OXYGEN TRANSPORT
advertisement
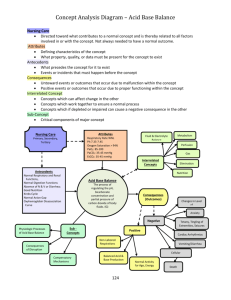
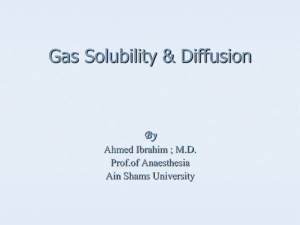
RSPT 1207 – Cardiopulmonary Anatomy & Physiology OXYGEN TRANSPORT Lecture Notes Reference & Reading: Egan’s Chapter 10 The cardiovascular and pulmonary systems share one common function which is the exchange of the gases of metabolism (O2 and CO2). This exchange occurs at several levels. I. KEY TERMINOLOGY a. Ventilation – the bulk transfer of gases into and placement into the alveoli b. Circulation – the bulk transfer of blood c. Perfusion – microcirculation at the capillary level d. Diffusion – the process where gas molecules move from an area of high partial pressure to an area of low partial pressure e. External Respiration – for diffusion to occur there must be an interface of the the single walled alveoli (A) and the single walled capillary (c). this interface is represented as “A-C” f. Internal Respiration – the diffusion of gases between the capillaries and the tissue cells of the body g. Cellular Respiration – the process of ATP formation II. EXTERNAL RESPIRATION a. The exchange of gases at the alveolar-capillary membrane or diffusion of gases b. There are several factors to be considered in the diffusion of gas across between these to entities 1. Pressure Gradient – must be present for gas molecules to diffuse 2. Membrane thickness – the thicker the membrane, less diffusion occurs through the membrane 3. Surface Area – the more surface area available, the more diffusion occurs 4. Composition of the gases – There are some gases that have the ability to dissolve in water easily. Because the composition of the alveolar wall is 90% water and the composition of the blood plasma and the RBC is water the ability for a gas to dissolve in water is clinically significant. Each gas also has a different ability to pass through a membrane based on its density. Smaller molecules diffuse better than larger ones When considering these two factors, each gas can be graded based on its diffusion constant. III. FICK’S LAW OF DIFFUSION – relates to gas transfer across a tissue (membrane) a. The law states: The rate of gas transfer across a sheet of tissue is directly proportional to the surface area of the tissue, diffusion constants and the difference in partial pressure of gas between the two sides of the tissue and is inversely proportional to the thickness of the tissue b. The greater the surface area, diffusion constant, and pressure gradient the more diffusion will occur. c. The larger distance across the membrane, less diffusion will occur. IV. DIFFUSION CONSTANTS – represents a gas’ ability to diffuse through a water filled membrane, it is noted in Fick’s Law, are determined by a combination of 2 gas laws: a. Henry’s Law – The amount of gas that dissolves into a liquid at a given temperature is proportional to the partial pressure of the gas 1. Solubility coefficient (of a liquid)– the amount of gas that can be dissolved by 1 ml of a given liquid at standard pressure (760 mmHg) and a specified temperature (37o is body temperature) 2. Gases can be categorized by its solubility coefficient 3. At normal barometric pressure (760 mmHg) and body temperature (37 degrees). The following is: The solubility of O2 is 0.0244 mL/mmHg/mLH2O The solubility of CO2 is 0.592 mL/mmHg/mLH2O On the basis of solubility coefficients of O2 and CO2 in a liquid medium, CO2 is more soluble than oxygen Solubility CO2 = 0.592 = 24 Solubility O2 = 0.0244 = 1 * We can see that CO2 is 24 times more able to dissolve than O2 b. Graham’s Law – The diffusion rate of a gas through a liquid is (1) directly proportional to the solubility coefficient of a gas and (2) inversely proportional to the square root of the gram-molecular weight (GMW) of the gas. GMW for O2 = 32 GMW for CO2 = 44 O2 diffuses faster than CO2 because of its lower GMW. It is a lighter gas. Diffusion rate for CO2 = √GMW O2 = √32 = 5.6 Diffusion rate for O2 = √GMW CO2 = √44 = 6.6 c. Diffusion Constant – a number assigned to a gas based on a combination of Henry’s Law and Graham’s Law 1. By combining the laws one can say that the rates of diffusion of two gases are directly proportional to the ratio of their solubility coefficient, and inversely proportional to the ratio of their GMW 2. In relation to O2 and CO2, CO2 dissolves 24x faster than O2, O2 is a less dense gas and will diffuse faster than CO2, ultimately CO2 diffuses through A-a membrane 19-20x faster than O2. Diffusion rate for CO2 = √GMW O2 X So. Coe. CO2 = 5.6 X 0.592 = 20 Diffusion rate for O2 = √GMW CO2 X So. Coe. O2 = 6.6 X .0244 = 1 V. PRESSURE GRADIENT a. Although based on the diffusion constant, CO2 has an advantage 20x faster than O2; O2/CO2 equilibration is completed in approximately 0.25 seconds even though the RBC is in the pulmonary capillary bed for 0.75 seconds. b. This occurs quickly because of the pressure gradient. c. In order for gas exchange to occur a difference in partial pressures must exist. In the normal lung alveolar (A) PO2 is approx 100 mmHg and the mean PCO2 is approx 40 mmHg. Venous blood returning to the lungs or PvO2 has a PO2 of approx 40 mmHg. Venous blood has a higher PCO2 than in the alveoli, the normal PvCO2 is 46 mmHg d. The pressure gradient for O2 is approximately 60 mmHg PAO2 – PvO2 = PO2 pressure gradient 100 mmHg – 40 mmHg = 60 mmHg e. The pressure gradient for CO2 is approximately 6 mmHg PvCO2 – PACO2 = PCO2 pressure gradient 46 mmHg – 40 mmHg = 6 mmHg f. The pressure gradient of O2 is now 10 x faster than that of CO2 which means that O2 diffusion happens as quickly as CO2 diffusion g. When a person has lungs damaged enough to effect surface tension, by increasing the gradient. h. When the damage is extensive where raising the gradient is ineffective it is considered refractory hypoxemia. VI. MEMBRANE THICKNESS a. The alveolar-capillary membrane is a mere 0.36 – 2.5 microns thick. b. O2 and CO2 molecules must pass through 7 separate layers for exchange. 1. Alveolar cell (membrane and intracellular water) 2. Basement layer below the Type I cell 3. Interstitial space – major determinate of the distance based on loose/tight space 4. Basement membrane of the capillary endothelium 5. Capillary endothelium 6. Blood plasma 7. RBC cell membrane and intracellular water c. As O2 molecules move out of the alveoli, it must travel through the layers to reach the hemoglobin molecule on the RBC. d. Thickening of the membrane or the space around it (i.e. – pulmonary fibrosis or edema) can increase the equilibration time. If the time were doubled 0.25 seconds to 0.5 seconds, there is still time for O2 equilibration because the RBCs remain in the capillary bed for 0.75 seconds. VII. OXYGEN CONTENT a. Once the oxygen has pass through the 7 layers of the membrane, the O2 molecules first fill up the plasma compartment of the blood (PaO2) b. For every mmHg unit of pressure, each 100 mL of blood can carry .003 mL of O2 dissolved in plasma c. If a person has a PaO2 of 100 mmHg the plasma carries 0.3 mL of O2 in 100 mL of blood. 100 mmHg X .003 mL of dissolved O2 = 0.3 vol % O2 d. Vol % represents the amount of O2 in mL in 100 mL of blood e. Vol % = ml O2/100 mL of blood, i.e. – if a person has 10 vol % of O2 mean there is 10 mL of O2 in 100 mL of blood f. If a person had a PaO2 of 50 mmHg would only have 0.15 vol % O2 in 100 mL of blood plasma g. h. i. j. When plasma is partially filled, the hemoglobin begins to fill. Each gram/dL of Hb carries 1.34 mL of O2 A person with 15 g/dL carries 19.5 mL of O2 SaO2 with a PaO2 of 100 mmHg, is usually 97% because of normal physiologic shunts Hb X Hb carrying capacity X SaO2 = O2 bound to Hb 15 g/dL X 1.34 mL X .97= 19.5 vol % O2 k. By combining the O2 carried in the plasma and O2 carried by the Hb of the RBC the result is O2 content or CaO2 l. Normal CaO2 is 19-20 vol % VIII. OXYGEN SATURATION a. The amount of O2 carried by the Hb is much higher than that of O2 carried in the blood plasma. b. Once an oxygen molecule has bound with hemoglobin, the affinity for Hb for more O2 molecules is increased. c. Hb tends to combine with four molecules or none, thus saturated or desaturated. Oxyhemoglobin is oxygenated hemoglobin. d. Oxygen saturation of arterial blood (SaO2): the percentage of hemoglobin that is carrying oxygen in arterial blood and is approximately 97%. Oxygen saturation of venous blood (SvO2) is normally approximately 75%. e. There are several factors that can effect the carrying ability of Hb: Partial Pressure of O2 Hydrogen ion concentration or pH Body temperature Organic phosphates Abnormal Hemoglobins IX. PARTIAL PRESSURE OF O2 a. There is a linear relationship between partial pressures and the amount of O2 dissolved in the blood. As PaO2 rises the O2 dissolved increases. The relationship PaO2 and SaO2 is direct, but not as linear. b. As O2 molecules leave the alveoli, plasma fills first, not the Hb, but as plasma fills and the PaO2 reaches 60 mmHg, the Hb fills faster. c. When PaO2 reaches 60, the SaO2 rises more quickly. d. The plasma still rises at the same rate of .003, but SaO2 will rise quickly at a PaO2 of 60 mmHg. e. Once the Hb is full, the rate of transfer plateaus. X. OXYGEN DISSOCIATION CURVE a. The effect of the relationship of the PaO2 and SaO2 can be visualized on the Oxygen Dissociation Curve b. If one were to plot this effect on a graph, with SaO2 on the vertical (y-axis) and PaO2 on the horizontal (x-axis) the plot will result in an “S” or sigmoid curve. c. The curve begins flat at the bottom, rises steeply in the middle, and then flattens again at the top. Image d. The clinical significance of the flattened portion at the top signifies that the hemoglobin is reaching it carrying capacity and can’t carry any more oxygen. Thus, going beyond approximately 100 mmHg adds very little to oxygen content in the blood. e. The clinical significance of the steep portion is that when the PaO2 falls below 60 mmHg, the quantity of O2 that reaches the tissue cells may be significantly reduced. Conversely, with small increases in the PaO2, the Hb releases large amounts of O2 as it moves through the capillaries and tissue cells. XI. The P50 a. A common point on the oxygen dissociation curve where the Hb is 50% saturated and is normally located at approximately PaO2 of 27 mmHg. b. There are situations where the curve will shift either to the right or left, thus effecting the P50 c. A shift to the right will signify that the affinity for oxygen is decreasing, causing the Hb to be less saturated at any given PaO2. A shift to the right means the P50 will increase. d. A shift to the left will show that the affinity for oxygen is increased; the Hb is more saturated at a given PaO2. As shift to the left means the will P50 decrease. XII. pH and THE BOHR EFFECT a. The presence of CO2 results in a rise in hydrogen (H+) ions, which decreases pH. b. The more CO2, the more H+ ions results in a lower pH and more acidic surroundings c. A decreased pH results in a physical change in the Hb molecule, which causes it to bind less strongly to O2 in an acidic environment. d. As the pH increases, the CO2 and H+ ions are decreasing and the Hb can bind better to the O2. e. The Bohr Effect is the ability of the pH to affect the affinity for oxygen by the hemoglobin. f. The result of the effect of pH on the Hb is that the hemoglobin will release O2 to the capillary beds and tissues that need the O2 (low pH and high CO2) and hold on to the O2 when there is an area that doesn’t need it (high pH and low CO2). g. The oxygen dissociation curve is also affected with the changes in pH. With more acid (acidosis) there is less Hb affinity for oxygen and a shift to the right. With less acid (alkalosis) there is more Hb affinity for oxygen and a shift to the left. h. The clinical significance of the Bohr effect can be seen in the following example: A patient has a pH of 7.40 a PaO2 of 70 mmHg and a saturation of 93% The pH drops to 7.20, the PaO2 remains the same, and saturation is now 88% i. In contrast, a patient who has a pH of 7.50 can have a saturation of 97-98%, which looks good, but the Hb does not release the O2 depriving the tissues of oxygen. XIII. BODY TEMPERATURE a. When body temperature changes it is directly related to metabolism. b. As temperature rises, cellular metabolism is increasing as well as the cell’s O2 requirement. The appropriate response for the blood is to release the O2 from the Hb to be delivered to the tissues. c. When body temperature decreases, the metabolism decreases the Hb does not have to release the oxygen as much. d. In a situation where there are cool temperatures and a low metabolic rate, the Hb will keep the O2, the tissues don’t require the O2, so a cold person with cyanotic hands will is not always in a serious condition. e. An increased body temperature, results in an increased metabolism, which in turn make less Hb affinity for oxygen, and a right shift in the oxygen dissociation curve. f. A decreased body temperature means a slower metabolism, more HB affinity for oxygen and a left shift in the oxygen dissociation curve. g. This website allows you to enter variables that temperature, pH, PCO2 have on the oxygen dissociation curve: VentWorld.com Oxygen Dissociation Curve XIV. ORGANIC PHOSPHATES (2,3-DPG) a. During cellular respiration, the anaerobic metabolism or glycolysis, creates some ATP or cellular energy but also creates a large amount of waste products: 1. Lactic Acid – decreases pH of the cell 2. 2,3 Diphosphoglycerate b. 2,3 DPG is found in RBCs where it forms a bond with the globin chains of deoxygenated Hb c. If a person is hypoxic, he will suffer from tissue hypoxia which increases the tissue levels of 2, 3 DPG. The Hb releases its oxygen to the hypoxic tissue d. If a person is Anemic, the CaO2 is decreased, anaerobic metabolism increases with tissue hypoxia, therefore there is increased levels of 2,3 DPG. Hb again releases its oxygen to hypoxic tissue e. In utero a fetus will have fetal Hb (HbF). Fetal Hb will shift the oxygen dissociation curve to the left increasing the Hb affinity for oxygen. 2,3 DPG counteracts the effect of fetal Hb in the newborn infant. f. Levels of 2,3 DPG in banked blood is decreases over time, and the blood is acidotic. Blood that is more than a few days old can impair oxygen delivery to the tissues because of levels of 2,3 DPG g. The presence of 2,3 DPG will result in a decreased Hb affinity for O2. With a large amount of 2,3 DPG there will be a right shift in the oxygen dissociation curve. XV. ABNORMAL HEMOGLOBINS a. Sickle Cell hemoglobin (Hb S): has less affinity for oxygen. Most danger is in its deoxygenated form, crystallizes in the erythrocyte causing the characteristic shape. Can lead to thrombus formation. b. Methemglobin (metHb): a condition in which iron atoms oxidize the hemoglobin into a ferric state which eliminate the ability for hemoglobin to carry oxygen. Can be seen in patients receiving iNO. c. Carboxyhemeglobin (HbCO): a toxic fume resulting from incomplete combustion of carbon or carbon-containing material; normal is <3% 1. A poisonous gas due to 2 properties Hb has an affinity for CO that is >200 times that of O2 CO creates an increased Hb affinity for O2, the O2 has a very strong bond with the Hb and the Hb does not release the O2 2. A person with CO poisoning can have an SpO2 of 100% only because the pulse oximeter reads molecules and can’t distinguish if it is O2 or CO 3. Treatment includes administration of 100% FiO2. If necessary hyperbaric chamber treatment with O2 is necessary. 4. By lowering the atmospheric pressure to 2-3 atmospheres, the PaO2 rises to great levels. By increasing the FiO2 in these conditions to 100%, the PaO2 would be 1746 mmHg. 5. With this PaO2 allows the plasma to carry 5.23 mL/dL and the tissue can receive the O2 it needs while the Hb is bound to the CO. XVI. HYPOXEMIA and HYPOXIA a. PaO2 in a normal, healthy adult is 80-100 mmHg b. When the PaO2 falls below normal limits, it is defined as hypoxemia. c. There are several reasons the PaO2 can fall below normal: 1. Low ambient PO2 2. Hypoventilation 3. Impaired diffusion 4. V/Q mismatches 5. Right-to-Left physiological shunting d. There are several levels of hypoxemia: 1. Normal: 80-100 mmHg 2. Mild: 60-79 mmHg 3. Moderate: 40-59 mmHg 4. Severe: <40 mmHg e. A person with COPD or is chronically hypercapnic will also be chronically hypoxemic. One must take caution when treating this type of patient with O2. f. Reponsive vs. Refractory hypoxemia 1. Responsive hypoxemia is hypoxemia that shows a significant response to and increase in FiO2. 2. It is usually a result of a V/Q mismatch. 3. A 20% increase in fiO2 results in a > 10 mmHg increase in the PaO2. 4. Refractory hypoxemia is hypoxemia demonstrating a nefligible increase in the PaO2 with the application of oxygen. 5. If the FiO2 is ≥ 50% and the PaO2 is < 60 mmHg. 6. If a 20% increase in FiO2 results in <10 mmHg increase in the PaO2. 7. This is a result of true shunting. g. Hypoxemia is a factor that leads to hypoxia h. Types of Hypoxia XVII. Formulas related to O2 transport