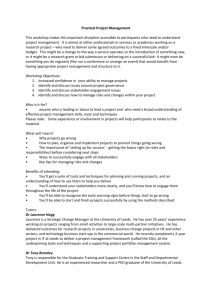
Academic Clinical Associate Professor in Health Economics
advertisement

C Faculty of Medicine and Health School of Medicine Leeds Institute of Health Sciences Academic Unit of Health Economics Academic Clinical Associate Professor in Health Economics (Decision Analysis and Simulation Modelling) and Honorary Consultant in Medical Oncology We have introduced the title of Clinical Associate Professor for our grade 9 academic staff, which is equivalent to Clinical Senior Lecturer. This is a new position that has been created with funding from the Leeds Institute of Health Sciences and Leeds Teaching Hospitals NHS Trust. An opportunity has arisen to appoint a senior academic and consultant in medical oncology to lead on decision analysis and simulation modelling in the context of the early evaluation of personalised medicines, diagnostic tests and medical devices with a focus on breast cancer. The University of Leeds is at the forefront of UK applied research in this area will provide a strong platform upon which to take forward a related personal research methodology programme. The applicant will reside within the Academic Unit of Health Economics but will work closely with researchers in Health Informatics, Biostatistics, Clinical Trials Research, Clinical Biochemistry, Proteomics, Genomics and Transport Studies. The applicant will be expected to bring new ideas in the methods for technology appraisal centred on modelling early in the evaluation programme. We are particularly interested in the use of decision modelling for research prioritisation and design, simulation of healthcare pathways and the use of real-time clinical and financial data linkage to improve the performance of such models. The position will include opportunities to work with the recently awarded Leeds NIHR Diagnostics Evidence Co-operative (http://www.nihr.ac.uk/infrastructure/Pages/DECs.aspx) for which we have adopted a philosophy of decision modelling early in the development pathway for in-vitro diagnostics. The clinical themes for this will include renal diseases, liver diseases, musculoskeletal diseases and cancer (with a focus on breast cancer). Similar opportunities exist in collaboration with the Leeds-based Health Technology Co-operative for Colorectal Therapies whose themes include engineering, nanotechnology, bio-sensing (http://www.nihr.ac.uk/infrastructure/Pages/HTCs.aspx). It will also be possible to work on projects with the Medical Technologies Innovation and Knowledge Centre (http://www.medical-technologies.co.uk/) and the University of Leeds Stratified Medicine Hub (http://www.leeds.ac.uk/info/125114/stratified_medicine). International collaboration will be an essential component of the position and will include working with a multi-million dollar research programme funded by Genome Canada looking at research methods for personalised medicine. The applicant will be expected to promote the further development of our portfolio of technology appraisal, model-based economic evaluation and big-data linkage in cancer genomics, point of care testing and companion diagnostics in collaboration with commercial and academic partners. A grade 7 researcher will support the successful applicant. You must have a strong track record in the quantitative and computational methods needed for decision modelling including competence with relevant software or programming tools. A suitable background might include economics, business, operations research, informatics, decision science or applied programming. Experience in health economics is desirable but not essential if you can bring alternative valuable skills to the position. You should have proven skills in academic leadership and be able to provide evidence of previous successful inter-disciplinary collaboration. You should also have an established record of successful clinical research in oncology and a significant record of administrative and teaching skills. You will be expected to work with clinical academics in Leeds Institute of Cancer and Pathology (LICAP) and NHS colleagues to develop and support clinical research, especially in breast cancer. You will undertake clinical activities (3PAs) in the medical oncology practice as part of an established team of medical and clinical oncologists within Leeds Teaching Hospitals Trust (LTHT), supported by junior staff and specialist nurses, and join a 1 in 18 out-of-hours acute oncology on call rota [arrangements subject to change.]. Candidates will be expected to have a postgraduate degree, hold the MRCP (or equivalent) and be included on the GMC’s Specialist Register for Medical Oncology (or be within six months of being admitted to the Register for trainees if currently in a training programme in the UK). You must have research experience that can be the basis to become internationally excellent and an ability to manage and initiate health economics and clinical cancer research. Salary will be on the clinical scale for the New Consultant Contract £75,249 - £101,451 p.a. The University of Leeds is committed to providing equal opportunities for all and offers a range of family friendly policies (http://hr.leeds.ac.uk/homepage/4/policies). The University is a charter member of Athena SWAN and holds the Bronze award. The School of Medicine gained the Bronze award in 2013. We are committed to being an inclusive medical school that values all staff, and we are happy to consider job share applications and requests for flexible working arrangements from our employees. Informal enquiries regarding the post should be directed to Professor Claire Hulme + 44 (0)113 343 0875, c.t.hulme@leeds.ac.uk or David Meads +44 (0)113 343 0860, d.meads@leeds.ac.uk (Leeds Institute of Health Sciences), Professor Chris Twelves +44 (0)113 2076 7469, c.j.twelves@leeds.ac.uk (Leeds Institute of Cancer and Pathology), or Dr David Jackson + 44(0)113 2067965, davidp.jackson@nhs.net (Leeds Teaching Hospitals Trust). If you have any specific enquiries about your online application please contact Mrs Sue Davis + 44 (0)113 343 0831, s.davis@leeds.ac.uk Job Ref: MHIHS1013 Closing Date: 18 December 2014 Purpose of the post This post is based in the Leeds Institute of Health Sciences with links to the Leeds Institute of Cancer and Pathology and Leeds Teaching Hospitals NHS Trust. This post will develop and lead ongoing programmes of decision analysis and simulation modelling in health economics research linked to existing and new programmes of activity with a focus on cancer; within Leeds Teaching Hospitals Trust the post-holder will deliver clinical service and clinical research of the highest quality and impact. You should be a member of the Royal College of Physicians and hold the MRCP or equivalent and be included on the GMC’s Specialist Register for Medical Oncology (or be within six months of being admitted to the Register for trainees if currently in a training programme in the UK). Main purpose of the job: To draw on extensive academic excellence to underpin and carry out research, teaching, leadership and management, in the field of Health Economics and within the School and Faculty. You will be expected to provide leadership in research and contribute to management/ administration as indicated below, with approximate breakdown of duties being 30% clinical and 70% research and teaching (including postgraduate students): The post-holder will be an Honorary Consultant (3PAs) in Medical Oncology based at St James’s University Hospital for clinical practice and clinically based research and work as part of an established breast oncology team. Main duties and responsibilities: General: To contribute to the development and achievement of University, Faculty and School strategy within the context of an international, research-led university Adhere to University values and standards, including the Leadership and Management Standard, and in line with University policies and procedures and local Faculty/School benchmarks as appropriate, upholding high professional standards and leading by example To be aware of and work in line with the University’s learning and teaching partnership agreement and work with our students as members of a learning community to provide world class education and an excellent student experience To maintain own continuing professional development To maintain a safe and healthy work environment, including ensuring compliance with health and safety legislation and the undertaking of appropriate risk assessments To integrate the University value of inclusiveness into all appropriate aspects of the job; respecting the dignity and diversity of all members of the University community and of visitors to the University Research, Innovation and Impact: To be recognised as an authority in the field, developing and maintaining an external profile as appropriate to the discipline To develop and lead health economics methods research in an area of established expertise To support the development of high quality applied health research with colleagues at the University of Leeds and elsewhere. To integrate advanced, and where appropriate novel, modelling methods in health economics To promote integration of health economics research with other research interests within LIHS as well as across the Faculty of Medicine and Health. To maintain a high quality record of regular and original research publications of external standing as appropriate to the discipline To attract research income on an individual and collaborative basis, as appropriate to the discipline, to underpin high quality research activity To provide high quality postgraduate supervision and attract research students to the university To establish and maintain a programme of high quality clinical breast cancer clinical research To take part in knowledge transfer activities, where appropriate and feasible Teaching: To undertake research-led teaching at different levels on undergraduate and/or postgraduate taught courses, regularly collecting, and responding to, student feedback To contribute at an appropriate level to School and Faculty policy and practice in teaching To play a significant role in the design, development and planning of modules and programmes within the subject area as required To play a significant role in the review of modules and programmes and in quality assurance and enhancement as required To develop innovative approaches to learning and teaching as appropriate To provide timely feedback and assessment of coursework and examinations To provide general support and guidance to students, resolving issues and/or referring to specialist parties, where appropriate To act as a personal tutor, supporting involvement in Leeds for Life To provide academic leadership through: Significant contribution to the overall work of the University and/or equivalent external organisations by representing the School and Faculty on appropriate committees and groups Effective contribution to the management and administrative processes and committee structures of the school, faculty and university Managing or leading major initiatives or areas of work (as either sustained or one-off projects) which facilitate School, Faculty or University performance or business as required Involvement in the recruitment, management and development of staff and act as a mentor to more junior/less experienced colleagues The promotion of the values of collegiality within the academic community Actively promoting and engaging with the objectives of our valuing and developing all our staff agenda via compliance with the University’s People Management Framework to ensure high standards of employment practices across the School. Clinical Programmed Activities: : An Honorary Consultant appointment with the Leeds Teaching Hospitals NHS Trust will be available for the successful candidate (3 PAs), based at St James’s University Hospital. Activities will include ward attending, out-patient clinics and multi-disciplinary team meetings for the breast oncology clinical services as appropriate, along with departmental audit, governance and continuing professional development; an indicative job plan is shown below. You will undertake clinical research to facilitate the development of a personal clinical research programme, with the support of established research teams. You will also undertake teaching duties in keeping with those of a Clinical Associate Professor/honorary teaching hospital consultant physician. The post will be subject to joint job planning and appraisal by the University and NHS. The Department is within the Institute of Oncology Clinical Services Unit (Clinical Director David Jackson), St James’s University Hospital. Details of the Consultant team are provided in appendix 1. This job description provides a framework for the role and it may be necessary for an Associate Professor to undertake any duties commensurate with the post as might reasonably be required Relationships You will be located in an Academic Unit of Health Economics and will be responsible to the Head of the Unit and accountable to the Institute Director and ultimately to the Dean of Medicine and Health. You will be expected to work with other research and teaching team members in addition to developing your specific research activities. You will also have key professional relationships with the Head of the Section of Oncology and Cancer Research (Professor Chris Twelves), and through him with the Divisional Director for the Institute of Cancer and Pathology (Professor Tim Bishop). There will be close clinical links with medical oncology, clinical oncology and other staff; clinical line management will be through the Lead Clinician for Medical Oncology (Dr Dan Swinson) to the Clinical Director for Oncology (Dr David Jackson) at Leeds Teaching Hospitals NHS Trust. University Values All staff are expected to operate in line with the University’s values and standards, which work as an integral part of our strategy and set out the principles of how we work together. More information about the university’s strategy and values is available at http://www.leeds.ac.uk/comms/strategy/ Essential Candidates will be expected to demonstrate appropriate levels of experience and skill to enable them to achieve the requirements of the job description. The following skills and abilities are essential in this context: Membership of the Royal College of Physicians (UK) or equivalent Must have completed a recognised training programme in medical oncology and be on the GMC specialist register in medical oncology Able to demonstrate a high level of clinical experience and competence in breast cancer PhD or equivalent experience in a relevant discipline A proven strong academic track record in modelling and/or the methods of efficient research and development in health care A coherent five-year research plan A track-record of academic leadership of health economics or statistical research A track-record of high quality peer-reviewed journal publications A track-record of multi-disciplinary collaboration with researchers A proven ability to attract research funding Effective interpersonal and organisational skills with the ability to prioritise work and maintain a high level of accuracy Effective communication, facilitation and presentation skills Experience of training undergraduate medical students and postgraduate doctors supervising postgraduate research students Excellent team player as well as to work independently within a programme of research Experience of facilitating the career development of less experienced colleagues in research, teaching and administration Computer literate; conversant with a range of software (e.g. Excel) Strong problem solving and negotiation skills Evidence of an enthusiastic and co-operative attitude Willingness to undertake appropriate training and administration Ability to lead, motivate and inspire others Effective communication and organisation skills Ability to work as part of a team and co-operate with others Commitment to own continuing professional development Aptitude for and attainment in teaching and learning An ability to forge links across disciplines Ability to initiate and manage and initiate clinical research independently and experience of developing clinical trial protocols. Experience of contributions to clinical research, for example through obtaining informed consent and data collection for patients in clinical trials Have an understanding of current NHS management and Trusts and be aware of the responsibilities that a consultant post brings Desirable A track-record strategic leadership of health economics or statistical research Experience using specific software (e.g. Treeage, STATA, Simul8) Skills in effective academic and strategic leadership within an established research group Experience of facilitating the career development of less experienced colleagues in research, teaching and administration An ability to think laterally, to be imaginative, and to anticipate trends and opportunities A recognised teaching qualification e.g. ULTA 2 or equivalent Experience of teaching all levels of HE students using different mechanisms stimulate development and learning Experience of course design and development of research led teaching Ability to provide leadership in the planning and development of modules, programmes, and short-courses within the fields of health economics Honorary Consultant Contract You will be awarded an honorary NHS contract with the Leeds Teaching Hospitals NHS Trust. Job plan and Working arrangements The job plan will incorporate clinical PAs and academic PAs. A sample job plan is outlined below but the precise details will be dependent on the interests and expertise of the successful candidate. The job plan will incorporate 7 academic (research and teaching) and 3 clinical (approximately 2 DCC, 1 SPA) and 2 additional academic PA will also be available.. A job plan review will take place annually, normally with the Trust Clinical Director or Clinical Management Team and University Academic Lead or Divisional Director. The annual job plan review may result in a revised prospective job plan. There may be an interim review of the job plan where duties, responsibilities, accountability arrangements or objectives have changed or need to change significantly within the area. The post is subject to clinical governance arrangements through the NHS Trust and a rolling programme of Audit is conducted, with support. Please note that this is an indicative job plan. The exact details of the sessional timetable will be negotiated with the successful candidate. The duties of the post may be changed with the agreement of the post holder and funding bodies. You will join a 1 in 18 out-of-hours acute on call rota in medical oncology; you will share responsibility for out-of-hours ward cover and acute oncology admissions on the same rota. Joint Appraisals In line with the Follett Report recommendations, the University of Leeds has been working closely with the local NHS Trusts in implementing joint appraisals. You will be expected to participate in a joint appraisal arrangement as agreed locally on an annual basis. The ‘joint appraisal’ will be conducted by two appraisers, one from the University and one from the NHS, working together with one appraisee on a single occasion. There will be annual job planning meetings. Indicative Job Plan Day Monday Time 09.00 to 13.00 Location Work St Clinic James’s Categorisation Trust: Direct Clinical Care No. of PAs 0.83 PA 14.00 to 18.00 9.00 to 13.00 LIHS Research 1 PA St James’s MDT/ Ward Round 1:3 University Academic Trust: Direct Clinical Care LIHS Research 2:3 Research University Academic University Academic University Academic Trust: SPA 0.66 PA University: Academic University Academic University: Academic 1 PA University: Academic 0.75 PA Tuesday Wednesday Thursday Friday 14.00 to 17.30 09.00 to 13.00 14.00 to 18 .00 LIHS 9.00 to 13.00 14.00 to 17.00 9.00 to 13.00 St James’s LIHS DEC Research Audit and clinical / research / governance meetings DEC Research Research LIHS Research 14.00 to 17.00 LIHS Research St James’s St James’s 1 PA 1.0 SPA 0.75 PA 1 PA None Sunday TOTAL PAs 0.87 PA None Saturday Additional agreed activity to be worked flexibly Predictable emergency on-call work Unpredictabl e emergency on-call work 0.34 PA Clinical admin Trust: Direct Clinical Care 0.33 PA Trust: Direct Clinical Care 0.5 PA As agreed Trust: University: Overall 3 PAs 7 PAs 10 PAs Resources available to support you: Staff – details are provided on the appendices attached Outpatient clinics – in Leeds, the oncology clinic areas will be available to the Consultant Inpatient facilities – inpatient facilities will be provided within the bed-base of non-surgical oncology in the Institute of Oncology Research programme and criteria – you will be encouraged to facilitate and contribute to the current clinical research programs on-going in the department A shared office with IT facilities (PC, email etc) will be provided on the St James’s campus with access to administrative assistance Shared clinical and academic secretarial support Leave Arrangements All leave will be in accordance with Trust leave policy according to the new consultant contract and will including long service awards accrued. Leave should be applied for in accordance with the Trust’s Leave Policy, normally giving six weeks’ notice of any leave, other than in exceptional circumstances. Training During the course of your employment, you agree to undergo whatever training the Trust deems necessary. This may include, but is not limited to, induction training, professional development and safe working practices. Funding of such training will be in accordance with the Trust’s Staff Development Policy. Continuing Medical Education The Trust fully supports the requirement for CME by the relevant Royal College and acknowledges that it is an essential component of a consultant’s professional activities that will be reviewed during the appraisal process and revalidation. Time and financial support for these activities will be granted in accordance with the Trust’s Leave Policy. Further information Faculty Information With more than 6,000 students, 1,600 staff and annual research income of £50m, the Faculty of Medicine and Health at Leeds is bigger than some universities. Leeds has one of the largest medical and bioscience research bases in the UK, and is an acknowledged world leader in cancer, cardiovascular, psychiatric, genetic, musculo-skeletal and health services research. Treatments developed in Leeds are transforming the lives of people around the world living with conditions such as HIV, TB, diabetes and malaria. The School of Medicine The School of Medicine at the University of Leeds is a major international centre for research and education. Our ambition is to improve health and reduce health inequalities, locally and globally, through excellent scientific research and the translation of that research into healthcare practice, and through the education of future scientific and clinical leaders who will advocate and practise an evidence-based approach. Our major strategic aims are to: Deliver outstanding research including basic discovery science through to applied health research that makes a significant difference to health. Produce exceptional graduates, clinicians, educators, doctoral and post-doctoral fellows whose learning has been informed and inspired by our research excellence and who will form the next generation of academic and clinical leaders. Develop and support knowledge transfer activities that flow from our academic activities. Create and maintain an efficient and sustainable environment for research and teaching within an organisational culture and management style that enacts and supports the university’s core values of community, inclusiveness, integrity and professionalism. The School of Medicine is organised into seven Institutes. All are committed to high quality research-led teaching, through their training of postgraduate research students, delivery of postgraduate taught courses, and its leadership in undergraduate teaching. The School works closely with the local NHS, having a number of jointly funded clinical posts to ensure this relationship is effective and strong for both research and student education. Leeds Institute of Health Sciences (LIHS) Director: Professor Tim Ensor LIHS delivers problem-driven research that supports decisions about the content or delivery of healthcare. Our interdisciplinary approach incorporates expertise in applied health research designs, health implementation sciences, social sciences, health economics, informatics and statistics, as well as skills in communicating with basic scientists, policy makers, healthcare providers, public and patients. We conduct research at the individual, population and organisational level. The Leeds Institute of Cancer And Pathology (LICAP) Director: Professor Tim Bishop The Leeds Institute of Cancer Studies and Pathology addresses both laboratory based and clinical research into cancer with a major focus on translational science. LICAP is one of the largest cancer Institutes in the country and has major financial support from the cancer charities. The laboratories and clinical research are all based on the St James’s site with laboratory activities being located in the Wellcome Trust Brenner Building and adjacent buildings while the clinical work is based within Bexley Wing. The Institute consists of seven Sections with the following interests: Leeds Institute of Genetics Health & Therapeutics (LIGHT), Director: Professor Mark Kearney LIGHT integrates basic and clinical scientists with a common goal of understanding the mechanisms underpinning common chronic diseases of human health and developing new approaches to treating patients at an individual and population level. At the heart of LIGHTs philosophy is a vibrant multidisciplinary approach to science that provides a platform to deliver internationally competitive translational research and teaching in disorders including cardiovascular disease, diabetes, cancer and neurodegenerative diseases) our key aim is to improve the lives of our patients and the experience of our students. Leeds Institute of Medical Education (LIME) Director: Professor Trudie Roberts LIME provides the administrative support, co-ordination and leadership for the School of Medicine’s undergraduate medical degree, including admissions, curriculum development, assessment, student support and clinical placement liaison. It provides the technology-enhanced learning and innovation support for the School of Medicine. LIME also has a very active scholarship programme of research and innovation in medical education and uses its expertise to influence medical education policy and practice nationally and internationally. To achieve this it works with a range of stakeholders including the academic community, the profession, the public, regulators and policy makers. Leeds Institute of Biomedical & Clinical Sciences (LIBACS) Director: Professor Philip Hopkins LIBCS undertakes clinically-driven research from the level of the gene through cellular, tissue and organ to clinical trials. Our vision is to develop a sustainable centre of excellence for the advancement of patient care by translating research results into clinical practise and contributing to medical education at undergraduate and postgraduate levels. Our research interests are encapsulated in 6 clinical themes (Gastrointestinal inflammation & tumorigenesis, Genetic disorders, Infection & immunity, Neuroscience, Perinatal medicine, Perioperative outcomes & technologies) underpinned by 4 generic science technology strands (Animal models, Cell biology, Gene regulations & Genomics). We are based predominantly at the St James’s University Hospital site. Leeds Institute of Rheumatic and Musculoskeletal Medicine (LIRMM), Director: Professor Paul Emery LIRMM is dedicated to improving diagnosis, therapy, intervention and outcome across the spectrum of rheumatic and musculoskeletal medicine. It boasts a dynamic portfolio of research and education, delivering wide-ranging clinical, translational and basic research across five Sections: Clinical Musculoskeletal Medicine, Experimental Musculoskeletal Medicine, Clinical Biomechanics and Physical Medicine, Rehabilitation Medicine and Orthopaedics. A multidisciplinary approach is the core of our activities, with significant interdisciplinary links between Experimental and Clinical research. LIRMM’s clinical activities are focussed at Chapel Allerton Hospital, which is also base for our NIHR Musculoskeletal Biomedical Research Unit (LMBRU) and our basic sciences at St James’s University Hospital. Leeds Institute of Clinical Trials Research (LICTR) Director: Professor Julia Brown LICTR delivers innovative design, delivery and knowledge transfer in clinical trials research. Our multidisciplinary approach, in collaboration with basic scientists, clinicians, policy makers, healthcare providers, public and patients and University colleagues, delivers internationally competitive research and teaching that makes a significant contribution to the evidence base for healthcare delivery. The Institutes research is conducted through the Clinical Trials Research Unit where we have expertise in design and conduct of complex clinical trials incorporating novel designs to evaluate CTIMPs, complex interventions, diagnostics, medical devices and surgery. St James’s University Hospital Campus Infrastructure and Facilities (SCIF) Director: Professor Pam Jones This group covers activities that cover School of Medicine functions for Institutes at St James’s University Hospital that span more than one institute including biomedical research facilities, student education, IT, health and safety, estates, seminars, PGR studentships and business support functions. These functions help support the 5 adjacent buildings on the site. There are 3 Institutes with staff and students at St James’s: LICP (Leeds Institute of Cancer studies and Pathology), LIBACS (Leeds Institute of Biomedical and Clinical Sciences), LIRMM (Leeds Institute of Rheumatic and Musculoskeletal Medicine). These three institutes are dedicated to basic, translational, clinical and health research integrated with student education. Cancer Research UK Centre The Leeds Cancer Research UK Centre (Chair, Professor Alan Melcher) consists of several research areas across Leeds. Specific themes include biologic and viral therapies, radiation biology and therapeutics and genomics with tumour sites of particular interest including brain tumours, colorectal cancer and haematologic malignancies. Leeds is also a Cancer Research UK/NIHR Experimental Cancer Medicine Centre (Lead, Professor Chris Twelves) and hosts an NIHR Clinical Research Facility (Leads, Professor Chris Twelves and Mrs Debbie Beirne). Research income is approximately £10M per annum and the accommodation is principally provided on the St James's University Hospital campus in the Cancer Research Building, Clinical Genetics Building and Cancer Resource and Information Centre but also in the Bexley Wing and at the Leeds General Infirmary. The Cancer Research UK Centre has a wide research portfolio (available on request) and approximately 200 staff. Clinical Trials : There is an active programme of breast cancer clinical trials and early clinical trials, with whom collaboration is encouraged. There are also established links with the Clinical Trials Research Unit (CTRU) led by Prof Julia Brown with Dr Fiona Collinson Deputy Director for Cancer trials; the CTRU also hosts the YCR Early Phase Clinical Trials Programme There are strong links within LICAP (including Professors Andy Hanby and Val Spiers, Drs Tom Hughes and Mihaela Lorger)for translational studies. Additional information Terms and Conditions Details of the terms and conditions of employment for all staff at the university, including information on pensions and benefits, are available on the Human Resources web pages accessible via the links on the right hand side, or at http://hr.leeds.ac.uk/policies University Teaching and Research Award The Senate of the University has agreed that all newly appointed staff with a contract of 0.5 FTE and above who have a teaching/ research role and are deemed new to teaching or research in Higher Education should be required to complete successfully all of the requirements of the University of Leeds Teaching and Research or an appropriate alternative. Whether or not this applies to you, will be decided as part of the appointment procedure at interview. Further details of the ULTRA are available at http://www.sddu.leeds.ac.uk/sddu-ultra.html. Staff with contracts of less than 0.5 FTE may take the ULTRA provided that they have a broad enough range of teaching, research and assessment to complete the requirements of the Programme: this will be decided in conjunction with the School and the course providers. Disclosure and Barring Service Checks A Disclosure and Barring Service (DBS) Check is not required for this position. However, applicants who have unspent convictions must indicate this in the ‘other personal details’ section of the application form and send details to the Recruitment Officer Disabled Applicants The post is located in the Charles Thackrah Building. Disabled applicants wishing to review access to the building are invited to contact the department direct. Additional information may be sought from the Recruitment Officer, email disclosure@leeds.ac.uk or Tel + 44 (0)113 343 1723. Disabled applicants are not obliged to inform employers of their disability but will still be covered by the Equality Act once their disability becomes known. Further information for applicants with disabilities, impairments or health conditions is available in the applicant guidance. Appendix 1 – List of consultant staff, and other medical colleagues the post holder will work with. Current staff and Site Specialisation 18 Medical Oncologists Dr Alan Anthoney Dr Geoff Hall Dr David Jackson Dr Satinder Jagdev GI Cancer / Early Phase Trials / Neuroendocrine (Senior Lecturer) Gynaecological Cancer (Senior Lecturer) Gynaecological Cancer Urology / Renal Dr Maria Marples Melanoma / Sarcoma / Young Adult Dr Clive Mulatero Prof. Tim Perren Lung Cancer / Melanoma Gynaecological Cancer / Breast Cancer Dr Christy Ralph Urological cancer (Clinical Associate Professor) Prof Peter Selby Prof Matt Seymour Sarcoma / Young Adult / Germ Cell Tumours GI Cancer Dr Dan Stark Dr Daniel Swinson Prof Chris Twelves Prof Galina Velikova Dr Fiona Collinson Dr Alison Young Sarcoma / Young Adult / Germ Cell Tumours (Senior Lecturer) GI Cancer / Neuroendocrine Breast Cancer/Early Phase Trials Breast / Quality of Life Research GI cancer (Senior Lecturer) Gynaecological Cancer / Acute Oncology Dr Cath Siller (Locum) Dr Naveen Vasudev Gynaecological cancer / Urological cancer Urological cancer (Clinical Associate Professor) 29 Consultant Clinical Oncologists Dr Julian Adlard Dr David Bottomley Dr Katy Clarke Dr Catherine Coyle Dr Adrian Crellin Dr Rachel Cooper Prof David Dodwell Dr Karen Dyker Dr Kevin Franks Dr George Gerrard Dr Vanessa Gill Dr Paul Hatfield Dr Ann Henry Dr Joji Joseph Dr Sri Kumar Dr Michelle Kwok Williams Prof Susan Short Dr Carmel Loughrey Prof Alan Melcher Dr Jane Orton Breast Cancer and Cancer Genetics Lung, Urological Oncology /Brachytherapy Lung Cancer Head & Neck Oncology / Urological Oncology GI Cancer Gynaecological Oncology / GI Cancer Breast Cancer Paediatric / Head & Neck Cancer Lung and Urological Cancer CNS Oncology / Thyroid Cancer Thyroid and Breast Cancer Brain and GI cancer Urology/Lung Cancer (Clinical Associate Professor) Urology/Breast (Resident York Oncologist) Breast Cancer Paediatric / Lower GI Cancer CNS Oncology Urological / CNS Oncology Melanoma Gynaecological Oncology / Breast Cancer Dr Robin Prestwich Dr Ganesh Radikrishna Prof David Sebag-Montefiore Dr Mehmet Sen Dr Michael Snee Dr Robert Stuart Dr Emma Thomas Dr Robert Turner Head & Neck / Lymphoma GI Cancer GI Cancer Head & Neck Oncology / Breast Cancer Lung Cancer Lung Cancer / Sarcoma Lymphoma / Breast Lung / Urology / Sarcoma Junior Medical Staff There are 19 Clinical Oncology SpRs which includes 2 academic fellows and 3 posts which rotate with Hull. There are 15 Medical Oncology clinical SpRs which includes 7 posts which rotate through Bradford, Huddersfield, York and Hull. There are 18 SHO grade staff for the DMT and 2 staff grades in Non Surgical Oncology. Appendix 2 Oncology Services The Institute of Oncology Clinical Service Unit is one of the large bed-holding Divisions within the Trust. It provides a wide range of secondary and tertiary services, acute and elective, and contains several internationally renowned centres The management of services are devolved to the CSU Management Teams with distinct areas of clinical and financial responsibility. The CSU brings together the core services providing non-surgical oncology services within the Trust and bringing them into a single new £250M specialist Cancer Centre building on the St James's University Hospital site in 2007 aims to improve the quality of care and provide a robust central resource for the Yorkshire Cancer Network (YCN). The DMT has dedicated Finance and Human Resources expertise. The Institute of Oncology CSU includes: Medical Oncology Clinical Oncology Clinical Haematology Bone Marrow Transplantation Palliative Care Medical Physics Breast & endocrine Surgery Thoracic Surgery Gynaecology Oncology Surgery General Manager Head of Nursing Clinical Director Matron Matron Matron Clinical Lead (Clinical Oncology) Clinical Lead (Medical Oncology) Clinical Lead (Palliative Care) Foluke Ajayi Kate Smith David Jackson Sue Dodman Sally Wild Sue Chadwick Professor David Dodwell Dr Daniel Swinson Dr Suzanne Kite Non-Surgical Oncology services Clinical and Medical Oncology services from within the Trust provide comprehensive non-surgical oncology services to the Trust and to the population of West and the majority of North Yorkshire. It is a key component of the Leeds Cancer Centre. There is a hub and spoke arrangement with the surrounding cancer units in Airedale, Bradford, Dewsbury, Halifax, Harrogate, Huddersfield, Pontefract, Wakefield and York. This covers a population of approximately 2.7 million. In addition there are other tertiary referrals from a more extensive catchment area from East Yorkshire, East Lancashire and North Yorkshire. The Clinical and Medical Oncology service currently works from the new St James’s Institute of Oncology Building on the St James's University Hospital site. These two disciplines run as a single bed base and integrated service with site specialist teams. See Appendix 1 for current Staff St James’s Institute of Oncology: In January 2008, oncology services across Leeds were relocated into a new £250M, 63,000m 2 Oncology Wing (the Bexley Wing) on the St James's University Hospital campus. This incorporates services in non-surgical oncology, haematology, the Academic Unit clinical offices and support areas and substantial services in cancer surgery. The St James's Institute of Oncology also a dedicated Cancer Research UK funded facility for patients in complex earlyphase clinical trials. The Bexley Wing, the principal base of the St James’s Institute of Oncology, is one of the largest oncology facilities in the UK, within one of the largest acute general hospitals in Europe. There are 350 beds, day-care and out-patients facilities and a patient hotel. Leeds Cancer Centre The Leeds Cancer Centre provides specialist tertiary services, including medical and clinical oncology, for the treatment of intermediate and rarer cancers within North and West Yorkshire and all cancers from within the city itself. It also provides treatment for common cancers to the local population of 1.2M. The Leeds Cancer Centre Network covers a population of approximately 2.7 million. The Cancer Units surrounding Leeds are evolving into a pattern of linked District General Hospitals. This has occurred through Trust merges and the drive to provide and maintain higher standards of site specialist care for the local population. The consequence of this is the “new” Cancer Units provide services for approximately 450,000 thousand of population. Most of the current Cancer Units already have the concept of resident oncology services in most cases Medical Oncology, complimented with visiting Clinical Oncology. This has allowed the development of some limited in-patient facilities and a higher level of local care for common cancers. They will have primary responsibility for the local resident services in the Units and in some cases take part in Cancer Centre Multi-disciplinary Teams for intermediate cancers and so allow some decentralised chemotherapy for ovarian, upper GI or urological cancers. The need to maintain co-ordinated patterns of care as well as professional links and post-graduate education are fundamental principles. The ability to maintain research and development across the whole network will also be facilitated The Cancer Centre has established a number of clinical groups for each of the key cancer sites/generic issues. Each group is headed by a designated Clinical Lead. The Groups aim to ensure the development of cancer services in accordance with Calman/Hine principles. The Cancer Centre Lead Clinician is Dr Geoff Hall; there is a Cancer Centre manager (Alex Lambert), and data manager (Mr Martin Waugh). A Steering Group has been established involving key clinicians and managers from the Leeds Teaching Hospitals NHS Trust plus Health Authority and primary care representatives. This group provides advice and direction on crucial issues for the development of the Cancer Centre. Outpatient clinics The breast cancer oncology clinics presently running would be available to the Clinical Associate Professor. In addition, the Leeds Clinical Research Facility (OCRF) is an out-patient area comprising recliners, examination room and office space designated for experimental cancer medicine trials. Inpatient facilities In the Bexley Wing there are 94 beds available for oncology patients and two protected research beds.