufficient in bringing the condition under control. They
allow a reduction in the dose of steroids, but may take 12-16 weeks or more to
become effective.
How is it taken?
• In tablet form, daily. The dosage will be advised by your Gastroenterology specialist
team.
Are there any side effects ?
These drugs are an important part of the treatment of patients with inflammatory
bowel disease, but a small number of patients may experience side effects that will
prevent them from continuing with treatment. Should you develop symptoms that
might be related to your treatment you should discuss them with your Doctor /
Gastroenterologist / IBD nurse specialist. Side effects that you should look out for
include :
• Nausea / vomiting and loss of appetite
• Abdominal pain – should this develop, the drug should be stopped immediately
• Hair loss
• Adverse effects on the blood
• Fever, weakness and fatigue (rare)
• Unusual bleeding / bruising (rare)
• Jaundice (rare)
• Rashes (rare)
• There are no special problems for children taking these medicines.
• Lower doses of these drugs may be used in patients aged over 60 years, as there may
be a slight increased risk of side effects.
• Avoid driving and hazardous work until you have learned how azathioprine /
Mercaptopurine affects you as these drugs occasionally can cause dizziness.
• No known problems with alcohol.
Special monitoring
Whilst taking this treatment, you will need regular blood tests. Once the dose of
treatment is stable, the frequency of blood testing will be reduced. The testing will be
supervised by your Gastroenterology specialist team or in a shared care arrangement
with your General Practitioner.
6
• Full Blood Count (FBC)
• Liver Function Test (LFT)
• Some centres will also arrange a test to measure Thiopurine Methyl Transferase
(TPMT).
FBC and LFT will be checked weekly for four weeks post commencement, then
monthly for two months and three monthly thereafter if the results are stable. Any
change in dosage will require similar monitoring. You may also be asked to have tests
of kidney function from time to time.
Other information :
• Immunisation with LIVE vaccines should be avoided. (Influenza and pneumovax
can be given). Please discuss with your General Practitioner or Hospital specialist
team.
• Sunscreens and or protective clothing should be encouraged to reduce sunlight
exposure.
• Other medicines that you are prescribed may interact with azathioprine or
Mercaptopurine. These include drugs used to treat gout (Allopurinol), the blood
thinning treatment warfarin and certain antibiotics (co-trimoxazole and trimethoprim).
You should discuss these with your Doctor.
Azathioprine / Mercaptopurine in pregnancy and breast feeding ?
Azathioprine is safe to take in pregnancy, although there are reports of premature
birth and low birth-weight babies in mothers taking this treatment.
Women receiving azathioprine treatment ideally should avoid breast feeding.
Although Azathioprine is broken down by the body into Mercaptopurine, the use of
Mercaptopurine is not recommended during pregnancy.
The literature with respect to the safety of thiopurines in men whose partners are planning to
conceive is mixed. Data and clinical experience suggest that the drug is safe in this context,
although an increased risk of malformations have been reported in other series.
Keep all medicines out of the reach of children. Never give any medication prescribed for you
to anyone else. It may harm them even if their symptoms are the same as yours.
For further information you can contact your IBD Nurse Specialist or
Gastroenterology specialist.
7
CICLOSPORIN
Introduction :
The main role for ciclosporin is in the treatment of patients with severe steroid
refractory Ulcerative Colitis. The study by Lichtiger1 demonstrated an 80% response
rate in this group to intravenous ciclosporin. After conversion to oral treatment about
2/3rds of patients were maintained in remission without steroids, with the remaining
1/3 rd proceeding to colectomy.
Response rates are improved by the addition of azathioprine or Mercaptopurine2,3, and
ciclosporin can be used as a bridge for maintenance therapy having a slow onset of
action.
Ciclosporin is of little benefit in Crohn’s disease and should be avoided4.
Ciclosporin may be given either intravenously (2mg/kg/day) or orally in a
microemusion formula (Neoral) in doses between 4.6 – 7.5 mg kg/day.
Cautions :
1. Uncontrolled hypertension
2. Use of potassium sparing diuretics
3. Immunisation with live vaccines should be avoided (Influenza and
pneumovax can be given).
4. Pregnancy and lactation
5. Grape fruit juice – to be avoided within one hour of ingestion
6. Malignancy – such as lymphoma etc
7. Drug interactions : Many drugs interact with ciclosporin (the most important
of which are included below), but refer to BNF / data sheet or your own
Hospital drug information service.
Contraindications :
1. Uncontrolled hypertension
2. Renal and liver failure
3. Severe electrolyte disturbance i.e. hyperkalaemia
4. Suspected systemic infection / sepsis
Monitoring
Oral : Trough (immediately before next dose) ciclosporin levels should be measured
weekly and dosages adjusted accordingly (liase with Clinical Biochemist / Renal Unit
for local therapeutic ranges); Initially, twice weekly – weekly creatinine (and / or
estimated glomerular filtration rate {eGFR}levels. The dose of ciclosporin should be
reduced if creatinine levels increase by more than 20% from baseline.
Ciclosporin levels are affected by many drugs, particularly antibiotics. More frequent
monitoring should take place when new drugs are introduced.
Intravenous : Facilities should be available to monitor ciclosporin and creatinine and
electrolyte levels daily.
Agents likely to increase Ciclopsorin levels
Drug
Calcium channel
Effect
Action
Monitor ciclosporin levels
8
blockers
-Diltiazem, Verapamil,
Nifedipine, Amlodipine
Grapefruit juice
Macrolides
- Clarithromycin
- Erythromycin
Metoclopramide
Oral contraceptives
- Danazol
Tacrolimus
Increase ciclosporin levels
and make dose reductions
as necessary
May increase Ciclosporin
levels
Markedly increase
ciclosporin levels.
Potentially serious
Avoid concurrent use
Increases ciclosporin
levels
Marked increase in
ciclosporin levels with
some oral contraceptives,
particularly Danazol
Increases ciclosporin
levels & increased risk of
renal failure
Avoid if possible
If concurrent use essential,
monitor ciclosporin levels
closely and reduce dose by
1/3 for duration of
macrolide course
Avoid concurrent use if
possible – where
concurrent use essential,
monitor ciclosporin levels
and examine pt for signs of
toxicity
If used in combination,
monitor ciclosporin levels
more frequently, look for
signs of ciclosporin or
hepatotoxicity. Adjust
dosages levels as
necessary.
Avoid concomitant use
1. Lichtiger S, Present DH, Kornbluth A. et al. Cyclosporine in severe ulcerative
colitis refractory to steroid therapy. N. Eng. J. Med. 1994; 330 : 1841-5.
2. Cohen RD, Stein R, Hanauer SB. Intravenous cyclosporin in ulcerative colitis
: a five year experience. Am. J. Gastroenterol. 1999; 94 : 1587-92.
3. Fernandes-Banares F, Bertran X, Esteve-Comas M et al. Azathioprine is
useful in maintaining long-term remission induced by intravenous
cyclosporine in steroid-refractory severe ulcerative colitis. Am. J.
Gastroenterol. 1996; 91 : 2498-9.
4. McDonald JW et al. Cyclosporine for induction of remission in Crohn’s
disease. Cochrane Database Syst Rev. 2005; 18 : CD000297.
9
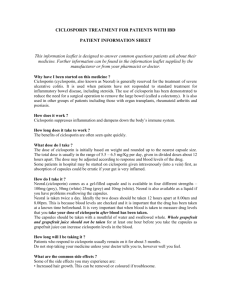
CICLOSPORIN TREATMENT FOR PATIENTS WITH IBD
PATIENT INFORMATION SHEET
This information leaflet is designed to answer common questions patients ask about
their medicine. Further information can be found in the information leaflet supplied
by the manufacturer or from your pharmacist or doctor.
Why have I been started on this medicine ?
Ciclosporin (cyclosporin, also known as Neoral) is generally reserved for the treatment of
severe ulcerative colitis. It is used when patients have not responded to standard treatment for
inflammatory bowel disease, including steroids. The use of ciclosporin has been demonstrated
to reduce the need for a surgical operation to remove the large bowel (called a colectomy). It
is also used in other groups of patients including those with organ transplants, rheumatoid
arthritis and psoriasis.
How does it work ?
Ciclosporin suppresses inflammation and dampens down the body’s immune system.
How long does it take to work ?
The benefits of ciclosporin are often seen quite quickly.
What dose do I take ?
The dose of ciclosporin is initially based on weight and rounded up to the nearest capsule
size. The total dose is usually in the range of 5.5 – 6.5 mg/Kg per day, given in divided doses
about 12 hours apart. The dose may be adjusted according to response and blood levels of the
drug.
Some patients in hospital may be started on ciclosporin given intravenously (into a vein) first,
as absorption of capsules could be erratic if your gut is very inflamed.
How do I take it ?
Neoral.(ciclosporin) comes as a gel-filled capsule and is available in four different strengths –
100mg (grey), 50mg (white) 25mg (grey) and 10mg (white). Neoral is also available as a
liquid if you have problems swallowing the capsules.
Neoral is taken twice a day. Ideally the two doses should be taken 12 hours apart at 8.00am
and 8.00pm. This is because blood levels are checked and it is important that the drug has
been taken at a known time beforehand. It is very important that when blood is taken to
measure drug levels that you take your dose of ciclosporin after blood has been taken.
The capsules should be taken with a mouthful of water and swallowed whole. Whole
grapefruit and grapefruit juice should not be taken for at least one hour before you take the
capsules as grapefruit juice can increase ciclosporin levels in the blood.
How long will I be taking it ?
Patients who respond to ciclosporin usually remain on it for about 3 months.
Do not stop taking your medicine unless your doctor tells you to, however well you feel.
What are the common side effects ?
Some of the side effects you may experience are:
• Increased hair growth. This can be removed or coloured if troublesome.
• Slightly enlarged or sore gums. Your dentist will be able to suggest treatment for this if it is
a problem.
• Shakiness of the hands.
10
• You may feel a little sick in the early stages, possibly with some abdominal discomfort
• Hot or burning sensations in the hands and feet. This normally lessens after a couple of
weeks.
• Metallic taste in the mouth
• Cramps and painful periods. Some women may notice that their periods cease whilst they
are on ciclosporin.
Do I need any special checks while on ciclosporin ?
Ciclosporin can raise your blood pressure and affect the kidneys. We recommend that your
blood pressure, blood count and kidney function are checked every 2-4 weeks for 2 months
then at 1-2 monthly intervals thereafter as appropriate.
What do I do if I experience side effects ?
If you feel unwell, develop a sore throat or any infections or are unsure about a certain
reaction contact your doctor / IBD nurse specialist or pharmacist.
What happens if I forget to take a dose ?
If you forget to take a dose, take another one as soon as you remember, unless it is almost
time for your next dose. Do not double the dose. If you take too much ciclosporin tell your
doctor immediately.
Does ciclosporin interfere with my other medicines ?
Ciclosporin can interact with other medicines including non-steroidal anti-inflammatory drugs
e.g ibuprofen, St John’s Wort and erythromycin. Always check with your doctor or
pharmacist first.
It is safe to drink alcohol in moderation whilst on ciclosporin. Avoid binge drinking as this
can seriously affect blood levels of the drug.
You should avoid having ‘live’ vaccines such as polio. Most travel vaccines and flu vaccines
are, however, acceptable. Discuss with your doctor or pharmacist first.
Is ciclosporin OK in pregnancy and breast feeding ?
If you are planning to become pregnant whilst on ciclosporin you should discuss with your
doctor first. You should not breast feed if you are taking ciclosporin.
Keep all medicines out of the reach of children. Never give any medication prescribed for you
to anyone else. It may harm them even if their symptoms are the same as yours.
For further information you can contact your IBD Nurse Specialist or
Gastroenterology specialist.
11
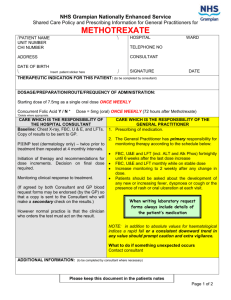
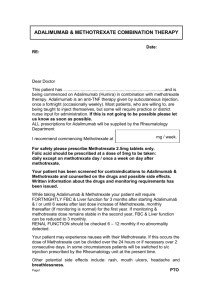
METHOTREXATE
Introduction :
Methotrexate is an immunomodulator used to induce and maintain remission of
Crohn’s disease and Ulcerative colitis in patients who have steroid dependent or
refractory disease, or who have been intolerant of either azathioprine or 6Mercaptopurine. Methotrexate inhibits the enzyme dihydrofolate reductase, essential
for the synthesis of purines and pyrimidines. Although unlicensed to treat
inflammatory bowel disease, methotrexate is widely used in Crohn’s disease (BNF
section 1.5) and less commonly in ulcerative colitis.
Dose and mode of administration :
Much of the evidence for the beneficial effects for methotrexate has been with the
intramuscular route of administration. The evidence for the efficacy and
bioavailability of oral methotrexate is limited in Crohn’s disease, although there is
very good evidence for its efficacy in the treatment of Rheumatoid Arthritis for over
50 years. Many Gastroenterologists are now recommending oral therapy as it is more
convenient for the patient and easier to supervise.
Intramuscular route : 25mg once per week for up to 16 weeks, then reduced to 15mg
once a week.
Oral route : Intially 15mg once per week as a single dose, increasing to 20mg once
per week after 2 weeks and up to a maximum of 25mg once a week after a further 2
weeks as tolerated and according to response.
A lower starting dose may be required for the elderly or frail or those with renal
impairment. Clinical response is usually evident in 4-6 weeks.
Folic acid treatment : Folic acid reduces the toxicity of methotrexate treatment and
improves continuation of therapy and compliance. Folic acid should be taken ONCE
weekly, but SHOULD NOT be taken on the same day as the methotrexate.
Recommended monitoring and precautions / interactions
Monitoring Schedule :
Pre-treatment assessment
British Society of Gastroenterology
recommendation
Avoid use in patients with known liver
disease (including fatty liver), alcohol
excess, obesity, diabetes or women trying
to conceive.
FBC, U&E, LFT’s
Pre-treatment Pulmonary Function Tests
and CXR may be considered for some
12
patients
FBC, U&E, LFT’S every 2 weeks after
the last dose change; thereafter monthly
until stabilised.
Monitoring frequency every 2-3 months if
patients results remain stable
Monitoring
Action to be taken :
9
WBC < 3.5 x 10 /l
Neutrophils < 2.0 x 109/l
Platelets < 150 x 109/l
Withold treatment and recheck in 1 week
Discuss with Specialist team
Withold treatment and recheck in 1 week
Discuss with Specialist team
Withold treatment and recheck in 1 week
Discuss with Specialist team
MCV > 105fl
Check serum B12, folate & TFT and
Discuss with Specialist team
AST, ALT > 2 fold rise (from the upper
limit of the reference range)
Consider for liver biopsy when persistent
elevation occurs.
Discontinue treatment in patients with
abnormal LFT’s who decline liver biopsy
Monitor closely and consider need for
liver biopsy
Nausea occurs commonly & may be
reduced by changing timing of dose
(before bedtime), ensure adequate intake
of folic acid, & consider antiemetic at
time of weekly dose
Albumin – Unexplained fall in the
absence of active disease
Nausea
Rashes or oral ulceration, vomiting &
diarrhoea
Renal function – significant
deterioration compared to baseline or
upper limit of normal of reference
range
Severe sore throat, abnormal bruising
New or increasing dyspnoea or dry
cough
Withold treatment and recheck in 1 week
Discuss with Specialist team
Withold treatment and recheck results
Discuss with Specialist team
Immediate FBC and withhold until the
result of FBC is available
Withold treatment; CXR & pulmonary
function tests;
Discuss with Specialist team
The incidence of hepatotoxicity in patients with inflammatory bowel disease is very
low and particularly so, if the drug is only given to carefully selected patients –
avoiding its use in :
In patients suspected of alcohol abuse;
13
The Obese
Patients with previously demonstrated fatty liver, pre-treatment abnormalities
of liver function and those with pre-existing liver disease
Liver biopsy should be considered when there is a persistent elevation of the
transaminases above baseline or a decrease in the albumin level below the reference
range when the inflammatory disease is inactive.
Methotrexate is contraindicated in patients with significant renal impairment because
the primary mode of excretion of the drug is via the kidneys. Renal toxicity occurs
rarely with methotrexate treatment, but cases of nephrotic syndrome and renal failure
have been described.
Pneumonitis has very rarely been reported in patients with IBD taking methotrexate
treatment. If respiratory symptoms develop whilst a patient is receiving methotrexate
treatment, a CXR and pulmonary function tests should be arranged urgently and the
drug discontinued.
Bone marrow suppression may occur as a result of methotrexate treatment. The risk is
greatest in the elderly and those with significant renal impairment. When a significant
fall in the indices has occurred the following should be arranged immediately :
Stop Methotrexate therapy
Give Folinic Acid Rescue – The initial dose should be at least 20mg given
intravenously. Subsequent doses of 15mg given orally at 6 hourly intervals
until the haematological abnormalities have improved (usually not more than 2
– 8 doses.
Consider immediate discussion with Supervising Specialist team / Medical
On Call team or the local Haematologist.
Pregnancy & Breast feeding :
Methotrexate is both teratogenic and is an abortofacient. Methotrexate may also be
toxic to sperm. Adequate birth control is therefore essential for both men and women.
Contraception (for both sexes) should be continued for at least 3 months after
stopping methotrexate therapy.
Methotrexate may be excreted in breast milk so breast feeding is contraindicated.
Should an inadvertent pregnancy occur, referral should me made to an Obstetrician.
Cautions :
Patients with clinically significant renal impairment from any cause
Localised or systemic infection including hepatitis B & C and past history of
TB
Unexplained anaemia or cytopenia associated with bone marrow failure
Immunisation with live vaccines should be avoided (pneumoccocal and
Influenza vaccinations can be given)
Drug interactions :
o Phenytoin, Co-trimoxazole, Trimethoprim – the antifolate effect of
methotrexate is increased
14
o Probenacid, Penicillin, Azapropazone, NSAID’s – Methotrexate
excretion is reduced (but a clinically significant interaction between
methotrexate and NSAID’s is rare
o Tolbutamide – serum concentrations of methotrexate may be increased
Duration of treatment
As for azathioprine, the duration for continuing treatment with MTX cannot be
recommended from current literature alone. If well-tolerated, the drug may be
continued for several years, under appropriate supervision. Hepatic fibrosis now
seems relatively uncommom in these IBD patients, and liver biopsy is no longer
routinely recommended after 1.5g intake. Serum markers of fibrosis are available in
spcialist centres, if needed. Again, informed discussion with the patient as to the
uncertainties of long-term toxicity are necessary, if therapy continues beyond 3-5
years without attempted withdrawal of the drug.
REFERENCES
1. Feagan.BG, Rochon.J. et al .Methotrexate for the treatment of Crohn’s disease. The
North American Crohn’s study group Investigations.N.Engl.J.Med.1995; 332:292297.
2.Feagan.BG, Fedorak.R et al. A comparison of methotrexate with placebo for the
maintenance of remission in crohn’s disease.N.Engl.J.Med. 2000; 342: 1627-1632.
3. Alfadhli AA, McDonald JW, Feagan BG. Methotrexate for induction of remission
in refractory Crohn’s disease. Cochrane Database Syst. Rev. 2005; (1) : CD003459.
4. Hawthorne AB. Methotrexate : a useful alternative in Crohn’s disease ? Gut 2001;
49 : 9-10.
5. Rampton DS. Methotrexate in Crohn’s disease. Gut 2001; 48 : 790-1.
6.Fraser AG, Morton D, McGovern D, Travis S, Jewell DP. The efficacy of
methotrexate for maintaining remission in inflammatory bowel disease. Aliiment.
Pharmacol. Ther. 2002; 16 : 693-7.
7. Aberra FN, Lichtenstein GR. Review article : monitoring of immunomodulators in
inflammatory bowel disease. Aliment. Pharmacol. Ther. 2005; 21 : 307-19.
8. Siegel CA, Sands BE. Review article : practical management of inflammatory
bowel disease patients taking immunomodulators. Aliment. Pharmacol. Ther. 2005;
22 : 1-16.
9. Sun JH, Das KM. Low-dose oral methotrexate for maintaining Crohn’s disease
remission : where we stand. J. Clin. Gastroenterol. 2005; 39 : 751-6.
10. Kurnik D, Loebstein R, Fishbein E, Almog S, Halkin H, Bar-Meir S, Chowers Y.
Bioavailability of oral vs. subcutaneous low dose methotrexate in patients with
Crohn’s disease. Aliment. Pharmacol. Ther. 2003; 18 : 57-63.
15
METHOTREXATE TREATMENT FOR PATIENTS WITH IBD
PATIENT INFORMATION LEAFLET
This information leaflet is designed to answer common questions patients ask about
their medicine. Further information can be found in the information leaflet supplied
by the manufacturer or from your pharmacist or doctor.
Why have I been started on this medicine ?
• Methotrexate is a medicine used to induce and maintain remission of Crohn’s
disease and Ulcerative colitis in patients who have steroid dependent or refractory
disease, or who have been intolerant of either azathioprine or 6-Mercaptopurine.
How is it taken ?
• In tablet form, weekly or by Intra Muscular injection.
Your Gastroenterology team will decide on the appropriate dose for you as well as
organizing regular blood tests.
To reduce the risk of side effects from methotrexate, you will also be asked to take a
vitamin called Folic Acid once a week (that will also be prescribed for you), but you
should NOT take this on the same day as the methotrexate treatment.
How does it work ?
Methotrexatesuppresses inflammation and dampens down the body’s immune system.
How long does it take to work ?
The benefits of methotrexate treatment often take quite a number of weeks to occur.
How long will I be taking it ?
Patients who respond to methotrexate usually remain on it for many months and perhaps
several years as long as the blood test monitoring remains satisfactory.
Do not stop taking your medicine unless your doctor tells you to, however well you feel.
What are the common side effects ?
Fortunately many patients do not suffer any side effects with this treatment. Some of
the common side effects can be reduced by simple measures :
• Nausea / vomiting – this is perhaps the commonest side effect likely to occur. These
symptoms can often be reduced by taking the drug at a different time of the day – eg
on retiring to bed; by ensuring that you are taking the vitamin supplement called Folic
acid; for some patients, your Specialist will give you a prescription for an antisickness medication to take about an hour before your weekly dose of methotrexate.
Other common side effects include : mouth and nasal ulcers; diarrhoea; abdominal
pain and bloating; fatigue; symptoms of a cold / flu like illness; joint pain; insomnia;
facial flushing; eye irritation; dizziness; mild hair loss; loss of libido / impotence;
decreased fertility (reversible on completion of treatment).
16
Other rare side effects include : headache; acne; skin irritation and itching; increased
sensitivity to light; tingling / numbness; dry cough and / or shortness of breath.
Should you develop any of these troublesome symptoms you should report them to
your specialist Gastroenterology team.
Special monitoring
You will need to undertake a pre treatment screening. The results of which will ensure
suitability. Blood tests will be taken at regular intervals throughout administration of
the drug.
• Do not receive any live vaccines (rubella, polio).
• Avoid contact with people who have infections.
• Avoid pregnancy.
• Contraception is strongly recommended.
• If breastfeeding, this should be stopped as methotrexate passes into breast milk.
• In certain patients, liver biopsy may be required if treatment is ongoing.
Methotrexate and pregnancy
Do not become pregnant whilst taking methotrexate treatment. Because methotrexate
may damage sperm, adequate birth control is essential for both men and women.
Contraception (for both sexes) should be continued for at least 3 months after
stopping methotrexate treatment.
Keep all medicines out of the reach of children. Never give any medication prescribed for you
to anyone else. It may harm them even if their symptoms are the same as yours.
For further information you can contact your IBD Nurse Specialist or
Gastroenterology specialist.
17
DRUGS FOR INFLAMMATORY BOWEL DISEASE
AMINOSALICYLATES (5-ASA)
Included in this group of drugs are : Sulphasalazine, Mesalazine, Olsalazine and
Balsalazide. Comment of mode of action is required ?
Route of administration :
Oral as tablets, granules and suspensions (sulphasalazine only).
Rectally as suppositories or enemas.
Cautions / Contraindications :
Sulphasalazine :
Glucose 6 phosphate dehydrogenase deficiency – may cause haemolysis.
Pregnancy / breast feeding :
Sulphasalazine may be associated with transient reversible oligospermia in men of
child bearing potential.
Folic acid supplements should be prescribed to those trying to conceive and during
pregnancy.
Small amounts of the drug are excreted in breast milk although this is not thought to
be a risk to healthy infants.
Contraindicated in patients with hypersensitivity to sulphonamides / co-trimoxazole.
All 5-ASA’s
Use with caution in patients with renal impairment – and discuss with Nephrology
team & monitor renal function regularly whilst on treatment.
Avoid in patients with severe renal failure.
There is a possible increased risk of haematological toxicity (leucopenia, unexplained
bleeding / bruising and purpura) when patients are taking azathioprine or 6 –
Mercaptopurine – monitor blood tests more frequently.
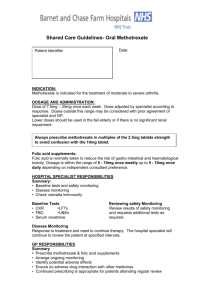
British Society of Gastroenterology (BSG) recommended monitoring schedule :
BSG Guidelines :
Pre-treatment assessment
Monitoring
FBC, U&E, Creatinine, LFT’s
FBC & LFT’s at 1 month
FBC, U&E, Creatinine, LFT’s at 3
months
If results stable repeat above blood
tests about once yearly
18
Following dose changes
Consider repeating bloods 1 month
after increase
Actions to be taken :
Nausea, dizziness, headache, worsening
diarrhoea
Severe abdominal pain
If troublesome, reduce or stop treatment
and consider alternative
Monitor carefully – if WBC continues to
fall, withhold until discussed with
Gastroenterology specialist team
Monitor carefully – if neutrophil count
continues to fall, withhold until discussed
with Gastroenterology specialist team
Monitor carefully – if platelet count
continues to fall, withhold until discussed
with Gastroenterology specialist team
Check amylase level; consider ultrasound
or CT scanning
> 2 fold rise above upper limit of normal
reference range for ALT / AST
Withold until discussed with specialist
team; Ultrasound liver.
Rise of creatinine level above the normal
range (or rise of > 20% compared to
baseline)
Withold until discussed with specialist
team; Urinalysis for proteinuria etc; renal
ultrasound; nephrology opinion.
Check FBC immediately and withhold
until result available. discuss with
Gastroenterology specialist team
Withold; seek urgent specialist
(preferably Dermatological) advice
WBC < 4.0 x 109/l
Neutrophils < 2.0 x 109/l
Platelets < 150 fl
Abnormal bruising or severe sore throat
Unexplained acute widespread rash
1. Ransford RA, Langman MJ. Sulphasalazine and mesalazine : serious adverse
reactions re-evaluated on the basis of suspected adverse reaction reports to the
Committee on Safety of Medicines. Gut 2002; 51 : 536-9.
2. Van Staa TP, Travis S, Leufkens HG, Logan RF. 5-aminosalicylic acids and
the risk of renal disease : a large British epidemiological study.
Gastroenterology 2004; 126 : 1733 – 9.
3. Muller AF, Stevens P, McIntyre AS, Ellison H, Logan RF. Experience of 5aminosalicylate nephrotoxicity in the United Kingdom. Aliment. Pharmacol.
Ther. 2005; 21 : 1217 – 1224.
19
DRUGS FOR INFLAMMATORY BOWEL DISEASE
THE AMINOSALICYLATES (5-ASA)
PATIENT INFORMATION
SHEET
This information leaflet is designed to answer common questions patients ask about
their medicine. Further information can be found in the information leaflet supplied
by the manufacturer or from your pharmacist or doctor.
If you have been diagnosed with Inflammatory Bowel Disease (Crohn’s disease or
Ulcerative Colitis) you may be prescribed an aminosalicylate sometimes called 5ASA (or mesalazine, olsalazine, basalazide, or sulphasalazine). These drugs have a
major role in maintaining remission of ulcerative colitis. Crohn’s disease patients
may also benefit from treatment with these drugs and they are often used to help
reduce the chances of Crohn’s disease recurring after operations.
What are 5-ASA’s ?
They are a group of drugs that work by minimising the degree of inflammation in the
intestine, giving the damaged lining time to heal.
There are several slightly different drugs in this group that all are designed to treat
different areas of the intestine. Your doctor will start you on the one that will give you
the most benefit. It is important that you stick to the same unless your doctor tells you
otherwise.
How are 5-ASA’s given ?
These drugs can be given by mouth (tablets, capsules and granules). For patients
whose colitis is limited to the distal part of the colon, these treatments may prove very
effective when given through the anus by inserting a suppository or enema.
How long will it take to work ?
These drugs do not work straight away. In order to remain in remission, you must
continue to take your mesalazine even if you feel well.
Do I need to take 5-ASAs long term ?
To keep the bowel condition under control and to reduce the risk of flare ups, patients
are usually advised to take these treatments long term.
The risk of bowel cancer in inflammatory bowel disease is slightly increased, but
some studies have suggested that this risk may be reduced by long-term use of 5aminosalicylates.
What dose of 5-ASAs will I be given ?
The dose will be decided by your doctor, and usually depends on how active the
disease is and may be increased or decreased accordingly.
You will usually remain on a dose to help keep your disease under control, this is
known as a maintenance dose.
What are the common side effects ?
20
5-ASAs are effective in the treatment of inflammatory bowel disease but can
occasionally be associated with some side effects, which are usually mild such as
diarrhoea, nausea, vomiting, headaches, and rashes.
Generally however, these drugs are very well tolerated with 90% of patients
experiencing no side- effects.
Very rarely, these drugs can affect the blood, kidneys, liver and pancreas. Rarely
some patients can be allergic or particularly sensitive to 5-ASAs and so it is important
to report any unexplained bleeding, bruising, skin rash, prolonged sore throat or fever.
If this happens sometimes the drug has to be stopped or changed.
Do I need to have blood tests ?
Because these drugs very rarely can cause blood disorders, your Doctor or Nurse
Specialist will arrange for you to have occasional blood checks – these would
normally be done at least once per year but usually sooner (e.g. between 1 - 3 months)
if you have recently started on the drug.
Can I have immunisations whilst taking 5-ASA’s ?
It is safe to have Vaccinations whilst on 5-ASAs.
Can I drink alcohol whilst taking 5-ASA’s ?
There is no reason to avoid alcohol (in moderation) whilst taking 5-ASAs, but it can
sometimes aggravate nausea.
Do 5-ASA’s affect fertility or pregnancy ?
There is one drug called Salazopyrin (sulphasalazine) that is associated with a
reversible reduction of male fertility. Salazopyrin is used less frequently nowadays as
the newer drugs may have fewer side effects. Other 5-ASAs do not affect fertility and
all can be safely taken in pregnancy.
Do these drugs interfere with my other medicines ?
Most drugs can be taken safely, however always check with your doctor or pharmacist
first.
Keep all medicines out of the reach of children. Never give any medication
prescribed for you to anyone else. It may harm them even if their symptoms are the
same as yours.
For further information you can contact your IBD Nurse Specialist or
Gastroenterology specialist.
21
22