Supplementary Information (doc 127K)
advertisement

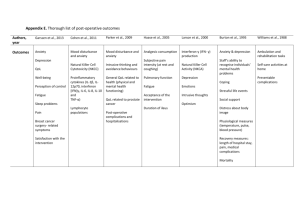
Supplementary online information (SI) at the website of Molecular Psychiatry Therapygenetics: The 5HTTLPR and Response to Psychological Therapy Correspondence: thalia.eley@kcl.ac.uk Online Supplementary Information contents Background Material and methods – participants, measures, genotyping, procedure Results Discussion, limitations and strength Acknowledgements Full reference list Supplementary figures and tables are in separate files: SupplementaryFigures.doc and SupplementaryTables.doc. 1 Background Candidate gene studies of anxiety, and related disorders such as depression, have provided substantial evidence of association with the Serotonin Transporter Promoter Polymorphism (5HTTLPR). The short (S) allele of the 5HTTLPR has been associated with reduced levels of 5HTT mRNA1, and was initially associated with a range of anxietyrelated traits2. This marker is, however, most consistently associated with depression in the context of stress3, 4, an example of gene-environment interaction. Of particular note, in studies of both depression5, 6, and anxiety7, not only has the short allele been associated with poorer outcome following stress, but also with better outcomes under low stress. This has led to the intriguing hypothesis that the marker reflects environmental plasticity8, and could thus predict enhanced response to psychological therapies9. We tested this hypothesis in a sample of children with anxiety disorders. Anxiety disorders are debilitating conditions that frequently emerge during childhood10, show strong continuity into adulthood11, are associated with a wide range of impairments and frequently precede other major psychiatric disorders, such as depression12. Given the adverse impact at both the individual and societal level, it is of critical importance to treat child anxiety disorders successfully and prevent development of other subsequent severe disorders. Cognitive-behavior therapy (CBT) is the most established treatment for child anxiety, with remission in approximately 55% of children post-treatment, and 65% by follow-up13. However, 35-45% of children remain significantly impaired following treatment. At present it is not possible to predict which children will benefit from CBT. This is clinically important, as predictive markers could be used to guide treatment and improve outcome. A number of factors have been reported to predict poor treatment response, three of which 2 could reflect genetic influence: increased symptom severity14, parental psychopathology1416 , and comorbidity with depressive disorders16, 17. However, in spite of the large literature supporting a role for specific genetic markers in predicting response to pharmacological treatment of psychiatric disorders15, the role of genetic markers has yet to be explored with respect to treatment using a purely psychological therapy. We tested this novel gene-environment interaction hypothesis in a sample of anxietydisordered children aged 6 to 13 years. Materials and methods Participants A total of 584 children aged 6-13 meeting DSM IV16 criteria for a primary diagnosis of an anxiety disorder were recruited (participation rate = 73%). The exclusion criteria were significant physical/intellectual impairment, psychoses, and concurrent treatment. Parental DNA was obtained where possible (maternal N = 521, paternal N = 425; complete trios N = 389). Recruitment was undertaken at two sites: Sydney, Australia and Reading, UK. The Australian sample was recruited from four groups treated by the Centre for Emotional Health at Macquarie University, Sydney: i) participants in a randomized trial of CBT for child anxiety disorders (N = 146)17, 18; ii) a parallel trial for children in rural Australia (N = 38)19; (iii) Prospective referrals to the clinic who met criteria after the trials ended (N = 143); and iv) archive participants (N = 96) from previous randomized trials. All participants completed the Cool Kids program, a CBT 10-12 session family and manual-based 3 treatment20. With the exception of the children from the rural trial, treatment was conducted in groups. Parents were involved in every session. The UK sample was recruited from two clinical trials at the Berkshire Child Anxiety Clinic (University of Reading) and a feasibility study within the Oxfordshire Primary Child and Adolescent Mental Health Service: (i) Participants from a clinical trial of child anxiety disorders, where the mother also had a current anxiety disorder (approximately 50% of cases, medication stable if used; N = 62); (ii) Remaining eligible children (no maternal anxiety disorders) who took part in a guided CBT self-help trial, (N = 76); (iii) Eligible participants from a funded feasibility study of guided CBT self-help (N = 23). Participants in the maternal anxiety trial completed an 8-session manual-based CBT treatment based on the Cool Kids program20 and a variety of adjunct sessions focused on maternal anxiety and mother-child interaction. The other two groups completed a 4-8 session guided CBT self-help treatment delivered via parents. This comprised the same primary components as the Cool Kids program and involved up to 4 in-person and 4 telephone sessions. Controls consisted of 459 white Europeans (177 men, 276 women, 6 sex unreported, mean age ± SD; 31.95 ± 12.62) recruited for the Bipolar Affected Case-Control study(24). All were screened for lifetime absence of psychiatric disorders using a modified version of the Past History Schedule21. Participants were excluded if they, or a first-degree relative, ever fulfilled criteria for major depression, bipolar disorder or schizophrenia, or they were ever treated for any psychiatric disorder including anxiety disorders. Measures 4 Child diagnosis Children were assessed using the Anxiety Disorders Interview Schedule for DSM-IV, Parent and Child Versions (ADIS-IV-C/P)22. Diagnoses and Clinical Severity Ratings (CSR; 0-8) were assigned by graduate or clinical psychologists based on composite parent/child report. Where the child met diagnostic criteria and received a CSR of 4 or more, diagnosis was assigned. Across both sites an experienced diagnostician trained the independent assessors using observation, feedback and supervision. To ensure a high level of consistency across sites, clearly specified guidelines for allocating diagnoses and CSRs were used. At the Macquarie site, trainees were required to observe and be observed by an experienced diagnostician, and were required to match the diagnoses of the experience diagnostician on at least 4 assessments. At Reading, assessors were trained using video-recorded assessments from Macquarie, and each assessor’s ratings were compared to ratings of a consensus group for the first twenty participants, to ensure high reliability (>.85) of diagnoses and CSRs. Once reliability requirements were met, assessors had to compare every sixth assessment with a consensus team in order to maintain high levels of reliability. Inter-rater reliability across diagnostic subtypes was excellent at both sites (>.80 for anxiety disorders, >.65 for mood disorders)18, 23. The percentages of children with specific disorders as their (a) primary diagnosis or (b) anywhere in their profile were as follows: Separation Anxiety Disorder (17.8%, 47.4%); Social Phobia (21.4%, 63.2%); Generalized Anxiety Disorder (45.1%, 80.2%) Specific Phobia (9.2%, 57.1%); Panic/Agoraphobia (0.8%, 3.1%); OCD (3.6%, 10.3%); PTSD 5 (0.3%, 0.6%) and Anxiety Disorders Not Otherwise Specified (1.7%, 1.9%). Mood disorders were present in 10.1% of the children (Depression: 3.4%; Dysthymia: 6.7%). Parental symptoms The parents completed the Depression, Anxiety and Stress Scale (DASS-21)24, a self-report measure of depression, anxiety and stress over the past week. It includes items such as “I tend to feel down-hearted and blue”, with a Likert scale response set ranging from “Does not apply to me at all”, to “Applies to me very much or most of the time”. Three scales consisting of 7 items each were created: stress, anxiety and depression, with scores ranging from a possible 0 to 42. The DASS-21 has good internal consistency and convergent validity25, 26. In this sample internal consistency for each scale was .85, .77 and .89 respectively. To identify parents significantly affected by depression, anxiety or general stress symptoms, we used the cut-offs for the “severe” category (scores greater than 21, 15, and 26 for depression, anxiety and stress respectively). Parents were classified as affected if they scored above the cut-off for any of the three scales. Mothers (fathers) reported 9.5% (11.4%), 10.3% (11.7%) and 11.7% (12.8%) depression, anxiety and stress respectively in the severe to extremely severe range. Descriptive statistics by site are given in Supplementary Table 1. The only significant differences were that the children from Sydney had higher primary disorder severity ratings at pre-treatment (p < .01), post-treatment (p = .01) and follow-up (p < .01). Descriptive statistics by trial are given in Supplementary Tables 2a (pre-treatment) and 2b (posttreatment and follow-up). Significant differences were observed for maternal psychopathology (p < .001). As expected, in the Reading Maternal Anxiety and Guided 6 Self-Help trials, maternal psychopathology was significantly higher and lower (respectively) than in any other groups. There were also significant differences between the trials for primary disorder severity ratings at pre-treatment (p < .001), post-treatment (p < .001) and follow-up (p < .001), % of primary anxiety responders at post-treatment (p = .05) and % of all anxiety responders at post-treatment (p < .01) and follow-up (p < .05). These differences reflect the greater severity ratings in the Sydney site as a whole both before and after treatment. Ethnicity Ethnicity was reported for the majority of children by asking about the ancestry of their grandparents, following which those with 4 grandparents of white European ancestry were included in the “white” sub-group (N = 359). Results were similar for the full sample (see Supplementary Tables 2, 5 and 7). Unfortunately, the numbers of subjects from other ethnic sub-groups were too small for a separate analysis (African or Caribbean, N = 1; Asian, N = 14; Arab and Middle Eastern, N = 8; Mixed, N = 39; Ancestry unknown and missing data, N = 163). Genotyping Genomic DNA was extracted from buccal swabs (for cases) and blood samples (for controls) using established procedures(31, 32). Genotyping of the 5-HTTLPR was performed by polymerase chain reaction TCCTCCGCTTTGGCGCCTCTTCC-3' (PCR) and using forward reverse primer primer 5'5'- TGGGGGTTGCAGGGGAGATCCTG-3' (Sigma-Aldrich, Dorset, UK). The PCR reaction was performed in a final volume of 20 µl containing 30 ng of genomic template, 0.2 µM each primer, 200 µM each dNTP and 0.25 U of HotStar Taq Polymerase with 1.5 mM 7 MgCl2 and 1 X Buffer (QIAGEN, Crawley, UK). PCR cycles consisted of an initial 15 min denaturation step at 95 °C followed by 35 PCR cycles of 94°C for 30 s, 65.5°C for 90 s and 72°C for 60 s with a final extension step of 10 min at 72°C. The amplified products (S-469 bp, L-512 bp) were separated by electrophoresis on a 3.5% agarose gel and stained with ethidium bromide. The genotyping success rate was 96.2 %. Genotype distribution for white subset (whole sample) was as follows; LL: 34.3% (32.2%); LS: 48.5% (47.9%); SS: 17.3% (19.9%) conformed to the Hardy-Weinberg Equilibrium (21 = 0.001, p = .97 and 21 = 0.40, p = .53 for the white subsample and whole sample respectively). Procedure. Ethical procedures were approved by Human Ethics and Biosafety Committees at both sites. Parents provided informed consent, children provided assent. Buccal swabs were collected either at the clinic or through the post. Families provided data at pre, post (N = 523; 89.6%) and one follow-up point (N = 427; 73.1%). The timing of the follow-up differed across trials (3-, 6-, and 12 months) and for these the N (percentage) were as follows: 52 (8.9%), 348 (59.6%), and 27 (4.6%) respectively. Within the white subsample, post-treatment data were available on 326 children (90.8%) with data from 40 (11.1%), 210 (58.5%) and 20 (5.6%) available at 3, 6 and 12 month follow-up points respectively (total follow-up = 75.2%). For the Sydney subset, post-treatment data were available on 240 children (93.0%) with data from 40 (15.5%), 155 (60.0%) and 20 (7.75%) available at 3, 6 and 12 month follow-up points (Total follow-up N = 215; 83.3%). For the Reading subset, post-treatment data were available on 86 children (85.5%), and follow-up data (only collected at 6 months) were available from 55 children (54.5%). The total amount of follow-up data available from each site differed significantly (21 = 32.47, p < .001), and significant differences were observed between 8 those with and without follow-up data. Those without follow-up data were significantly older (9.96 years vs. 9.27 years, p =.002), had less severe ratings for their primary disorder at pre-treatment (6.01 vs. 6.23, p =.05) but had a greater frequency of comorbid mood disorders (18.0% vs. 7.4%, p = .004). Note that at the Reading site trials are ongoing, and levels of follow-up data reflect the cut-off in time taken for this paper. Results To test the association between 5HTTLPR and anxiety disorders, we first cross-tabulated genotypic frequencies for our white cases (N = 359) and a white European sample of never-psychiatrically ill controls (N = 459)24. There were no significant differences using either a genotypic (contrasting SS, SL and LL; 22 = 0.40, p = .82) or recessive (SS versus SL/LL; 21 = 0.04, p = .85) model. A within-family analysis using a transmissiondisequilibrium test (TDT) on the white trios (child, mother and father; N = 267), was also non-significant (22 = 0.10, p = .75). We classified treatment response initially as the absence of the primary anxiety disorder (“primary anxiety response”). In order to explore whether treatment response extended beyond the primary diagnosis, we also considered the absence of any anxiety diagnosis (“all anxiety response”). Outcome was assessed at two time-points: immediately posttreatment and at follow-up, usually 6-months after the end of treatment, with a proportion assessed at 3- and 12-months post-treatment. Note that although we conduct multiple analyses, as these all test the same hypothesis, albeit in slightly different ways, we did not correct for multiple testing. The analyses proceeded in two steps. First we cross-tabulated 9 treatment response in the three genotype groups, at post-treatment and follow-up. There were significant associations between 5HTTLPR and both “primary” and “all” anxiety response at follow-up (see Figure 1 and Supplementary Table 3) but not post-treatment (see Supplementary Figure 1 and Supplementary Table 3). The association with treatment response at follow-up was significant in both genotypic and recessive models, but favourable treatment response in the SS group drove the association, indicating a recessive model. Positive response at follow-up was seen in 20.0% and 18.8% more children with the SS than the SL/LL genotype for “primary” (78.4% vs. 58.4%, p < .01) and “all” (60.8% vs. 42.0%, p < .02) anxiety response respectively. When the analyses were repeated for the entire sample (i.e. not just the white sub-set) very similar patterns of effects were shown (See Supplementary Table 3a). Furthermore, similar results were seen in the Sydney and Reading subsets individually, although these failed to reach significance in the small Reading sample (N = 55; see Supplementary Table 3b). Next, to provide unbiased estimates in the presence of missing data, and to control for covariates, we used multiple logistic regressions with robust standard errors and fullinformation maximum likelihood estimation. The model included 5HTTLPR genotype (SS coded as 1, SL/LL as 0), time (linear and quadratic effects to take into account the use of 3 follow-up time-points), age, gender and treatment site (Sydney or Reading; see Supplementary Table 4). For both outcome measures at follow-up, only 5HTTLPR was a significant predictor (See Supplementary Table 5, model 2, for post-treatment results). The low odds ratios (OR; e.g. 0.39 [95% CI: .18 - .81], p = .01 for “primary” anxiety response) indicate that SS genotype children were almost 3 times less likely to have their primary anxiety disorder at follow-up, i.e. they had a better response than the rest of the sample. Importantly, in a model that controlled for other significant influences on treatment 10 response (mood disorders, pre-treatment symptom severity and maternal psychopathology), the odds ratio for 5HTTLPR remained undiminished (for primary anxiety response, OR = .39, [.18 - .87], p = .02; see also Supplementary Table 5 model 3 for “all” anxiety response). Of note, the odds ratio for 5HTTLPR was very similar when analyses were repeated for (a) the full sample; (b) just those with 6-month follow-up only; and (c) just those who received at least 8 in-person CBT sessions (see Supplementary Table 5 models 4-6). Furthermore, the Odds Ratios were similar for the Sydney and Reading subsets, though again not reaching significance for the Reading subset. Finally, we examined whether these results were specific to the presence/absence of disorder per se, or whether they generalized to improvement in symptom severity across diagnostic boundaries. We conducted multiple linear regressions with robust standard errors using change in severity ratings of the primary diagnosis from pre-treatment to follow-up. The 5HTTLPR significantly predicted change in severity ratings to follow-up but not to post-treatment (see Supplementary Figure 2 and Supplementary Table 6 models 1 and 2). The standardized beta coefficient for the follow-up analyses ( = -.15, p < .01) indicates that SS children had, on average, a .15 standard deviation greater reduction in severity scores than SL/LL children. The beta coefficient for 5HTTLPR remained significant ( = -.17, p < .01) even after controlling for other significant clinical covariates (pre-treatment symptom severity and maternal psychopathology; see Supplementary Table 7 model 3). The 5HTTLPR also significantly predicted change scores to follow up in (a) the full sample; (b) just those with 6-month follow-up only; and (c) just those who received at least 8 in-person CBT sessions (see Supplementary Table 7 models 4-6). Furthermore, as with the categorical analyses, the results were similar for both Sydney 11 and Reading subsets, though weaker and non-significant in the latter (Supplementary Table 7). In contrast to the pharmacogenetics literature25, no study to date has explored the role of a genetic marker in relation to response to a purely psychological treatment for a psychiatric disorder. Previous studies have comprised small samples and have not considered pure psychological treatment groups. Specifically, one previous pilot study (N = 69) revealed a significant influence of the COMTval158met polymorphism on response to exposurebased CBT in adult panic disorder, but in that sample almost 50% of subjects were also medicated27. A naturalistic study found that those with the S form of the 5HTTLPR were less likely to respond to treatment, be it CBT, medication or both26. Here we present evidence that in children with anxiety disorders, those with the 5HTTLPR SS genotype were 20% more likely to respond to a purely psychological treatment (CBT). Furthermore, children with the SS genotype showed significantly greater reduction in their clinical symptom severity ratings than those with SL/LL genotypes. These contradictory findings are likely to reflect not only small sample sizes and varying phenotypes, but also the role of medication (see below). This study has some limitations that need to be considered when interpreting the findings. The first is that whilst the sample size is large in terms of treatment trials in child anxiety, it is small for a genetic study. Furthermore, although these findings hold true both in the white subset and the entire sample, there is no independent replication so they must therefore be considered preliminary. Replication will be crucial, and we are currently working towards obtaining a replication sample. Second, we only had parent-reported depression, anxiety and stress symptoms pre-treatment and not at follow-up, when our 12 main findings were seen. It would be interesting to see if parental data at follow-up influenced the association between genotype and treatment response. Finally, while the effects of the SS genotype at follow-up were robust to the inclusion of potential confounders, no significant effects were evident immediately post-treatment. The period between post-treatment and follow-up is typically characterised by continued improvement as the child continues to apply the skills learnt13, thus it is possible that the genotype influences capacity for continued benefit from the intervention. This may be mediated by changes in anxiety-relevant cognitions which, whilst being moderately heritable27, appear to change largely as a result of environmental influences28. It is plausible that children with the SS genotype have subtle differences in their cognitive processing that make them not only susceptible to anxiety-related symptoms in the presence of stress, but also more capable of change in response to a supportive environment such as CBT. These findings are important both clinically and conceptually. First, our data suggest that knowledge of genetic markers can be used to inform treatment choices with respect to psychotherapeutic as well pharmacological interventions. We term this approach therapygenetics. If replicated, these findings could potentially be useful to clinicians treating anxious children. Thus, there may come a time when children with the SL or LL genotypes are offered enhanced treatments in order to maximise the chance of them improving. Of note, in adult depression, response to SSRIs is better in LL subjects25, revealing an interesting potential double dissociation between this genotype and response to different types of treatment. Second, the possibility that the 5HTTLPR, in particular, may tag a subtype of disorder that is more responsive to psychological treatment 9, is in keeping with the hypothesis that this marker reflects environmental sensitivity8. Psychological treatment is just one positive environmental influence currently being considered in the 13 context of this hypothesis, and it will be interesting to see if other positive environments also interact with the SS genotype resulting in beneficial outcomes. In conclusion, we have shown that the 5HTTLPR SS genotype is associated with a significantly increased likelihood of positive response to CBT. If replicated, these results may provide a tool which could help decide whether an individual is likely to benefit from standard CBT alone or whether enhanced treatment is required. 14 Acknowledgements: Supported by the Australian Research Council (DP0666048), Australian National Health and Medical Research Council (PG382008 and PG488505), UK Medical Research Council (MRC; GU601020, G0802326, G0901874, and G120/635) and by the UK National Institute for Health Research (PBPG019712042). Creswell supported by MRC Fellowship G0601874, Uher supported by the European Commission (115008). The authors have no financial interests to disclose 15 References 1. Heils A, Teufel A, Petri S, Stober G, Riederer P, Bengel D et al. Allelic variation of human serotonin transporter gene expression. J Neurochem 1996; 66: 2621-2624. 2. Lesch KP, Bengel D, Heils A, Zhang Sabol S, Greenburg BD, Petri S et al. Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science 1996; 274: 1527-1531. 3. Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H et al. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science 2003; 301: 386-389. 4. Karg K, Burmeister M, Shedden K, Sen S. The Serotonin Transporter Promoter Variant (5HTTLPR), Stress, and Depression Meta-analysis Revisited: Evidence of Genetic Moderation. Arch Gen Psychiatry 2010 January 3, 2011. 5. Eley TC, Sugden K, Gregory AM, Sterne A, Plomin R, Craig IW. Gene-environment interaction analysis of serotonin system markers with adolescent depression. Mol Psychiatry 2004; 9: 908-915. 6. Taylor SE, Way BM, Welch WT, Hilmert CJ, Lehman BJ, Eisenberger NI. Early family environment, current adversity, the serotonin transporter promoter polymorphism, and depressive symptomatology. Biol Psychiatry 2006; 60: 671-676. 16 7. Stein MB, Schork NJ, Gelernter J, Stein MB, Schork NJ, Gelernter J. Gene-by-environment (serotonin transporter and childhood maltreatment) interaction for anxiety sensitivity, an intermediate phenotype for anxiety disorders. Neuropsychopharmacology 2008; 33: 312319. 8. Belsky J, Jonassaint C, Pluess M, Stanton M, Brummett B, Williams R. Vulnerability genes or plasticity genes? Mol Psychiatry 2009; 14: 746-754. 9. Uher R. The implications of gene-environment interactions in depression: will cause inform cure? Mol Psychiatry 2008; 13: 1070-1078. 10. Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui LH et al. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 2010; 49: 980-989. 11. Bittner A, Egger HL, Erkanli A, Costello EJ, Foley DL, Angold A. What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry 2007; 48: 11741183. 12. Cole DA, Peeke LG, Martin JM, Truglio R, Seroczynski AD. A longitudinal look at the relation between depression and anxiety in children and adolescents. J Consult Clin Psychol 1998; 66: 451-460. 17 13. James A, Soler A, Weatherall R. Cochrane review: Cognitive behavioural therapy for anxiety disorders in children and adolescents. John Wiley & Sons, Ltd., 2007, pp 12481275. 14. Hudson JL. Efficacy of Cognitive-Behavioural Therapy for Children and Adolescents With Anxiety Disorders. Behaviour Change 2005; 22: 55-70. 15. Serretti A, Kato M, De Ronchi D, Kinoshita T. Meta-analysis of serotonin transporter gene promoter polymorphism (5-HTTLPR) association with selective serotonin reuptake inhibitor efficacy in depressed patients. Mol Psychiatry 2007; 12: 247-257. 16. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. American Psychiatric Association: Washington, DC, 1994. 17. Rapee RM, Abbott MJ, Lyneham HJ. Bibliotherapy for children with anxiety disorders using written materials for parents: A randomized controlled trial. J Consult Clin Psychol 2006; 74: 436-444. 18. Hudson JL, Rapee RM, Deveney C, Schniering CA, Lyneham HJ, Bovopoulos N. Cognitive-Behavioral Treatment Versus an Active Control for Children and Adolescents With Anxiety Disorders: A Randomized Trial. J Am Acad Child Adolesc Psychiatry 2009; 48: 533-544. 19. Lyneham HJ, Rapee RM. Evaluation of therapist-supported parent-implemented CBT for anxiety disorders in rural children. Behav Res Ther 2006; 44: 1287-1300. 18 20. Lyneham HJ, Abbott MJ, Wignall A, Rapee RM. The Cool Kids Anxiety Treatment Programme. MUARU, Macquarie University: Sydney 2003. 21. McGuffin P, Katz R, Aldrich J. Past and Present State Examination: the assessment of 'lifetime ever' psychopathology. Psychol Med 1986; 16: 461-465. 22. Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for Children-IV (Child and Parent Versions). Oxford University Press: New York 1996. 23. Lyneham HJ, Abbott MJ, Rapee RM. Interrater reliability of the anxiety disorders interview schedule for DSM-IV: Child and parent version. J Am Acad Child Adolesc Psychiatry 2007; 46: 731-736. 24. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 1995; 33: 335-343. 25. Keers R, Aitchison KJ. Pharmacogenetics of antidepressant response. Expert Review of Neurotherapeutics 2011; 11: 101-125. 26. Steiger H, Joober R, Gauvin L, Bruce KR, Richardson J, Israel M et al. Serotonin-System Polymorphisms (5-HTTLPR and-1438G/A) and Responses of Patients With Bulimic Syndromes to Multimodal Treatments. J Clin Psychiatr 2008; 69: 1565-1571. 19 27. Eley TC, Gregory AM, Clark DM, Ehlers A. Feeling anxious: A twin study of panic/somatic symptoms, anxiety sensitivity and heart-beat perception in children. Journal of Child Psychology and Psychiatry 2007; 48: 1184-1191. 28. Zavos HMS, Rijsdijk FV, Eley TC. Longitudinal associations between Anxiety Sensitivity, Anxiety and Depression. Submitted for publication. 20